Optic Organ Implantation
Received: 30-May-2022 / Manuscript No. troa-22-68125 / Editor assigned: 01-Jun-2022 / PreQC No. troa-22-68125 / Reviewed: 15-Jun-2022 / QC No. troa-22-68125 / Revised: 20-Jun-2022 / Manuscript No. troa-22-68125 / Accepted Date: 25-Jun-2022 / Published Date: 27-Jun-2022 DOI: 10.4172/troa.1000141
Abstract
Sarcoidosis is a persistent idiopathic granulomatous provocative sickness that can influence many significant organ frameworks, basically the lungs, and subsequently has wonderful clinical heterogeneity. No less than half of patients with fundamental sarcoidosis foster fiery eye illness, and in roughly 21% of cases, it could be the main clinical appearance. Neuro-visual contribution happens in <3% of all sarcoidosis cases, and seldom includes the optic nerve. We depict an uncommon instance of an intraocular sarcoidosis introducing as an indistinct optic nerve mass.
Keywords
Neuro-ocular sarcoidosis; Optic nerve sarcoidosis; Ocular sarcoidosis
Introduction
The goal of recent animal experimental experiments is to use retinal components to replace lost or deteriorated retina and enhance visual function. Different animal species had mature or immature retinal components implanted into the subretinal space.
Cell transplantation is a clever helpful technique to reestablish visual reactions to the ruffian grown-up brain retina and addresses an interesting area of regenerative neurotherapy. Up to this point, it has been shown that relocated postmitotic photoreceptor antecedents can practically incorporate into the grown-up mouse brain retina [1]. In this audit, we examine the separation of photoreceptor cells from both grown-up and undeveloped determined undifferentiated organisms and their true capacity for retinal cell transplantation. We likewise talk about the procedures used to beat hindrances present in the ruffian brain retina and further develop retinal cell combination. At long last, we consider the future interpretation of retinal cell treatment as a helpful technique to treat retinal degeneration.
Undeveloped and non-early stage retina parts of various creatures or of people are utilized as unions. They are relocated to grown-up have creatures. There is the chance of using a back transscleral approach or a vitreoretinal approach. The last option offers a superior visual control. Transplantation of retinal color epithelium could safeguard photoreceptors in grown-up rodents with acquired or age-related macular degeneration [2].
Case report
A 61-year elderly person was alluded to the Liverpool Ocular Oncology Center in 2018 with a right optic nerve head (ONH) mass. He had a one year history of monocular visual misfortune and expanding torment in the right eye that had not answered a fourweek course of oral corticosteroids. His past ophthalmic and general clinical history included: Stage II HL including the left cervical hubs analyzed in 2013 [3], treated with four patterns of chemotherapy and field radiotherapy; mediastinal sarcoidosis thought on a break positron discharge tomography examine during chemotherapy, and affirmed by mediastinal lymph hub biopsy in 2014; as well as diabetes mellitus and fundamental hypertension. The patient's prescription at the hour of LOOC conference included latanoprost, iopidine, atropine drops to the right eye; amlodipine; ramipril and headache medicine. On ophthalmological assessment, vision in the left eye (LE) was 6/6 supported; front portion assessment was typical with an intraocular pressure (IOP) of 19 mmHg. There was no light discernment in the right eye (RE), gentle conjunctival infusion, an unmistakable cornea with a profound and 'calm' foremost chamber, rubeosis iridis and front synechiae. His right IOP was 41 mmHg. The right front glassy was unexceptional. Fundoscopy of the RE uncovered constricted retinal vessels and a non-pigmented mass at the optic plate. B-output of the optic nerve showed a cancer like sore of the ONH reaching out past the lamina cribrosa. The LE fundus was typical.
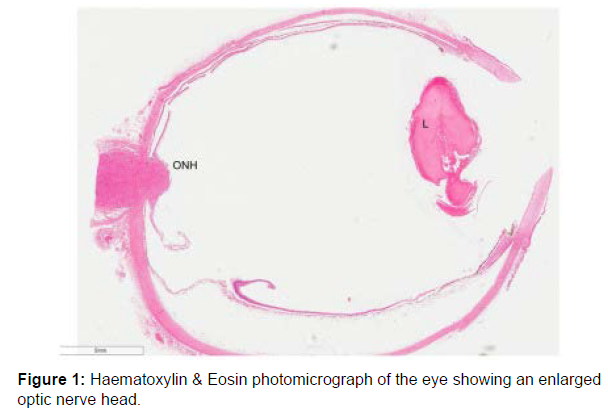
Histomorphological discoveries of the RE included ONH and nerve substitution by a broad non-caseating granulomatous penetrate (Figure 1). The last option was primarily made out of epithelioid histiocytes with plentiful eosinophilic cytoplasm and dissipated plasma cells, eosinophils and little responsive lymphocytes. Large numbers of the epithelioid histiocytes were organized in blended granulomas made [4] out of multinucleated cells shaping Langhans'- type monster cells. The granulomatous penetrate reached out into the optic nerve extraction edge. It was restricted to the optic plate and didn't include either the neighboring retina, sclera or choroid. In the front portion of the eye, the iris showed neovascularisation with extremely fine synechiae between the iris leaves and the back cornea (Figure 2). The focal point showed age-related cataractous changes. In spite of different levels being attempted, granulomata were not found in the whole uveal parcel.
