Commentary Open Access
One Leg Standing Test: A Quantification of the Neuromuscular System for Spine Research and Practice
Paul S Sung*
Department of Physical Therapy, Central Michigan University, USA
- Corresponding Author:
- Paul S. Sung
Department of Physical Therapy
College of Health Professions
Central Michigan University
Health Professions Building 1220
Mt. Pleasant, MI-48859, USA
Tel: 989-774-2347
E-mail: drpsung@gmail.com
Received Date: July 27, 2016; Accepted Date: July 28, 2016; Published Date: July 30, 2016
Citation: Sung SP (2016) One Leg Standing Test: A Quantification of the Neuromuscular System for Spine Research and Practice. J Pain Relief 5:256. doi:10.4172/2167-0846.1000256
Copyright: © 2016 Sung SP, This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Commentary
Recurrent low back pain (LBP) is a common musculoskeletal problem, and there is a 24% to 87% recurrence rate within one year [1,2]. Those who have recovered from an episode of LBP demonstrated altered paraspinal muscle spindle afference and central processing of this sensory input for balance performance [3-5], altered proprioceptive postural control that might be caused by anticipation of postural instability, and less refined positional sense [6-8]. However, there is a lack of data to quantify altered kinematic and kinetic changes from postural coordination and balance performance in subjects with neuromuscular dysfunction.
The source of pain is the dysfunction, which is an impairment of the musculoskeletal system and/or the neuromuscular system. However, clinicians are often focused on the pain itself rather than on understanding the specific nature of the dysfunction, which is the source of pain within the neuromuscular, musculoskeletal, cardiopulmonary, and integumentary systems. The characteristics of clinical research are often misleading since pain control is developed from subjective data rather than a quantified measure.
The physiological organ systems interact to produce and support movement, which articulates the neuromuscular and musculoskeletal systems. The dissemination of quantifying neuromuscular research findings in peer-reviewed journals has been relatively weak when the principle is not always applied in practice. It would be beneficial to focus on clinical applications based on correct research designs with sensitive measures to understand the dysfunction. For example, fear of falling in older women is a common and persistent complaint that is caused mainly by impairments of balance and mobility and is known to affect quality of life in older adults [9].
There is great variation in the reported prevalence of fear of falling in older adults, which is associated with multiple factors including physical and psychological factors as well as poor health status [10,11]. These variations have warranted further investigation for a complete understanding of the role of these factors in relation to fear of falling [12]. Fear of falling contains potentially serious outcomes, and the results for balance problems or fear of falling imply that early intervention must be important in fall prevention. However, the approach might ignore the validity or reliability of the data as well as its comprehensive analyses while considering the four systems of human motion. When we analyze the obtained data, we might not apply the data to patient care in practical ways.
Recent studies have been mostly performed to evaluate the role of transabdominal and paraspinal muscles on core stability for LBP recurrence [13-15]. It is evident that pain is attributed to postural instability and balance deficits due to changes in proprioception and postural control strategies [16,17]. In order to assess static postural control and balance control, the one leg standing test is frequently used in clinical assessments since approximately 40% of human gait movement occurs during one leg stance [18,19]. The variations in balance and body sway also suggested that kinematic changes of the trunk were compensated by postural alignment and core spine stability [8,20].
Those subjects with recurrent LBP demonstrate less refined positional sense and altered proprioceptive postural control [6-8]. Postural stability might be changed due to a possible pain avoiding strategy from the standing limb. The diminished feedback for core spine control might be compensated by the trunk for integrated balance performance as the control group took advantage of core spine activity in addition to lumbar spine stability [21]. As a result, clinicians need to consider motor control of integrated balance activity in addition to trunk stability to refine postural adaptations in elderly subjects with balance deficits.
Because exercise interventions relate to changes in motor control, it is important to investigate the effects of intervention in terms of the musculoskeletal and/or neurological link [5,22]. Although some therapeutic interventions have demonstrated benefits, researchers have not quantified or characterized the results yielded by specific nonsurgical interventions. Furthermore, kinematic and kinetic assessments of postural stability require further measurements which can provide three-dimensional dynamic motion data. The aberrant lumbo-pelvic motion in individuals with LBP might be directly related to trunk rotations and pain [21,23].
