Oral Microbiota in Mouth-Breathing Patients
Received: 03-Jun-2020 / Accepted Date: 17-Jun-2020 / Published Date: 24-Jun-2020 DOI: 10.4172/2332-0702.1000259
Abstract
Aim: The aim of this study was to evaluate the changes for some bacteria in the oral cavity (Streptococcus Mutans and Lactobacillus Spp.) over time, in mouth-breathing patients (test group) compared to nose-breathing patients (control group).
Materials and methods: 40 patients, homogeneous by age and sex, were evaluated: 20 mouth-breathing patients (Test group) and 20 nose-breathing patients (Control group). The levels of S. Mutans and Lactobacillus Spp., salivary flow, saliva buffer capacity, and plaque index (PI) were assessed. Withdrawals were made at baseline (T0), after 3 months (T1) and after 6 months (T2). All data were compared using the "Student's test" statistical analysis.
Results: The control group has a reduced amount of S. Mutans compared to the test group (G. C. T0=10%, T1=0%, T2=0%) (G. T. T0=0%, T1=5%, T2=35%); while the quantity of Lactobacillus Spp. was different (control group T0=15%, T1=0%, T2=10%, test group T0=0%, T1=5%, T2=35%); Total salivary flows had increased in the control group (T0=47, T1=61, T2=61) compared to the test group, in which it had remained almost constant and lower (T0=44, T1=45, T2=45); Salivary buffering power is unchanged in all controls; Total PI-plaque indices had decreased in nose breathing subjects (T0=3, T1=0, T2=2) compared to mouth-breathing subjects (T0=0, T1=14, T2=27).
Conclusion: Comparing all the data, it can be inferred that mouth breathing predisposes patients to an increase in periodontal disease susceptibility with a noticeable increase in periodontal indices and bacterial colonization.
Keywords: Mouth breathing; Salivary indices; Plaque; Streptococcus mutans; Lactobacillus
Introduction
“ Mouth breather ” we define all the individuals in whom the respiratory function is carried out with the exclusive passage of air through the oral cavity as a result of a pathological adaptation, whether in the presence of nasal and/or pharyngeal obstruction [1-3].
Physiological breathing at rest takes place through the nose with the lips closed effortlessly and the front part of the back of the tongue resting on the palate. Indeed, the primary function of the nose is to humidify, heat and purify from dust and bacteria the air inhaled, before taking it in ideal conditions to the lungs [4].
Chronic breathing through the mouth, in the child, will affect the morphology of the face. It will appear elongated, characterized by a contraction of the maxilla and the base of the nose, with a high palatal vault and a class II malocclusion produced by downward and backward mandibular growth. Respiratory habits acquired during childhood may be responsible for the appearance of habitual oral breathing in adulthood [5,6].
The characteristic appearance in these subjects is commonly called "Adenoid Facies" with gingival smile, dark circles, narrow nostrils and incompetent lips. At the dental level a front open bite and a posterior cross bite are characteristic, resulting in an unsuitable labial seal. Prolonged or continuous exposure of the tissues to the airflow dries the teeth and mucosa, especially in the anterior portion of the mouth, leading to chronic gingival inflammation.
Despite the scarce scientific evidence, the increased prevalence of gingivitis and reduced salivary protection in these patients also suggests an increased susceptibility to dental caries [7]. Bacterial microflora present in the oral cavity contributes to the health of the host and prevents infections by potentially pathogenic exogenous microorganisms, thus providing resistance to colonization by these parasitic species, and by regulating the inflammatory response to the commensal bacteria that are harbored in the buccal cavity [8-11].
Two literature reviews show that there is moderate-to-high evidence that orthodontic appliances are able to significantly influence the concentration of oral microbiota, causing an alteration of the quantity of Streptococcus mutans (S. mutans) and Lactobacilli that can basically affect the process of dental caries and tooth enamel demineralization, due to their acid production and tooth adhesive properties. This statement is confirmed both for removable) and fixed orthodontic appliances [9,12-14].
When the pH, following the intake of fermentable carbohydrates with the diet, remains at low values for a greater amount of time than normal, accumulation of plaque containing acidogenic and acid-tolerable species responsible for carious pathology is favored. The most common are Streptococcus mutans, other acidogenic Streptococcus Spp., Lactobacillus Spp. and bifidobacteria [15-18].
