Research Article Open Access
Optimal Timing of Pre-operative Endoscopic Clipping for Determining the Resection Line for Laparoscopy-assisted Distal Gastrectomy: Experience with 92 Gastrectomies for Early Gastric Cancer
Won Chang Shin*, Ji Young Park, Tae Joo Jeon, Tae Hwan Ha, Mi Jin Ryu, Ye na Choi, Seung Suk Baek, Gi Jun Jang, Tae-Hoon Oh and Won-Choong Choi
Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Republic of Korea
- *Corresponding Author:
- Won Chang Shin
Assistant professor, Division of Gastroenterology
Department of Internal Medicine, Sanggye Paik Hospital
Inje University College of Medicine, Republic of Korea
Tel: 82-10-7104-6227
E-mail: human0016@gmail.com
Received date: February 19, 2014; Accepted date: March 20, 2014; Published date: March 26, 2014
Citation: Shin WC, Park JY, Jeon TJ, Ha TH, Ryu MJ, et al. (2014) Optimal Timing of Pre-operative Endoscopic Clipping for Determining the Resection Line for Laparoscopy-assisted Distal Gastrectomy: Experience with 92 Gastrectomies for Early Gastric Cancer. J Gastroint Dig Syst 4:179. doi: 10.4172/2161-069X.1000179
Copyright: © 2014 Shin WC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Objective: Pre-operative endoscopic clipping for determining the resection line in patients with early gastric cancer (EGC) has been used safely, and its efficacy has been demonstrated. However, the optimal timing of endoscopic clipping for determining the resection line in EGC patients undergoing laparoscopy-assisted distal gastrectomy (LADG) has not been investigated.
Methods: A retrospective analysis of 92 patients with EGC who underwent gastric resection after endoscopic clipping at OOO Hospital, Korea was performed. We analyzed the clinical and endoscopic features of patients, number of clips, time from clipping to surgery, and number of patients showing detachment of clips from the gastric wall before surgery. Patients were categorized into the following 2 groups: group A included patients whose clips were applied within 1 day before surgery and group B included patients whose clips were applied more than 1 day before surgery.
Results: Of the 92 patients, 56 were in group A and 36 were in group B. In 11 patients (12.0%, 5 in group A and 6 in group B, P=0.329), the clips were detached from the gastric wall before surgery. The mean time from clipping to surgery did not differ significantly between the detached and non-detached groups (11 patients, mean 4.6 ± 4.6 days vs. 81 patients, mean 3.0 ± 4.0 days, P = 0.227).
Conclusion: The timing of endoscopic clipping for the localization of tumors in EGC patients undergoing gastrectomy is not important for determining the resection line.
Keywords
Endoscopic clipping; Laparoscopy-assisted distal gastrectomy; Early gastric cancer; Resection margin; Pre-operative clipping
Introduction
The expanded use of diagnostic endoscopy has increased the detection rate of early gastric cancer (EGC) [1]. The therapeutic option for EGC is gastric resection with an adequate resection margin and perigastric lymph node dissection [1-3]. However, EGC cannot be detected by inspection of the serosal surface in the operative field, and it is generally not manually palpable because of its shallow invasion depth [1,2,4,5]
Endoscopic mucosal clipping was developed for hemostasis of gastrointestinal bleeding, but it is now widely used for other purposes, for example, as a marker for radiotherapy and for closing gastrointestinal perforations [2,6,7]. Some studies have demonstrated the value of endoscopic clipping of the proximal region outside the lesion for selecting the appropriate surgical procedure and determining the resection line for tumors located in the middle corpus or more distal portions of the stomach [2,8,9]. This technique is safe, cost-effective, and easily performed. Furthermore, the clips are not easily detached and remain firmly in place for several days [1,2]. However, the optimal timing of pre-operative endoscopic clipping for determining the resection line has not been investigated. In the present study, we evaluated the optimal timing of endoscopic clipping for determining the resection line in patients with EGC undergoing laparoscopy-assisted distal gastrectomy (LADG).
