Research Article Open Access
Obesity-related Dietary Behaviours among Racially and Ethnically Diverse Pregnant and Postpartum Women
Ashley Harris1*, Nymisha Chilukuri1, Meredith West1, David Levine1, Janice Henderson2, Shari Lawson2, Sarah Polk3 and Wendy L Bennett 1,4,5
1The Johns Hopkins University School of Medicine, Division of General Internal Medicine, Baltimore, MD, USA
2Department of Gynecology and Obstetrics, The Johns Hopkins University School of Medicine, Baltimore, MD, USA
3Department of Pediatrics, Division of General Pediatrics and Adolescent Medicine, The Johns Hopkins University School of Medicine, Baltimore, MD, USA
4Welch Center for Prevention, Epidemiology and Clinical Research, The Johns Hopkins University, Baltimore, MD, USA
5The Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA
- Corresponding Author:
- Ashley Harris
The Johns Hopkins University School of Medicine
Division of General Internal Medicine
Baltimore, MD, USA
Tel: 203-921-7233
Fax: 410-955-0476
E-mail: aharr101@jhmi.edu
Received date: March 21, 2016; Accepted date: April 01, 2016; Published date: April 06, 2016
Citation: Harris A, Chilukuri N, West M, Levine D, Henderson J, et al. (2016) Obesity-related Dietary Behaviours among Racially and Ethnically Diverse Pregnant and Postpartum Women. J Preg Child Health 3: 238. doi:10.4172/2376-127X.1000238
Copyright: © 2016 Harris A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Introduction: Obesity is common among reproductive age women, and disproportionately im-pacts racial/ethnic minorities. Our objective was to assess racial/ethnic differences in obesity-related dietary behaviors among pregnant and postpartum women, to inform peripartum weight management interventions that target diverse populations. Methods: We conducted a cross-sectional survey of 212 Black (44%), Hispanic (31%) and White (25%) women, age ≥18, pregnant or within one year postpartum, in hospital-based clinics in Bal-timore Maryland in 2013. Outcomes were fast food or sugar-sweetened beverage intake once or more weekly. We used logistic regression to evaluate the association between race/ethnicity and obesity-related dietary behaviors, adjusting for sociodemographic factors. Results: In adjusted analyses, Black women had 2.4 increased odds of fast food intake once or more weekly compared to White women (CI=1.08, 5.23). There were no racial/ethnic differences in the odds of sugar-sweetened beverage intake. Discussion: Compared with White or Hispanic women, Black women had 2-fold higher odds of fast food intake once or more weekly. Black women might benefit from targeted counseling and intervention to reduce fast food intake during and after pregnancy.
Introduction
Obesity is increasingly prevalent among reproductive age women [1-3] and is associated with pregnancy complications such as gestational diabetes and hypertensive disorders of pregnancy [2,4-6]. Obesity disproportionately impacts women of racial and ethnic minorities, with highest rates in Black women, followed by Hispanic and White women [3] and potentially contributes to racial and ethnic disparities in other chronic diseases such as diabetes, hypertension and cardiovascular disease [7-9]. Like preconception obesity, gaining excessive gestational weight, disproportionately affects racial and ethnic minorities [2] is associated with pregnancy complications and future risk of long term overweight and obesity [10,11].
Pregnancy provides an opportunity to identify unhealthy behaviors and promote healthy eating habits, which can be sustained beyond pregnancy. Understanding racial and ethnic differences in health behaviors could inform and target future interventions. However, evidence is not yet clear whether the observed racial and ethnic differences in preconception obesity and gestational weight gain are associated with differences in obesity-related dietary behaviors [12-16]. Further, we found no studies specifically evaluating fast food and sugar-sweetened beverage intake in this population, two potentially modifiable dietary behaviors which are associated with obesity [17-19]. Previous studies used health behavior surveys to evaluate differences in dietary habits between Black and Hispanic women, but results did not show consistent differences between the racial and ethnic groups [12-14,16]. The largest of these four studies excluded women with chronic medical co-morbidities such as hypertension or diabetes [12] or high risk pregnancies [16]. Another large, prospective cohort of 2394 women used food frequency questionnaires to evaluate dietary differences among racial groups [15] but the study populations was primarily middle class.