Discussion
Here we present an exceptionally strange instance of histomorphologically-affirmed ONH sarcoidosis in a patient with a foundation history of simultaneous HL and mediastinal sarcoidosis, viewed as disappearing. Neuro-ophthalmic sarcoidosis introducing at first as disengage optic nerve granulomata, with next to no contribution of the uveal parcel, is intriguing. Furthermore, our case exhibits the symptomatic vulnerabilities looked in deciding repetitive sarcoidosis versus a repetitive lymphoma. The case represents concurrent pathologies, named sarcoid-like responses or 'sarcoid-lymphoma condition', which are not great understood.
Sarcoidosis is an ongoing idiopathic granulomatous fiery illness that can influence any significant organ framework, principally the lungs, and subsequently has exceptional heterogeneity in clinical show, discoveries and normal history [5]. The frequency of visual contribution in foundational sarcoidosis is variable as per various examinations, going from 13% in a Turkish report, 21% in Korean review to 53% in a British report, through to 79% in Japanese review. For our situation, enucleation was performed because of a visually impaired excruciating eye inert to steroids. There was broad penetration of the optic nerve and including careful resection edge by non-caseating epithelioid granulomata, though the remainder of the eye hushed up'. As opposed to the histology detailed in past cases,the granulomatous penetrate was restricted to the optic nerve with next to no proof of contribution of the uveal lot. Audit of the past cases demonstrates that optic nerve granuloma is a rare finding, and biopsy is clearly not frequently practical. Attention to cases like our own, with granuloma restricted to the optic nerve [6], as well as the shortfall of optic nerve biopsies in numerous different examples, features the symptomatic vulnerability looked without histological affirmation. Moreover, our case gives a sign of the differential determination of neuro-sarcoidosis in optic nerve sores. This is of specific significance to future practice as intraocular sarcoidosis doesn't be guaranteed to constantly need to include the uveal plot, as composed nearly as creed in numerous Ophthalmology course books. This case likewise legitimizes thought of optic nerve biopsy with regards to serious sight-compromising optic-nerve sores.
Results
At long last, our case was of additional interest because of the intricacy in arriving at a finding because of the patient's experience of simultaneous cervical HL and mediastinal sarcoidosis. Befuddling cross-over exists between the clinical signs of HL and sarcoidosis prompting difficulties in distinctive the two circumstances. Terms to depict the event of HL and sarcoid simultaneously or in a steady progression have been proposed. 'Sarcoid-like' response alludes to the improvement of non-caseating granulomas in patients with a known malignancy. A 'sarcoid-like' response has been seen in organs far off from the essential danger as well as in lymph hubs that channel the neoplastic tissue. conversely, 'Sarcoid-lymphoma' disorder alludes to the advancement of lymphoma in patients with sarcoidosis.
Conclusion
Biopsy is the most reliable method for affirming the determination; be that as it may, biopsy of intraocular tissue or brain tissue is typically not performed because of the intrusiveness and effect of optic nerve biopsy. Rather than the couple of cases detailed, we present discoveries of sarcoid-related granulomatous penetrate restricted to the ONH and missing in other visual tissues. Our case likewise exhibits the ineffectively figured out peculiarity of sarcoid-lymphoma disorder.
Acknowledgement
The authors are grateful to the, Shanghai Jiao Tong University for providing the resources to do the research.
Conflict of Interest
The authors declared no potential conflicts of interest for the research, authorship, and/or publication of this article.
References
- Bawany MH, Kudla C, Khan FA, Chung MM, Aquavella JV (2021) Short-Term Outcomes of Pediatric Keratoprosthesis with the Near-Complete Conjunctival Flap. Cornea 40: 679-684.
- Park J, Phrueksaudomchai P, Cortina MS (2020) Retroprosthetic Membrane: A Complication of Keratoprosthesis with Broad Consequences. Ocul Surf 18: 893-900.
- Lam FC, Chia SN, Lee RMH (2015) Macular Grid Laser Photocoagulation for Branch Retinal Vein Occlusion. Cochrane Database Syst Rev CD008732.
- Gökgöz G, Tortumlu G, Bayar S, Yilmaz G, Haberal M (2022) Peripapillary Vascular Density Measurement in Pediatric Renal and Liver Transplant. Exp Clin Transplant 20: 96-101.
- Atilgan CU, Goker YS, Hondur G, Kosekahya P, Kocer AM, et al. (2022) Evaluation of the Radial Peripapillary Capillary Density in Unilateral Branch Retinal Vein Occlusion and the Unaffected Fellow Eyes. Ther Adv Ophthalmol 14: 25158414221090092.
- Atmaca LS, Atmaca-Sonmez P, Idil A, Kumbasar OO, Celik G (2009) Ocular Involvement in Sarcoidosis. Ocul Immunol Inflamm 17: 91-94.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Chang Y, Zhou L, Vore A (2022) Optic Organ Implantation. Transplant Rep 7: 141. DOI: 10.4172/troa.1000141
Copyright: © 2022 Chang Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1842
- [From(publication date): 0-2022 - Feb 23, 2025]
- Breakdown by view type
- HTML page views: 1629
- PDF downloads: 213