Streptococcus mutans is a Gram-positive bacterium, characterized by the ability to adhere to dental structures and to produce lactic acid from sugars and intra and extracellular polysaccharides is able to resist an acidic environment.
Lactobacilli are mainly responsible for the progression of caries, causing significant damage to dental structures through multiplication and diffusion and are characterized by the production of acid, resist to substances that reduce the bacterial load such as chlorhexidine and acids. Unlike mutant streptococci, they colonize areas of difficult access for cleaning and oral hygiene [19].
It is not surprising that there is a significant correlation between carious lesions and the quantity of lactobacillus in both adults and children [20]. In order to verify the risk of incidence of caries, it is necessary to evaluate not only the presence of Streptococcus mutans but also of Lactobacillus spp. [21].
Materials And Methods
In this study, the levels of Streptococcus Mutans and Lactobacillus Spp. in the saliva of the patients enrolled were evaluated. The stimulated salivary flow, the saliva buffering power and the Silness-Loe plaque index were also analyzed. All data were compared with a group of oral non-respiratory patients (control group). The protocol included a group of twenty oral respiratory patients (test group) and a control group of twenty non-oral respiratory patients (control group).
The two groups were homogeneous by age (10-14 years) and sex. This study was approved by the Clinical Research Ethics Committee (CEIC), following the principles of Helsinki for human experimentation. The salivary samples were analyzed by CRT® bacteria (Ivoclar Vivadent Clinical, Schaan, Liechtenstein). The CRT® bacteria was employed for the bacterial count, as previously published [22,23].
CRT® bacteria was used to determine the S. mutans and Lactobacilli count in saliva by means of selective culture media. The dentist and skilled personnel professionally conduct the test. Findings of 105 CFU or more of Lactobacilli and S. mutans per ml saliva indicate a high caries risk. Leaving the test vial inside an incubator for an additional day or two does not influence the number of CFUs. The preparation of samples and incubation were carried out according to the step-by-step procedure as it was described in its instruction brochure. This test only determines whether or not S. mutans are present in dental saliva [22].
The CRT® bacteria can be considered a comprehensive test, whose main benefits are to determine the caries risk status, to create the basis for target treatment and individualized check-up intervals for the long-term maintenance of oral health. This chair-side method is highly specific and sensitive for S. mutans and its only limitation is that at least 48 hours are require for detection of S. mutans [23].
The samples were taken at the beginning of the observation (T0), after three months (T1) and at six months from the beginning of the observation (T2). All patients had previously been motivated to home oral hygiene [14,24-27]. Patients should not have eaten, drunk, smoked, or brushed their teeth for at least an hour before the visit, as all these actions could alter the salivary flow.
Each patient was given a paraffin tablet to be chewed for 30 seconds to stimulate the saliva, which was then eliminated. The paraffin tablet was then chewed again for 5 minutes, and the saliva gradually produced was collected in a graduated glass tube. By means of this procedure, the quantity (ml) of saliva collected in the defined period of time and the salivary flow (the amount of saliva produced during the same period) were recorded [28,29].
• The saliva buffering capacity was calculated using the CRT® buffer, and evaluated at three values: low, medium or high.
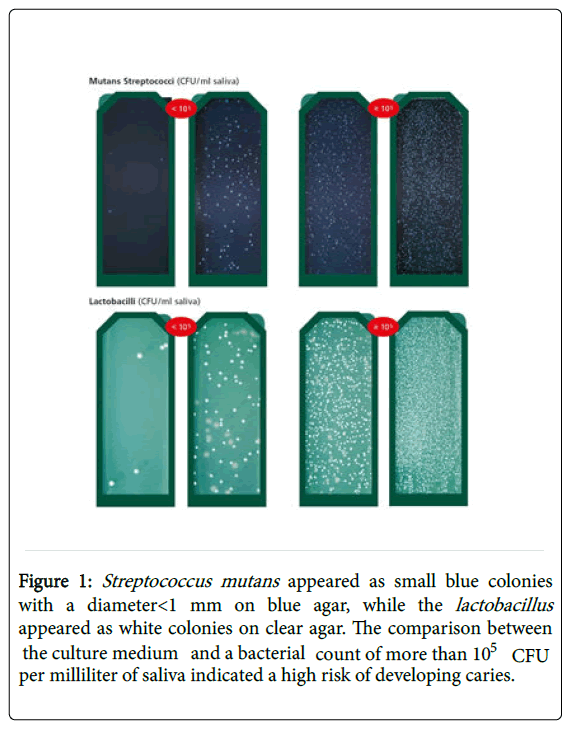
• The CRT® bacteria test was used to count the Lactobacillus spp. and Streptococcus mutans in the following way: from the graduated glass, previously filled by the patient, a sufficient quantity of saliva was collected using pipettes (1 ml) to completely wet the culture medium (agar). A tablet of NaHCO3 was placed in the container of the culture medium; this procedure was necessary to stimulate bacterial growth. The container was placed in an incubator at 35°C-37°C for 48 hours. Evaluation of the results was carried out is shown in Figure 1.