Our primary objective was to address an important evidence gap: the association between race and ethnicity and differences in in women√ʬ?¬?s obesity-related dietary behaviors during pregnancy and after delivery. Based on evidence from previous studies [1-3,12,14] we hypothesized that Black women would have higher odds of both fast food and sugar-sweetened beverage intake. Our secondary objective was to describe the perceived barriers to healthy dietary behaviors, and potential interventions to address these barriers. We anticipate using this information to directly inform weight management interventions in pregnant and postpartum women.
Methods
Study design
We conducted a cross-sectional analysis using data collected in a convenience sample, using a one-time, self-administered questionnaire describing health behaviors among a sample of pregnant and postpartum women. This study was approved by the Johns Hopkins University School of Medicine Institutional Review Board.
Sample population
A total of 247 English or Spanish speaking women, ≥ 18 years old, pregnant or within 1 year postpartum, who reported the ability to read the survey in English or Spanish, completed the survey. Women were recruited from 1 of 4 outpatient clinics, (including high risk obstetrics and pediatrics practices), in 2 academic hospitals in Baltimore, Maryland between January and April 2013. Participants completed a one-time self-administered questionnaire at the time of their or their children√ʬ?¬?s appointments. Of the 247 women, the 212 women who identified as Black, Hispanic, or White, were included in this secondary analysis. The 35 participants in the other racial categories 4% were Asian, 0.4% were Hawaiian or Pacific Islander, 1.6% was American Indian or Native Alaskan, and 3.3% described themselves as multiethnic. The diversity of the other racial/ethnic group limited our ability to make comparative inferences about their dietary habits, and these women were thus excluded from this analysis.
Our study was performed on a convenience sample. Data was collected only from those women who were approached and agreed to participate. We did not calculate the percent of patients approached who agreed to participate in our study, or evaluate the ways in which the participating women may differ from those women that chose not to participate.
Measure
The survey, which included questions about socio-demographics, dietary behaviors, and facilitators and barriers to lifestyle changes, was adapted from validated national survey instruments [20-22]. Items on fast food were adapted from the Coronary Artery Risk Development in Adults Study: How many times in the past week did you eat out in a fast food restaurant such as McDonald√ʬ?¬?s, Burger King, Wendy√ʬ?¬?s, Arby√ʬ?¬?s, Pizza Hut or Kentucky Fried Chicken? (1) Never or less than once weekly, (2) 1-2 times per week, (3) More than 3 times per week but less than daily, (4) At least daily [20]. Items related to sugar-sweetened beverages were adapted from the Behavioral Risk Factor Surveillance System: In the past 7 days, how often did you drink soda (not diet), or other sugar-sweetened beverages, like Hawaiian Punch, lemonade or Kool-Aid? (1) Never or less than 1 can per week, (2) 1-2 cans per week, (3) More than 3 cans per week but less than daily, (4) about 1 can per day, (5) 2 or more cans per day [21].
The final questionnaire was translated into Spanish and back translated to English. A pilot study was performed to ensure that the questionnaire met criteria for a 5th grade literacy level, as well as culture appropriateness, ease of understanding, and quick time to completion.
Definition of main predictor variables: Race/Ethnicity and BMI
Race and ethnicity were self-reported on the questionnaire. Participants were asked the following questions: Are you Hispanic or Latino?: Which of the following best describes your race? (Check all that apply): Asian, African American or Black, Caucasian/White/ European American, Native Hawaiian or other Pacific Islander, American Indian/Alaska Native, or Multiethnic or mixed. We then categorized the racial and ethnic groups into African American/Black, Hispanic, Caucasian, or other races/ethnicities. As above, women reporting other racial or ethnic categories, were not included in the analysis.
