Case Report Open Access
Open Ankle Fracture in Geriatric Patient - A Treatment Strategy
Matthias Bungartz*, Georg Matziolis, Marcel Schulze and Olaf Brinkmann
Department of Orthopaedic, Friedrich-Schiller-Universitat Jena, Campus Eisenberg, Germany
- *Corresponding Author:
- Matthias Bungartz
Department of Orthopaedic, Friedrich-Schiller-Universitat Jena
Campus Eisenberg, Klosterlausnitzer Street. 81, Eisenberg 07607, Germany
Tel: +4915253638112
E-mail: mat.bungartz@gmail.com
Received date: Aug 23, 2016; Accepted date: Sep 13, 2016; Published date: Sep 22, 2016
Citation: Bungartz M, Matziolis G, Schulze M, Brinkmann O (2016) Open Ankle Fracture in Geriatric Patient - A Treatment Strategy. Clin Res Foot Ankle 4:204. doi:10.4172/2329-910X.1000204
Copyright: © 2016 Bungartz M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
The alteration of the age pyramid also leads to changes in the orthopaedic routine. Hence, increasingly more old and very old people (>75.YOA and 91.-100.YOA according to WHO Definition) are being treated with injury patterns that were very rare in this form until now. This could be explained on one hand both by the decreasing osseous stability and the alteration of the soft-tissue condition, and on the other hand by the maintenance of everyday activities even in old age. Thus, low-energy traumas can partly lead to serious injuries. Treatment strategies need to be adapted to the individual cases. The medical care of bones and soft-tissue injuries results to be demanding.
Case Illustration
A 86 years old lady (60 kg; 1.54 m) fell by walking across her icy courtyard and got a third-degree open ankle joint dislocation fracture on the left. She was found hypothermic and anaemic after approximatively 3 hours. Before the accident, the patient was able to manage independently her everyday life.
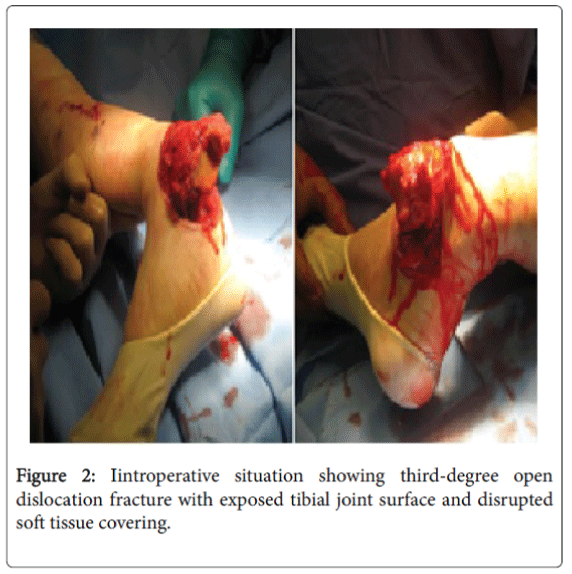
A soiled, distal tibia with exposed articular surface became apparent. Peripheral sensibility and blood perfusion were both intact. The 6 cm long wound – running diagonally above the medial malleolus – showed dirty and avital margins.
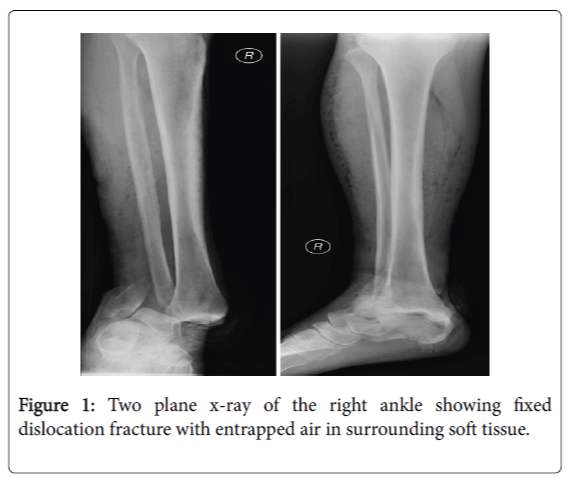
After immediate stabilisation of the vital functions, the patient was taken care in the operation theater. A reposition attempt by an emergency physician at the accident scene failed, therefore no other manoeuvre was undertaken in the emergency room (Figures 1 and 2).