Valid and reliable measurement tools for balance deficits associated with fear of falling would be important for clinicians to use before developing rehabilitation strategies. Most clinical outcome studies are still not convincing in their measurements, and implications of the specific tasks need to be further investigated [5,24]. For example, center of pressure displacement may provide useful information in quantifying standing postural stability as well as predicting dynamic balance [25]; however, the displacement provides limited results as it is only a two-dimensional quantity.
Despite numerous efforts over the years, valid and reliable assessment tools for balance deficits in subjects with fear of falling and postural dysfunction remain elusive. Individual aspects of multifactorial issues need to be investigated in long-term, follow-up studies with quantified assessment tools. There is growing scientific evidence supporting the one leg balance test as a significant and easyto- administer predictor of injurious falls. However, no single factor seems to be accurate enough to be the sole predictor of fall risk or fall injury risk because many diverse factors are involved in falling [26]. The one leg standing test was introduced as reliable assessment tool to provide a valid measurement of postural steadiness [21]. It is important to investigate the assessment tools for motor coordination since they are not simply related to muscle activation, but appear to be related to the task [5,22].
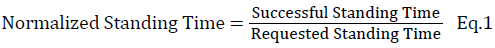
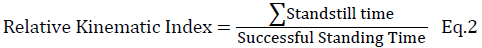
The one leg standing test is based on how posture is stable during the time of standing. A normalized standing time is defined as a ratio between the successful standing time and the requested standing time (Eq.1). The successful standing time is the amount of time the subject is able to successfully stand based on the amount of time requested. A relative kinematic index is the ratio between standstill time and successful standing time (Eq. 2). The standstill time is the summation of temporal segments where the three-dimensional rotation (Rxyz) of the tested axis is below the threshold. The Rxyz is defined as the rotational angle of each specific body region (Eq. 3), which is calculated between two adjacent joints in three dimensions and then combined to quantify the relative kinematic index.
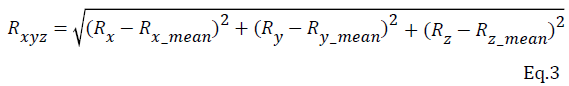
In this way, body segments are modeled as rigid bodies, and the relative rotation angles are taken from a fixed point in the center of the joint. Those kinematic data might be applied to describe relative rotations of one segment with respect to another reference segment based on the angular changes.
It was reported that most of the research on the neuro-musculoskeletal system completed thus far has been cross-sectional in nature and has not compared the individual aspects of multidimensional factors, which led to an inaccurate estimate of the true effect of fallrelated fear [27,28]. There are needs for pain control and balance dysfunction to provide more longitudinal and prospective research with a constructive design and specific inclusionary and exclusionary criteria. Therefore, this study will investigate integrated measurements, such as the level of pain/disability as well as kinetic, kinematic, and muscle activation patterns by electromyography, compared with other fear of falling scales.
Understanding the mechanisms and responses associated with postural dysfunction will ultimately enhance the clinical application and quality of care for those subjects with balance deficits. The kinetic and kinematic changes in three-dimensional trunk motion could be compared to reflect standing balance contributions to postural control [21]. Postural compensation based on the one leg standing test may lead to a better understanding of human motion patterns and falling to clarify clinical applications for quality of care.
References
- Pengel LH, Herbert RD, Maher CG, Refshauge KM (2003) Acute low back pain: systematic review of its prognosis. BMJ 327: 323.
- Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, et al. (2008) After an episode of acute low back pain, recurrence is unpredictable and not as common as previously thought. Spine (Phila Pa 1976)33: 2923-2928.
- Sung PS, Park HS (2009) Gender differences in ground reaction force following perturbations in subjects with low back pain. Gait Posture 29: 290-295.
- Brumagne S, Cordo P, Lysens R, Verschueren S, Swinnen S (2000) The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine (Phila Pa 1976) 25: 989-994.
- Tsao H, Druitt TR, Schollum TM, Hodges PW (2010) Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain. J Pain 11: 1120-1128.
- Brumagne S, Janssens L, Knapen S, Claeys K, Suuden-Johanson E (2008) Persons with recurrent low back pain exhibit a rigid postural control strategy. Eur Spine J 17: 1177-1184.