Figure 1: Streptococcus mutans appeared as small blue colonies with a diameter<1 mm on blue agar, while the lactobacillus appeared as white colonies on clear agar. The comparison between the culture medium and a bacterial count of more than 105 CFU per milliliter of saliva indicated a high risk of developing caries.
Results
The No significant differences were found between the samples of the two groups at T0 in Table 1 distribution of the values at T0 of the two groups. No significant differences were found between the samples of the two groups at T0. (For the plaque index, the scores are 0, 1, 2, 3; For salivary flow: 1 ≤ 1; 2=1<x<1, 5; 3=1, 5<x<1. 75; 4=1. 75<x<2; 5=2<x<2. 5; 6>2. 5; For the buffering power of saliva: 1=low; 2=medium-low; 3=medium ; 4=medium-high; 5=high).
| Variables | Control group | Test group |
|---|---|---|
| Age | 13 years | 12-14 years |
| PI (T0) | 0 | 0 |
| Salivary flow (sum of values) | 47 | 44 |
| Buffering power of saliva | Medium | Medium |
Table 1: Distribution of the values at T0 of the two groups.
Total PI-Plaque indices had decreased in nose breathing subjects (T0=3, T1=0, T2=2) compared to mouth-breathing subjects (T0=0, T1=14, T2=27) in Table 2 total Plaque indices (PI) and the comparison of the two groups according to Student’s t-test. It can be seen that the total plaque indices are much lower at T1 and T2 in the control group compared to the test group. In mouth-breathing patients there is a progressive increase of the plaque index over time.
| Variables | PI (T0) | PI (T1) | PI (T2) | T0 vs. T1 | T0 vs. T2 | T1 vs. T2 |
|---|---|---|---|---|---|---|
| Control Group | 3 | 0 | 2 | 0, 082814 | 0, 643017 | 0, 16255 |
| Test Group | 0 | 14 | 27 | 2, 7516 × 10-5 | 1, 61997 × 10-10 | 0, 000431873 |
| Control Group vs. Test Group | 0, 082814 | 2, 7516 × 10-5 | 5, 1249 × 10-11 | |||
Table 2: Total Plaque indices (PI) and the comparison of the two groups according to Student’s t-test.
The buffering power of saliva was unchanged in both groups over time in Table 3 (we see how the average buffering power of the saliva does not change over time).
| Average buffering power | T0 | T1 | T2 |
|---|---|---|---|
| Test Group | 3 | 3 | 3 |
| Control Group | 3 | 3 | 3 |
Table 3: Average buffering power.
Total salivary flows had increased in the control group (T0=47, T1=61, T2=61) compared to the test group, in which it had remained almost constant and lower (T0=44, T1=45, T2=45) in Table 4 total salivary flows (SF) and the comparison of the two groups according to the Student’s t-test. It can be noted that the total salary flow is greater at T1 and T2 in the Control Group compared to the Test Group. In the latter, the salivary flow remained almost constant.
| Variables | SF (T0) | SF (T1) | SF (T2) | T0 vs. T1 | T0 vs. T2 | T1 vs. T2 |
|---|---|---|---|---|---|---|
| Control Group | 47 | 61 | 61 | 0, 215774 | 0, 215774 | 1 |
| Test Group | 44 | 45 | 45 | 0, 909746 | 0, 909746 | 1 |
| Control Group vs. Test Group | 0, 769123 | 0, 113993 | 0, 113993 | |||
Table 4: Total salivary flows (SF) and the comparison of the two groups according to the Student’s t-test.