Surgical Treatment
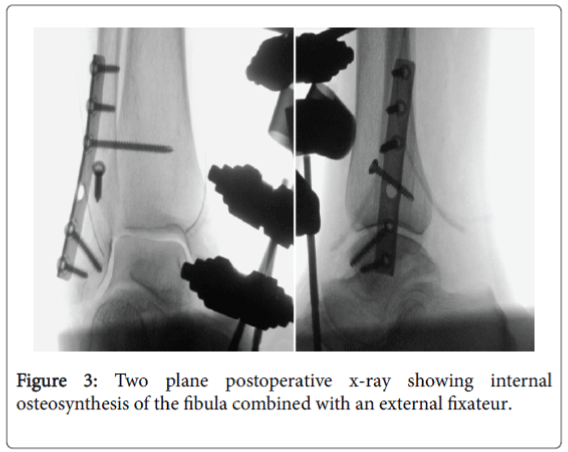
Initially, while in intubation anaesthesia, a mechanical cleaning with a sterile brush and Lavanid® was performed. Afterwards the wound was disinfected with alcohol solution. In a further step, JET-Lavage took place until macroscopic clean conditions were accomplished. The articulation surface showed a flake-fracture in the talus area. The unstable parts were removed. Next, the dislocation was reduced after dilatation incisions and simultaneously a radical debridement of the wound margins was performed. Furthermore the primary reconstruction of the fibula via lateral approach and stabilisation by dorsolateral plate was accomplished. A tension-free lateral and medial skin closure after trans-osseous reinsertion of the torn deltoid ligament followed afterwards. Previously, absorbable antibiotic carriers were inserted in the talo-crural joint for infection prophylaxis. Finally, in order to secure retention and soft-tissue protection, a joint-transfixing tibiometatarsal AO-Fixator was applied (Figure 3).
Two days later a “second-look” operation showed no evidence of macroscopic or microscopic infection. The patient was discharged and transferred to a supervised living structure after suitable conditioning and with irritation-free soft-tissue circumstances.
After 6 weeks, at the planned readmission for removing the fixator, the patient showed a pin-site infection as well as an infected wound margins necrosis in the area of the medial malleolus.
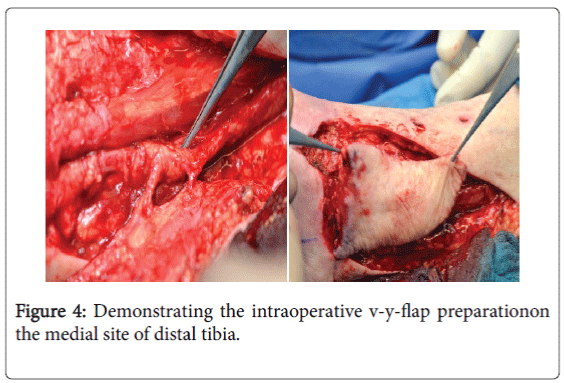
Therefore, the indication was set to remove the fixator, perform a radical soft-tissue debridement and administrate antibiotics locally. Signs for an empyema of the talo-crural joint were not notifiable at the time. After radical debridement, the soft-tissue defect size resulted to be of about 5×4 cm in the area over the medial malleolus.
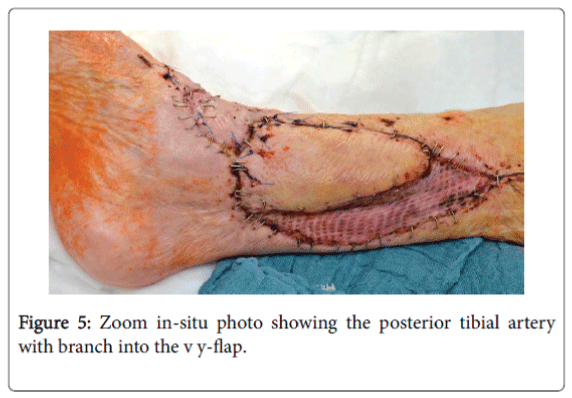
After restoration of the infection and Doppler-sonographic examinations of the vascular status, a VY-Plasty in shape of the posterior tibial artery perforator flap was applied [1-4]. The remaining defect was covered by mesh-graft plasty (Figures 4 and 5).
