Ocular Syphilis: A Rare Complication of an Emerging Disease
Received: 30-Nov-2020 / Accepted Date: 14-Dec-2020 / Published Date: 21-Dec-2020
Abstract
Syphilis rates in the United States have had a dramatic increase in the past 10 years. Incidence in 2018 of primary and secondary syphilis was 10.8 cases per 100,000, a 71.4% increase from the incidence in 2014. With the increase in incidence of primary and secondary syphilis awareness of the complications of this disease are paramount. A rare complication is ocular involvement. We present the case of a 60-year-old man who presented with ocular syphilis. Given the emerging public health concern of this illness understanding rare presentations is essential for contact tracing and infection control.
Keywords: Ocular syphilis; Contact tracing; Infection control; Amphetamine
Keywords
Ocular syphilis; Contact tracing; Infection control; Amphetamine
Case report
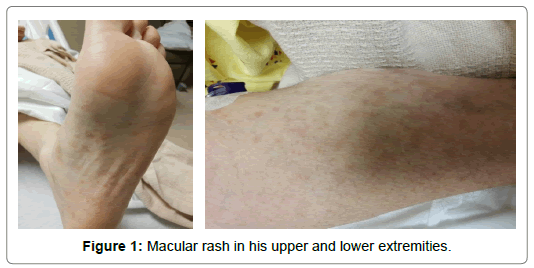
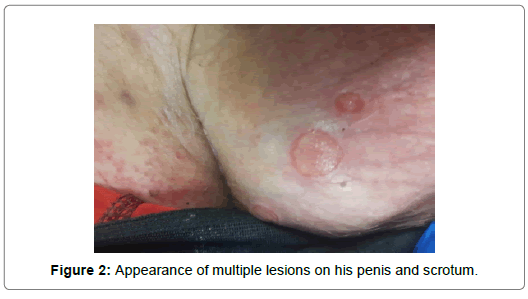
A 60-year-old Caucasian male with past medical history of hypertension, hyper-lipidemia and amphetamine abuse presented with chief complaint of painful left eye blindness and worsening vision of the right eye. Five months prior he noticed a painless ulcer on the dorsum of his penis. The ulcer did not improve and was intermittently painful. Two months after the appearance of the ulcer he started developing a pruritic, macular rash in his upper and lower extremities (Figures 1-2). One month after developing the rash, he started having intermittent transient episodes of vision loss in the left eye. These episodes lasted for 45-60 seconds; were associated with eye pain and photophobia which was partially alleviated by aspirin and acetaminophen. During this time, he also reported having a 40 pound unintentional weight loss and the appearance of multiple lesions on his penis and scrotum (Figure 3). The left eye vision loss progressed to complete permanent loss of vision. One week after the complete vision loss in his left eye he began to have transient vision loss in his right at which point he saw an ophthalmologist. He was seen by ophthalmology and was diagnosed with pan uveitis on the left eye and edema on the right optic nerve. RPR was reactive with a dilution of 1:256 at which point he was admitted to our hospital for further work up. Social history was pertinent for multiple sexual partners in his life, with 3 in the past 2 years without the use of contraception. He participated in oral and anal sex, with only female partners and denied any previous history of sexually transmitted disease. On admission vital signs were within normal limits and he was AAOx3. Extra ocular movements were intact with bilateral pupil constriction and swelling noted of left globe which was erythematous, with ecchymosis. He was unable to perceive images, movement or light with the left eye. A non-painful, diffuse maculopapular rash was noted in all extremities and the upper trunk. 5 genital ulcers measuring 1 cm X 1cm on the dorsum of the penis and scrotum were noted. Proprioception was decreased bilaterally. Laboratory studies showed a normal CBC and BMP. The Hepatitis panel and HIV were negative. A urine drug screen was positive for amphetamines. A lumbar puncture was performed with an opening pressure of 10cm H20, CSF fluid was hazy and pink CSF. Protein was 63.2 mg/dl, glucose 57 mg/dl, WBC 213/ mm3, Mononuclear 91%, RBC 5,000/mm3. Serum VDRL was reactive with a dilution of >1:512. CSF VDRL was non-reactive. Serum TPPA was reactive. Herpes panel, Tuberculosis, Enterovirus in the CSF were all negative. Neisseria and Gonorrhoea were negative. Because of the patient’s persistent headache and painful vision loss he underwent a bilateral temporal artery biopsy which showed no inflammatory infiltrates, giant cells, or granulomas. No steroids were given. CT and MRI of the brain did not show any abnormalities. Given his positive lumbar puncture, and clinical exam findings he was diagnosed with secondary syphilis and neurosyphilis with ocular involvement. He was started on Penicillin G-4 million units every 4 hours, for a total of 14 days. After monitored for 48 hours for the Jarisch-Herxheimer reaction he was discharged. No vision recovery on the left eye was noted at the time of discharge, however, the headache and eye pain had resolved.