The control group showed a lower percentage of patients who had a quantity of S. mutans able to cause carious pathology (T0=10%, T1=0%, T2=0%) compared to the Test group (T0=0%, T1=5%, T2=35%) in Table 5 percentage of patients with Streptococcus mutans>105 CFU and the comparison of the two groups according to the “Student’s t function”. The quantity of bacteria decreases with time in the control group compared to the test group, where instead a progressive increase of the bacterial colonies can be observed over time.
| %of Patients with S. Mutans>105 CFU | T0 | T1 | T2 | T0 vs. T1 | T0 vs. T2 | T1 vs. T2 |
|---|---|---|---|---|---|---|
| Control Group | 10% | 0% | 0% | 0, 16255 | 0, 16255 | 0 |
| Test Group | 0% | 5% | 35% | 0, 329877 | 0, 004729 | 0, 019172 |
| Control Group vs. Test Group | 0, 16255 | 0, 3298768 | 0, 00472946 |
Table 5: Percentage of patients with Streptococcus mutans >105 CFU and the comparison of the two groups according to the "Student’s t function”.
While the quantity of Lactobacillus spp. was different (control group T0=15%, T1=0%, T2=10%, test group T0=0%, T1=5%, T2=35%) in Table 6 percentage of patients with Lactobacillus>105 CFU and the comparison of the two groups according to the “Student’s t function”. In this case, the amount of bacteria in the control group decreases at T1 (after three months) but increases at T2 (after six months). In any case, the percentage values of the Control Group are lower than the values of the Test Group, in which the amount of bacteria increases with time.
| % of Patients With Lactobacillus>105 CFU | T0 | T1 | T2 | T0 vs. T1 | T0 vs. T2 | T1 vs. T2 |
|---|---|---|---|---|---|---|
| Control Group | 15% | 0% | 10% | 0, 082814 | 0, 643017 | 0, 16255 |
| Test Group | 0% | 5% | 35% | 0, 329877 | 0, 004729 | 0, 019172 |
| Control Group vs. Test Group | 0, 082814 | 0, 329877 | 0, 062005 |
Table 6: Percentage of patients with Lactobacillus >105 CFU and the comparison of the two groups according to the "Student’s t" function.
Discussion
Mouth breathing is a stable and pathological alteration of the normal breathing pattern [30], common among children of school age [31], and is often accompanied by morphological alterations in the normal growth pattern of the face and various harmful effects on physiological health [32].
If protracted in time, such alteration may have detrimental effects on gingival health in the presence of dental plaque [33].
Saliva has an important role in controlling oral microflora, because of its mechanical washing and antimicrobial properties. In mouth breathers, the protective role of saliva is diminished in the air-exposed teeth and gingival areas in the anterior maxillary region, resulting in a higher incidence of gingivitis [7].
The aim of this study was to evaluate the microbial colonization in the oral cavity in mouth-breathing patients and to compare the results with a non-oral respiratory control group, homogeneous for sex and age.
We evaluated also the Plaque Index and collected the total stimulated saliva to estimate the salivary flow and its buffering capacity in order to understand how they affect bacterial colonization over time.
Observing the trend of the Sillness-Loe Plaque Index over time, it can be seen how the amount of plaque at T1 (after three months) and T2 (after six months) of the Control Group decreases in comparison with the Test Group, in accordance with international literature [34-41].
Other research states that in caries-free children a quantity of Streptococcus mutans<105 CFU is present. Therefore, for the microbial counts, this value indicated the cut-off of reference for our observations [42].
A different tendency in bacterial colonization was observed in the two groups analyzed in our study. In the control group, where at T0 10% of patients had a quantity of CFU>105, there was a total decrease in the levels of Streptococcus mutans at T1 and T2 (0%). A different situation was observed in the Test Group, in which the number of patients who had a CFU>105, at T0 was zero, 5% at T1, reaching as high as 35% at T2.
Similarly plaque indices had decreased, explained by the presence of a higher salivary flow in non-oral respiratory patients than in mouth-breathing patients.
Moreover, from these data, it can be seen that the levels of Streptococcus mutans at the beginning of the observation are not predictive of future bacterial colonization, neither is the amount of plaque, as over time both the microbial counts and the amount of plaque decreased in non-oral respiratory patients.
This is due to the fact that the presence of oral breathing alters the balance between salivary flow and bacterial colonization in the oral cavity, in favor of the latter [41,42]. The degree to which the lips cover the upper teeth influences dental plaque accumulation and gingivitis, as in the presence of incompetent lips, since the front part of the gingiva is not bathed by saliva, and therefore receives less benefit from its protective and cleansing actions [43-46].