Discussion
The preservation of injured extremities is very important for maintaining the social integrity of the patient–especially when in old age. The 1- year mortality of all, surgically treated and non surgically treated ankle fractures, ranges in between 6.9% and 15.4% [5]. Bariteau et al. [6] could show a significant decrease of mortality within the group of surgically treated patients with ankle fractures in comparison to the group of patients with conservative treatment.
Hence an operative treatment to provide early mobilisation and rehabilitation should be favoured. One-year mortality was 21.5% for the nonoperative group and 9.1% for the operative group (P<0.0001) [6]. Therefore, it is important to include the whole spectrum of surgical eventualities during the treatment planning [7].
Naturally, the possibly protracted treatment duration and the potential immobilization should be considered. The choice of treatment should be based on the individual cases, there can’t exist socalled standards when the possible conditions are multifactorial [8]. The stage-modality approach in this case report is evident. Stage treatments with combination of internal and external fixation with rapid and consequent soft-tissue covering are fundamentally reasonable.
The interdisciplinary planning is useful from the start since, in many cases, the patients are multimorbid. Concerning the plastic reconstruction, a series of possible variations should be taken into account (local or free flaps), here again the choice of procedure depends in each individual case on the vascular status, the dimensions of the defect, the location and the compliance of the patient. Looking back, it should be questioned – considering the injury extend – if the primary application of a vacuum therapy with “third-look” – after having stated infection-freedom and appropriate vascular diagnostics – if a primary or “early” flap could have prevented the mentioned complications.
Particularly in old age, a high rate of soft-tissue complications in distal extremities should be taken into account. Early revision is better than waiting! In this specific case, short-term clinical reviews could have been better and the necessary programmed revision would not have been delayed.
In summary, it can be stated from our perspective that for the preservation of extremities and function - above all with geriatric patients - the usage and stringent application of all available therapyoptions is necessary and can result to be successful.
References
- Olsen JR, Hunter J, Baumhauer JF (2013) Osteoporotic ankle fractures. OrthopClin North Am 44:225-241.
- Toole WP, Elliott M, Hankins D, Rosenbaum C, Harris A, et al. (2015) Are low-energy open ankle fractures in the elderly the new geriatric hip fracture? J Foot Ankle Surg 54:203-206.
- Strauss EJ, Egol KA (2007) The management of ankle fractures in the elderly. Injury 38:S2-S9.
- Niranjan NS, Price Rd,Govilkar P(2000) Fascialfeederand perforator-based V-Y advancement flaps in the reconstruction of lower limb defects. JPRAS 53:679-689.
- Kadakia RJ, Hsu RY, Hayda R, Lee Y, Bariteau JT(2015) Evaluation of one-year mortality after geriatric ankle fractures in patients admitted to nursing homes. Injury 46:2010-2015.
- Bariteau JT, Hsu RY, Mor V, Lee Y, DiGiovanni CW, et al. (2015) Operative versus nonoperative treatment of geriatric ankle fractures: a Medicare Part A claims database analysis. Foot Ankle Int 36:648-655.
- Herscovici D, Scaduto JM (2012) Management of high-energy foot and ankle injuries in the geriatric population. GeriatrOrthopSurgRehabil 3:33-44.
- Pagliaro AJ, Michelson JD, Mizel MS (2001) Results of operative fixation of unstable ankle fractures in geriatric patients. Foot Ankle Int 22: 399-402.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14092
- [From(publication date):
September-2016 - Jul 02, 2025] - Breakdown by view type
- HTML page views : 13201
- PDF downloads : 891