Materials and Methods
Between January 2010 and December 2012, we performed a retrospective analysis of partial gastrectomies after endoscopic clipping for the localization of EGC. A total of 92 patients with EGC who had undergone gastric resection after endoscopic clipping at OOO Hospital, Korea were enrolled in the study. Pre-operative endoscopic clipping was performed to determine the proximal resection line by identifying the exact site of the tumor in patients undergoing LADG. All data were retrospectively reviewed. The clinical and endoscopic features of all patients, number of clips, time from clipping to surgery, and number of patients whose clips were detached from the gastric wall before surgery were analyzed. The detachment of clips was detected by plain radiographic images obtained before surgery. Patients were categorized into the following 2 groups: group A included patients whose clips were applied within 1 day before surgery and group B included those whose clips were applied more than 1 day before surgery.
Endoscopic clipping
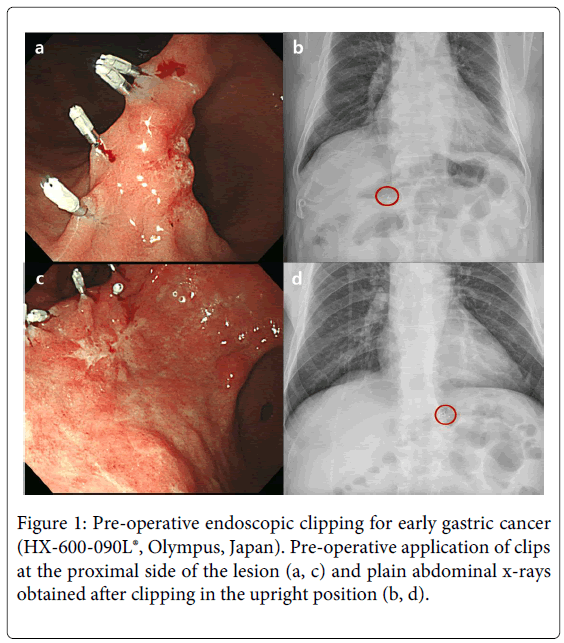
Before the operation (mean, 3.1 days; range, 0-18 days), several endoscopic clips (HX-600-090L, Olympus, Japan) were placed at proximal sites outside the lesion to determine the resection line through a flexible endoscope using a roticulator clip-fixing device (HX-5QR-L, Olympus). The procedure was performed separately by 3 endoscopists with extensive experience (>700 gastroscopies per year for a period of more than 10 years). The clips were 8 mm in length and 2 mm in diameter. After application of the clips, patients were evaluated by plain radiography of the chest and abdomen before surgery to obtain general information on the location of the lesion and attachment of the clips to the gastric wall
(Figure 1).
Statistical analysis
The chi-square and Fischer’s exact tests were used to compare categorical data. All continuous data values were expressed as mean ± SD (standard deviation). Differences in the mean values were examined by Student’s t-test. The significance level was set at a P value of less than 0.05. All statistical calculations were performed with SAS 8.1 (Cary, NC).
Results
The clinical and endoscopic characteristics of all patients are summarized in Table 1. All the applied endoscopic clips were easily detected by plain radiography as radiopaque materials. Of the 92 patients, 56 were included in group A and 36 in group B. A total of 287 clips were used, with 2-4 clips per patient (mean, 3.1 clips/patient; range 1-5 clips/patient). Detachment of clips from the gastric wall before surgery was observed in 11 patients (12.0%, 5 in group A, 6 in group B). Age, tumor location, number of clips applied, and number of patients showing detachment of clips from the gastric wall before surgery did not differ significantly between the 2 groups (P > 0.05).