Oral hygiene invariably has an important role to play [47,48].
With regard to the Lactobacillus spp., a different trend was observed in the control group: at the beginning of the treatment (T0) 15% of patients had a bacterial count>105, CFU, a figure which decreased to 0% at T1 but increased after six months to 10%.
Among the various hypotheses which may explain this phenomenon is the fact that, as stated before, the Lactobacillus spp. are much more resistant and acid-tolerant than Streptococcus mutans, colonize areas of difficult access, and are not eliminated by substances such as chlorhexidine [49,50].
Conclusion
By analyzing the data obtained we can conclude, with the limitations due to the reduced number of samples that oral breathing does not help the patient to maintain a sufficient level of oral hygiene, understood as oral microbial flora due to a decrease in salivary flow which leads to a decrease in the host's defenses. The increase in the microbial flora of the oral cavity, attributable to the two previous points, implies a significant increase in the bacterial colonization of S. mutans and Lactobacillus spp.
Our deductions, obtained from the critical analysis of the data collected and summarized in the tables, confirm what was stated in the literature that "the presence of mouth breathing is actually an aggravating factor in the state of oral health in patients with this problem".
The presence of oral respiration conditions the microbiological balance in the oral cavity and causes a decrease in salivary flow, with a consequent increase in plaque and bacteria responsible for inflammatory insult in periodontal tissues.
The results of our study seem to indicate that a correct treatment of the dento-periodontal problems related to the presence of respiratory defects in both pediatric and adult patients, naturally preceded by early interception and diagnosis of such disorders, is able to provide a valid contribution to improving patients’ health.
It can be considered of fundamental importance that the Dentist intercepts early on the morphofunctional alterations of the craniofacial district as the possible cause of respiratory disorders and consequent chain of related pathologies, and that she/he be ready to intervene in the alteration of the oral cavity connected to them, also by educating and motivating her/his patients.
References
- Valeriani F, Protano C, Gianfranceschi G, Cozza P, Campanella V, et al. (2016) Infection control in healthcare settings: Perspectives for mfDNA analysis in monitoring sanitation procedures. BMC Infect Dis 16: 394.
- Di Francesco RC (2017) Respirador oral semobstáculo das viasaéreassuperiores. Obstrução nasal-o direito de respirarpelonariz. Rio de Janeiro: Atheneu 2: 69.
- Campanella V, Syed J, Santacroce L, Saini R, Ballini A, et al. (2018) Oral probiotics influence oral and respiratory tract infections in pediatric population: A randomized double-blinded placebo-controlled pilot study. Eur Rev Med Pharmacol Sci 22: 8034-8041.
- Valera FC, Anselmo-Lima WT, Tamashiro E (2017) A criaņcarespiradoraoral. In: SoleÌ D, Prado E, Weckx LL (eds) Obstru̧cãonasal - o direito de respirarpelonariz. Rio de Janeiro: Atheneu 2: 31.
- Sano M, Sano S, Kato H, Arakawa K, Arai M (2018) Proposal for a screening questionnaire for detecting habitual mouth breathing, based on a mouth-breathing habit score. BMC Oral Health 18: 216.
- Quinzi V, Scibetta ET, Marchetti E, Mummolo S, Gianni AB, et al. (2018) Analyze my face. J Biol RegulHomeost Agents 32: 149-158.
- NascimentoFilho E, Mayer MP, Pontes P, Pignatari AC, Weckx LL, et al. (2004) Caries prevalence, levels of mutans streptococci, and gingival and plaque indices in 3. 0-to 5. 0-year-old mouth breathing children. Caries Res 38: 572-575.
- Marsh PD (2010) Controlling the oral biofilm with antimicrobials. J Dent 38: S11-S15.
- Mummolo S, Tieri M, Tecco S, Mattei A, Albani F, et al. (2014) Clinical evaluation of salivary indices and levels of Streptococcus mutans and Lactobacillus. Eur J Paediatr Dent 15: 367-370.
- Mummolo S, Nota A, Albani F, Marchetti E, Gatto R, et al. (2020) Salivary levels of Streptococcus mutans and Lactobacilli and other salivary indices in patients wearing clear aligners versus fixed orthodontic appliances: An observational study. Plos One 15: e0228798.