Preconception body mass index (BMI) was calculated based on selfreported height and preconception weight for pregnant women, and current weight for postpartum women and categorized into obese (BMI ≥ 30) and non-obese (BMI<30) [23,24].
Definition of outcomes
The primary outcomes were fast food frequency and sugarsweetened beverage intake, both defined as less than once weekly versus once or more weekly. The rationale for these cut-points was based on the median intake in our sample. Prior studies used similar cut-points and showed that the consumption of fast food two or more times per week was associated with weight gain and insulin resistance over 15 years, when compared to those who eat fast food less than twice weekly [18]. Notably, existing literature on sugar-sweetened beverage intake demonstrated greatest risk of weight gain [25] and coronary heart disease [26,27] with at least daily consumption of sugar-sweetened beverages. A frequency cut-point of once or greater per week was also deemed simple to assess clinically and to be potentially actionable.
Other covariates
Socio-demographic variables included age, language proficiency, marital status, education, employment and income. Age was categorized: 18-24, 25-29, 30-34, ≥35. English language proficiency was categorized as √ʬ?¬?adequate√ʬ?¬Ě, if the respondent reported very good English language proficiency, and √ʬ?¬?limited√ʬ?¬Ě for other responses, based on response categorization in the U.S. Census [28]. A binary variable for marital status was created to assess differences between those who were married or living with a partner, and those who were not.
Education level was divided into three variables including those with less than a high school education, those graduating high school or obtaining a GED, and those with one or more years of college. Employment was assessed, and categorized into employed (full or part time), unemployed, maternity leave, home maker, disability, or student. We also assessed income, and categorized the data into broad categories, as noted in Table 1. Financial strain was a separate income variable, based on participant response to the survey question √ʬ?¬?In the past 12 months, was there ever a time when you did not have enough money to meet the daily needs of you and your family?
| Overall n=212 |
Black n=95 |
Hispanic n=63 |
Caucasian n=54 |
P Value |
||
|---|---|---|---|---|---|---|
| Individual Demographic Covariates | Number (%) | Number (%) | Number (%) | Number (%) | ||
| Maternal Age<0.0001 | ||||||
| 18-24 | 74 (34.9) | 46 (48.4) | 21 (33.3) | 7 (13.0) | ||
| 25-29 | 65 (30.7) | 30 (31.6) | 19 (30.2) | 16 (29.6) | ||
| 30-34 | 36 (17.0) | 9 (9.5) | 12 (19.0) | 15 (27.8) | ||
| ≥35 | 37 (17.4) | 10 (10.5) | 11 (17.5) | 16 (29.6) | ||
| English Language Proficiencya | <0.0001 | |||||