| Group A (≤ 1 day, n=56) | Group B (>1 day, n=36) | |
|---|---|---|
| Age (years, mean ±SD) | 61.8 ± 10.4 | 61.3 ± 10.7 |
| Sex (M:F) | 43 (76.8%):13 (23.2%) | 19 (52.8%):17(47.2%) |
| Location | ||
| antrum | 31 (55.4%) | 13 (36.1%) |
| angle | 11 (19.6%) | 8 (22.2%) |
| lowerbody | 11 (19.6%) | 13 (36.1%) |
| middlebody | 3 (5.4%) | 2 (5.6%) |
| No. of clips (mean ± SD) | 3.1 ± 0.8 | 3.1 ± 1.0 |
| Loss of clips (No. of patients) | 5 (8.9%) | 6 (16.7%) |
SD: standarddeviation, M: male, F: female, No.: number * P < 0.05
Table 1: Clinical and endoscopic features of the 92 patients who underwent endoscopic clipping for early gastric cancer.
The clinical and endoscopic features of the 11 patients showing detachment of clips applied before surgery for determining the resection line are presented in Table 2. One clip was lost in 9 patients and 2 clips were lost in 2 patients. The mean time from clipping to surgery did not differ significantly between the detached and non-detached groups (mean, 4.6 ± 4.6 days [n = 11] vs. mean, 3.0 ± 4.0 days [n = 81], P = 0.227).
| Detached (n=11, 12.0%) | Non-detached (n=81, 88.0%) | P value* | |
|---|---|---|---|
| Age (year, mean ±SD) | 65.4 ± 9.0 | 61.1 ± 10.6 | 0.202 |
| Sex (M:F) | 8 (72.7%):3 (27.3%) | 54 (66.7%):27 (33.3%) | 0.687 |
| Location | 0.187 | ||
| antrum | 8 (72.7%) | 36 (44.4%) | |
| angle | 0 (0%) | 19 (23.5%) | |
| lower body | 2 (18.2%) | 22 (27.2%) | |
| middle body | 1 (9.1%) | 4 (4.9%) | |
| No. of clips (mean ± SD) | 3.1 ± 0.8 | 3.0 ± 1.1 | 0.632 |
| Time-to-surgery (day, mean ± SD) | 4.6 ± 4.6 | 3.0 ± 4.0 | 0.227 |
SD: standard deviation, M: male, F: female, No.: number *P < 0.05
Table 2: Clinical and endoscopic features of 11 patients who showed detachment of clips applied for determining the resection line before surgery
Discussion
Many studies have reported that EGC is associated with a favorable prognosis; therefore, improving the quality of life of patients with EGC remains the primary therapeutic objective [1,4,10]. LADG has many advantages over open distal gastrectomy, such as less pain, smaller wounds, fewer respiratory complications, a shorter hospital stay, better quality of life postoperatively, and an earlier return to normal activity [10,11]. The success of LADG depends on the precise determination of the tumor site [1,5,12]. As accurate localization of the tumor is sometimes difficult, specific techniques are necessary to define an adequate gastric resection range, especially in patients undergoing laparoscopy-assisted gastrectomy [1,2]. Several studies have shown that endoscopic clipping is a safe and reliable procedure for determining the resection line in tumors located in the stomach, and this technique has been widely used for this purpose [1,2]. However, the optimal timing of pre-operative endoscopic clipping for determining the resection line has not been analyzed, and in our institution, clipping has been routinely performed 1 day before surgery without definitive reference.
In the present study, the number of patients showing detachment of clips from the gastric wall before surgery did not differ significantly between groups A and B (5 patients vs. 6 patients, P=0.329). Furthermore, the mean time from clipping to surgery was not significantly different between the detached and non-detached groups. Similarly, there were no significant differences in tumor location (P = 0.187) and number of clips (P = 0.632) between the detached and non-detached groups. These results suggest that the timing of the clipping procedure was not important for localizing tumors in EGC patients.