- Mummolo S, Tieri M, Nota A, Caruso S, Darvizeh A, et al. (2020) Salivary concentrations of Streptococcus mutans and Lactobacilli during an orthodontic treatment. An observational study comparing fixed and removable orthodontic appliances. Clin Exp Dent Res 6: 181-187.
- Lucchese A, Bondemark L, Marcolina M, Manuelli M (2018) Changes in oral microbiota due to orthodontic appliances: A systematic review. J Oral Microbiol 10: 1476645.
- Quinzi V, Ferro R, Rizzo FA, Marranzini EM, Canova FF, et al. (2018) The Two by Four appliance: A nationwide cross-sectional survey. Eur J Paediatr Dent 19: 145-150.
- Pennazza G, Marchetti E, Santonico M, Mantini G, Mummolo S, et al. (2008) Application of a quartz microbalance based gas sensor array for the study of halitosis. J Breath Res 2: 017009.
- Socransky SS, Haffajee AD, Cugini MA, Smith C, Kent Jr RL (1998) Microbial complexes in subgingival plaque. J Clin Periodontol 25: 134-144.
- Libonati A, Taranto DV, Mea A, Montemurro E, Gallusi G, et al. (2019) Clinical antibacterial effectiveness Healozone Technology after incomplete caries removal. Eur J Paediatr Dent 20: 73-78.
- Libonati A, Montemurro E, Nardi R, Campanella V (2018) Percentage of Gutta-percha–filled Areas in Canals Obturated by 3 Different Techniques with and without the Use of Endodontic Sealer. J Endod 44: 506-509.
- Libonati A, Di VT, Santoro MM, Di DC, Ombres D, et al. (2018) Comparison of coronal leakage of different root canal filling techniques: an ex vivo study. J Biol RegulHomeost Agents 32: 397-405.
- Featherstone JD (2000) The science and practice of caries prevention. J Am Dent Assoc 31: 887-899.
- Hardie JM, Thomson PL, South RJ, Marsh PD, Bowden GH, et al. (1977) A longitudinal epidemiological study on dental plaque and the development of dental caries—interim results after two years. J Dent Res 56: 90-98.
- Loesche WJ (1986) Role of Streptococcus mutans in human dental decay. Microbiol Rev 50: 353-380.
- Mummolo S, Nota A, Caruso S, Quinzi V, Marchetti E, et al. (2018) Salivary markers and microbial flora in mouth breathing late adolescents. BioMed Res Int
- Freitas AO, Marquezan M, Nojima MD, Alviano DS, Maia LC (2014) The influence of orthodontic fixed appliances on the oral microbiota: a systematic review. Dental Press J Orthod 19: 46-55.
- Marchetti E, Mummulo S, Marzo G, Civisca A, Di Pietro C, et al. (2009) Effect of an essential-oil containing mouthrinse on the reduction of plaque and interproximal inflammation in comparison with an ethanol solution. Prev Assist Dent 35: 123-127.
- Bernardi S, Zeka K, Mummolo S, Marzo G, Continenza MA (2013) Development of a new protocol: a macroscopic study of the tongue dorsal surface. Italian J Anatomy Embryol 118: 1.
- Mummolo S, Marchetti E, Giuca MR, Gallusi G, Tecco S, et al. (2013) In-office bacteria test for a microbial monitoring during the conventional and self-ligating orthodontic treatment. Head Face Med 9: 7.
- Sánchez-GarcÃa S, Gutiérrez-Venegas G, Juárez-Cedillo T, Reyes-Morales H, Solórzano-Santos F, et al. (2008) A simplified caries risk test in stimulated saliva from elderly patients. Gerodontology 25: 26-33.
- Isola G, Polizzi A, Alibrandi A, Indelicato F, Ferlito S (2020) Analysis of Endothelin-1 concentrations in individuals with periodontitis. Scient Rep 10: 1-8.
- Isola G, Alibrandi A, Rapisarda E, Matarese G, Williams RC, et al. (2020) Association of vitamin D in patients with periodontitis: A cross-sectional study. J Periodontal Res
- Favero L, Arreghini A, Cocilovo F, Favero V (2013) Respiratory disorders in paediatric age: orthodontic diagnosis and treatment in dysmetabolic obese children and allergic slim children. Eur J Paediatr Dent 14: 190-194.