Discussion
Ocular syphilis is a rare manifestation of syphilis that affects various parts of the eye, and it is considered a type of neurosyphilis [1]. It can present in many different ways including uveitis as in our patient, retinitis, vitritis, and retinal vasculitis. In those that are HIV positive, ocular syphilis has a tendency to present as placoid chorioretinitis of the macula. Given the various structures that can be affected, it makes sense that the patient may present with complaints ranging from pain to blurry vision to outright blindness. Of note, symptoms may occur acutely as in our patient or chronically [2]. Depending on the structure infected, the severity of the infection, and the duration of infectious burden, resolution of infection and salvage of visual acuity is possible [3]. The incidence of ocular syphilis is rising. A study in 2016 found that ocular manifestations were present in 0.17% to 3.9% of syphilis cases. Given the possible loss of function from ocular syphilis, these rising numbers pose great concern in clinical practice. True cases are likely higher as underreporting likely contributes to underrepresentation of true incidence. The likelihood of ocular syphilis does not appear to be higher in those who received their infections from a partner who developed ocular syphilis. Of note, it does appear that ocular syphilis and HIV infection share some link. Some studies have found that ocular syphilis was associated with HIV infection in up to 80% of cases making co-testing paramount [1-3]. Given the potential for reversible vision loss makes understanding of presentation and diagnosis essential. In general, penicillin is the treatment of choice for all types of syphilis. The stage and clinical manifestations of the disease affect the duration, route of administration, and dose used. Primary and secondary syphilis can be treated with a sing dose of penicillin G 2.4 MU IM, whereas neurosyphilis requires the use of aqueous crystalline penicillin G 18-24 MU/day IV for 10-14 days [3]. Some studies have shown that ocular syphilis can be treated as secondary syphilis among those who are HIV negative and as neurosyphilis among those who are HIV positive. Current guidelines recommend treating all cases of ocular syphilis with the same regiment as neurosyphilis as outlined above regardless of HIV status [2-3]. Given the increasing incidence of syphilis in the United States understanding rare presentations is important for prompt diagnosis and treatment. Early identification is essential to prevent long term devastating complications as seen in our patient.
References
- Marx GE, Dhanireddy S, Marrazzo JM (2016) Variations in Clinical Presentation of Ocular Syphilis: Case Series Reported From a Growing Epidemic in the United States. Sexu Transmit Dis 43: 519-23.
- Oliver SE, Aubin M, Atwell L (2016). Ocular Syphilis: Eight Jurisdictions, United States. Mortal Wkly Rep65:1185-88.
- Parc CE, Chahed S, Patel SV (2007) Manifestations and Treatment of Ocular Syphilis during an Epidemic in France. Sexu Transmit Dis 34: 553-56.
Citation: Peng Y (2020) Ocular Syphilis: A Rare Complication of an Emerging Disease. J Neuroinfect Dis 11: 311.
Copyright: © 2020 Peng Y. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3053
- [From(publication date): 0-2020 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 2462
- PDF downloads: 591