None of the patients included in the study lost more than 3 clips, with 9 patients losing 1 clip and 2 patients losing 2 clips. This result indicates that more than 3 clips should be applied for the localization of lesions, although large-scale prospective randomized controlled studies are needed to prove this result. The exact period of exposure to the clips tolerated by patients cannot be determined from our results. However, clips remained in place for > 7 days in 16 cases, and the longest duration was 18 days in 2 cases. The suggestion of an optimal or tolerable duration requires further studies.
The main limitations of our study are inherent to its retrospective study design. All data were collected retrospectively, and data were not adjusted for age and sex. In addition, the distances between the specimen, tumor margin, and depth of clipping were not determined after the gastrectomy. Therefore, adequate placing of endoscopic clips could not be assessed. Furthermore, assessment of clip detachment was performed by plain radiography instead of the analysis of specimens after gastrectomy because specimens could not be obtained at the beginning of our study. The possible overlapping of clips may have been missed in radiographic images, and this could have affected our results. Despite these limitations, the present study is important, as it is the first to evaluate the optimal timing of endoscopic clipping for determining the resection line for LADG in patients with EGC.
In conclusion, the results of the present study showed that the timing of clipping for the localization of tumors in EGC patients undergoing gastrectomy is not important. Further large-scale prospective randomized controlled studies are needed to confirm these findings.
References
- Hyung W, Lim J, Cheong J, Kim J, Choi S, et al. (2005) Intraoperative tumor localization using laparoscopic ultrasonography in laparoscopic–assisted gastrectomy. Surgical Endoscopy And Other Interventional Techniques 19: 1353-1357.
- Ryu KW, Lee JH, Choi IJ, Bae JM (2003) Preoperative endoscopic clipping: localizing technique of early gastric cancer. J SurgOncol 82: 75-77.
- Bozzetti F, Marubini E, Bonfanti G, Miceli R, Piano C, et al. (1999) Subtotal versus total gastrectomy for gastric cancer: five-year survival rates in a multicenter randomized Italian trial. Italian Gastrointestinal Tumor Study Group. Ann Surg 230: 170-178.
- Kikuchi S, Hirai K, Kuroyama S, Katada N, Sakuramoto S, et al. (2004) Role of endoscopic clipping for determining the resection line for tumors located in the middle or upper corpus of the stomach: experience with 100 gastrectomies for early gastric cancer. Anticancer Res 24: 4163-4168.
- Beretvas RI, Ponsky J (2001) Endoscopic marking: an adjunct to laparoscopic gastrointestinal surgery. SurgEndosc 15: 1202-1203.
- Cipolletta L, Bianco MA, Rotondano G, Marmo R, Piscopo R, et al. (2000) Endoscopic clipping of perforation following pneumatic dilation of esophagojejunal anastomotic strictures. Endoscopy 32: 720-722.
- Weyman RL, Rao SS (1999) A novel clinical application for endoscopic mucosal clipping. GastrointestEndosc 49: 522-524.
- Kuwano H, Sadanaga N, Watanabe M, Ikebe M, Mori M, et al. (1995) Preoperative endoscopic clipping for determining the resection line in early carcinoma of the esophagus. J Am CollSurg 180: 97-99.
- Okabayashi T, Gotoda T, Kondo H, Ono H, Oda I, et al. (2000) Usefulness of indigo carmine chromoendoscopy and endoscopic clipping for accurate preoperative assessment of proximal gastric cancer. Endoscopy 32: S62.
- Lee SE, Kim YW, Lee JH, Ryu KW, Cho SJ, et al. (2009) Developing an institutional protocol guideline for laparoscopy-assisted distal gastrectomy. Ann SurgOncol 16: 2231-2236.
- Kim Y-W, Baik YH, Yun YH, Nam BH, Kim DH, et al. (2008) Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Annals of surgery 248: 721-727.
- Ohgami M, Otani Y, Kumai K, Kubota T, Kim YI, et al. (1999) Curative laparoscopic surgery for early gastric cancer: five years experience. World J Surg 23: 187-192.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15154
- [From(publication date):
April-2014 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 10576
- PDF downloads : 4578