- Garde JB, Suryavanshi RK, Jawale BA, Deshmukh V, Dadhe DP, et al. (2014) An epidemiological study to know the prevalence of deleterious oral habits among 6 to 12 year old children. J Int Oral Health 6: 39-43.
- Jefferson Y (2010) Mouth breathing: adverse effects on facial growth, health, academics, and behavior. Gen Dent 58: 18-25.
- Bhatia A, Sharma RK, Tewari S, Narula SC (2015) A randomized clinical trial of salivary substitute as an adjunct to scaling and root planing for management of periodontal inflammation in mouth breathing patients. J Oral Sci 57: 241-247.
- Giuca MR, Pasini M, Tecco S, Marchetti E, Giannotti L, et al. (2012) Skeletal maturation in obese patients. Am J orthod Dentofacial Orthop 142: 774-779.
- Lin JJ, Cameron SM, Runyan DA, Craft DW (1999) Disinfection of denture base acrylic resin. J Prosthet Dent 81: 202-206.
- Sukontapatipark W, El-Agroudi MA, Selliseth NJ, Thunold K, Selvig KA (2001) Bacterial colonization associated with fixed orthodontic appliances. A scanning electron microscopy study. Eur J Orthod 23: 475-484.
- Arendorf T, Addy M (1985) Candidal carriage and plaque distribution before, during and after removable orthodontic appliance therapy. J Clin Periodontol 12: 360-368.
- Chang HS, Walsh LJ, Freer TJ (1999) The effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of mutans streptococci and lacto bacilli. Aust Orthod J 15: 229-334.
- Peros K, Mestrovic S, Anic-Milosevic S, Slaj M (2011) Salivary microbial and nonmicrobial parameters in children with fixed orthodontic appliances. Angle Orthod 81: 901-906.
- Moritsuka M, Kitasako Y, Burrow MF, Ikeda M, Tagami J, et al. (2006) Quantitative assessment for stimulated saliva flow rate and buffering capacity in relation to different ages. J Dent 34: 716-720.
- Li Y, Hu B, Liu Y, Ding G, Zhang C, et al. (2009) The effects of fixed orthodontic appliances on saliva flow rate and saliva electrolyte concentrations. J Oral Rehabil 36: 781-785.
- Krasse B (1988) Biological factors as indicators of future caries. Int Dent J38: 219-225.
- Mummolo S, Marchetti E, Albani F, Campanella V, Pugliese F, et al. (2014) Comparison between rapid and slow palatal expansion: evaluation of selected periodontal indices. Head Face Med 10: 30.
- Mummolo S, Nota A, De Felice ME, Marcattili D, et al. (2018) Periodontal status of buccally and palatally impacted maxillary canines after surgical-orthodontic treatment with open technique. J Oral Sci 60: 552-556.
- Addy M, Dummer PM, Hunter ML, Kingdon A, Shaw WC (1987) A study of the association of fraenal attachment, lip coverage, and vestibular depth with plaque and gingivitis. J Periodontol 58: 752-757.
- Gulati MS, Grewal N, Kaur A (1998) A comparative study of effects of mouth breathing and normal breathing on gingival health in children. J Indian Soc Pedod Prev Dent 16: 72-83.
- Peixoto IT, Enoki C, Ito IY, Matsumoto MA, Nelson-Filho P (2011) Evaluation of home disinfection protocols for acrylic baseplates of removable orthodontic appliances: A randomized clinical investigation. Am J Orthod Dento facial Orthop 140: 51-57.
- QuiveyJr RG, Kuhnert WL, Hahn K (2001) Genetics of acid adaptation in oral streptococci. Crit Rev Oral Biol Med 12: 301-314.
- Cotter PD, Hill C (2003) Surviving the acid test: responses of gram-positive bacteria to low pH. Microbiol Mol Biol Rev 67: 429-453.
- Svensäter G, Borgström M, Bowden GH, Edwardsson S (2003) The acid-tolerant microbiota associated with plaque from initial caries and healthy tooth surfaces. Caries Res 37: 395-403.
Citation: Mummolo S, Quinzi V, Dedola A, Albani F, Marzo G, Campanella V (2020) Oral Microbiota in Mouth-Breathing Patients. J Oral Hyg Health 8: 259. DOI: 10.4172/2332-0702.1000259
Copyright: © 2020 Mummolo S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3977
- [From(publication date): 0-2020 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 3113
- PDF downloads: 864