- Sung PS (2013) Disability and back muscle fatigability changes following two therapeutic exercise interventions in participants with recurrent low back pain. Med SciMonit 19: 40-48.
- Tsao H, Hodges PW (2008) Persistence of improvements in postural strategies following motor control training in people with recurrent low back pain. J ElectromyogrKinesiol 18: 559-567.
- Tinetti ME, Richman D, Powell L (1990) Falls efficacy as a measure of fear of falling. J Gerontol 45: P239-243.
- Cumming RG, Salkeld G, Thomas M, Szonyi G (2000) Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A BiolSci Med Sci 55: M299-305.
- Salkeld G, Cameron ID, Cumming RG, Easter S, Seymour J, et al. (2000) Quality of life related to fear of falling and hip fracture in older women: a time trade off study. BMJ 320: 341-346.
- Legters K (2002) Fear of falling. PhysTher 82: 264-272.
- Heidari P, Farahbakhsh F, Rostami M, Noormohammadpour P, Kordi R (2015) The role of ultrasound in diagnosis of the causes of low back pain: a review of the literature. Asian J Sports Med 6: e23803.
- Hides J, Wilson S, Stanton W, McMahon S, Keto H, et al. (2006) An MRI investigation into the function of the transversusabdominis muscle during "drawing-in" of the abdominal wall. Spine (Phila Pa 1976) 31: E175-178.
- Teyhen DS, Miltenberger CE, Deiters HM, Del Toro YM, Pulliam JN, et al. (2005) The use of ultrasound imaging of the abdominal drawing-in maneuver in subjects with low back pain. J Orthop Sports PhysTher 35: 346-355.
- MacDonald D, Moseley GL, Hodges PW (2010) People with recurrent low back pain respond differently to trunk loading despite remission from symptoms. Spine (Phila Pa 1976) 35: 818-824.
- Brumagne S, Cordo P, Verschueren S (2004) Proprioceptive weighting changes in persons with low back pain and elderly persons during upright standing. NeurosciLett 366: 63-66.
- Aberg AC, Thorstensson A, Tarassova O, Halvorsen K (2011) Calculations of mechanisms for balance control during narrow and single-leg standing in fit older adults: A reliability study. Gait Posture 34: 352-357.
- Verhagen E, Bobbert M, Inklaar M, van Kalken M, van der Beek A, et al. (2005) The effect of a balance training programme on centre of pressure excursion in one-leg stance. ClinBiomech (Bristol, Avon) 20: 1094-1100.
- Lee DC, Ham YW, Sung PS (2012) Effect of visual input on normalized standing stability in subjects with recurrent low back pain. Gait Posture 36: 580-585.
- Sung PS, Leininger PM (2015) A kinematic and kinetic analysis of spinal region in subjects with and without recurrent low back pain during one leg standing. ClinBiomech (Bristol, Avon) 30: 696-702.
- Hodges P, van den Hoorn W, Dawson A, Cholewicki J (2009) Changes in the mechanical properties of the trunk in low back pain may be associated with recurrence. J Biomech 42: 61-66.
- Sung PS1 (2014) A kinematic analysis for shoulder and pelvis coordination during axial trunk rotation in subjects with and without recurrent low back pain. Gait Posture 40: 493-498.
- Baldwin KM, Haddad F (2001) Effects of different activity and inactivity paradigms on myosin heavy chain gene expression in striated muscle. J ApplPhysiol (1985) 90: 345-357.
- Rhee HS, Kim YH, Sung PS (2012) A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain. Med SciMonit 18: CR174-81.
- Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, et al. (1997) One-leg balance is an important predictor of injurious falls in older persons. J Am GeriatrSoc 45: 735-738.
- Young WR, Mark Williams A (2015) How fear of falling can increase fall-risk in older adults: applying psychological theory to practical observations. Gait Posture 41: 7-12.
- Chomiak T, Pereira FV, Clark TW, Cihal A, Hu B (2015) Concurrent arm swing-stepping (CASS) can reveal gait start hesitation in Parkinson's patients with low self-efficacy and fear of falling. Aging ClinExp Res 27: 457-463.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 13177
- [From(publication date):
July-2016 - Apr 26, 2025] - Breakdown by view type
- HTML page views : 12191
- PDF downloads : 986