| Adequate | 157 (74.1) | 94 (98.9) | 10 (15.9) | 53 (100) | ||
| Language spoken at home | <0.0001 | |||||
| English | 157 (75.1) | 94 (100) | 10 (16.1) | 53 (100) | ||
| Marital Status | <0.0001 | |||||
| Married/Live-in Partner | 153 (68.6) | 50 (52.6) | 54 (85.7) | 43 (79.6) | ||
| Childcareb | 0.04 | |||||
| Yes | 43 (20.3) | 46 (48.4) | 16 (25.4) | 24 (44.4) | ||
| Not required | 86 (40.6) | 31 (32.6) | 31 (49.2) | 19 (35.2) | ||
| No | 81 (38.2) | 18 (19.0) | 14 (22.2) | 11 (20.4) | ||
| Child under 5 years old | 0.28 | |||||
| Yes | 139 (65.6) | 63 (66.3) | 45 (71.4) | 31 (57.4) | ||
| Education | <0.0001 | |||||
| ≤Grade 11 | 53 (25.2) | 13 (13.8) | 33 (53.2) | 7 (13.0) | ||
| High school / GED | 73 (34.8) | 45 (47.9) | 19 (30.7) | 9 (16.6) | ||
| ≥1 year college | 84 (40.0) | 36 (38.3) | 10 (16.1) | 38 (70.4) | ||
| Employment | <0.0001 | |||||
| Employed Full/Part Time | 75 (36.6) | 34 (37.0) | 14 (23.7) | 27 (50.0) | ||
| Unemployed | 52 (25.4) | 31 (33.7) | 12 (20.3) | 9 (16.7) | ||
| Maternity Leave | 12 (5.89) | 10 (10.9) | 0 (0.0) | 2 (3.7) | ||
| Disability | 10(4.9) | 6 (6.5) | 1 (1.7) | 3 (5.5) | ||
| Homemaker | 46 (22.4) | 6 (6.5) | 30 (50.8) | 10 (18.6) | ||
| Student | 10 (4.9) | 5 (5.4) | 2 (3.5) | 3 (5.5) | ||
| Income | <0.0001 | |||||
| <10,000 | 49 (23.1) | 33 (34.7) | 11 (17.5) | 5 (9.3) | ||
| 10,000-19,999 | 41 (19.3) | 18 (18.9) | 16 (25.4) | 7 (13.0) | ||
| 20,000-34,999 | 23 (10.9) | 13 (13.7) | 7 (11.1) | 3 (5.5) | ||
| 35,000-49,999 | 10 (4.7) | 5 (5.3) | 2 (3.2) | 3 (5.5) | ||
| >50,000 | 38 (17.9) | 4 (4.2) | 4 (6.3) | 30 (55.6) | ||
| Declined to answer | 51 (24.1) | 22 (23.2) | 23 (36.5) | 6 (11.1) | ||
| Financial Strain | 0.003 | |||||
| Yes | 92 (41.3) | 46 (48.4) | 29 (46.0) | 12 (22.2) | ||
| No | 127 (56.9) | 48 (50.5) | 31 (49.2) | 42 (77.8) | ||
| Access to Care | ||||||
| Insurance | <0.0001 | |||||
| Private | 51 (25.3) | 14 (15.1) | 5 (8.9) | 32 (60.4) | ||
| Medicaid | 110 (54.5) | 74 (79.6) | 15 (26.8) | 21 (39.6) | ||
| Medicare | 4 (2.0) | 3 (3.2) | 1 (1.8) | 0 (0.0) | ||
| Uninsured | 37 (18.3) | 2 (2.1) | 35 (62.5) | 0 (0.0) | ||
| Primary Care Physician<0.0001 | ||||||
| Yes | 131 (58.7) | 69 (72.6) | 12 (19.0) | 45 (83.3) | ||
| No | 90 (40.4) | 25 (26.3) | 50 (79.4) | 9 (16.7) | ||
| Don’t Know | √?¬†210 (0.9)(1.1)(1.6) |
|||||
| Medical Status | ||||||
| Pregnancy Status0.1 | ||||||
| Pregnant | 179 (84.4) | 83 (87.4) | 48 (76.2) | 48 (88.9) | ||
| Postpartum | 33 (15.6) | 12 (12.6) | 15 (23.8) | 6 (11.1) | ||
| Pre-pregnancy BMIc<0.0001 | ||||||
| <18.5 | 5 (2.3) | 2 (2.1) | 1 (1.6) | 2 (3.7) | ||
| 18.5-24.9 | 50 (23.6) | 17 (17.9) | 9 (14.3) | 24 (44.4) | ||
| 25-29.9 | 49 (23.1) | 22 (23.2) | 15 (23.8) | 12 (22.2) | ||
| 30-39.9 | 60 (28.3) | 37 (38.9) | 10 (15.9) | 13 (24.1) | ||
| >40.0 | 15 (7.1) | 11 (11.6) | 2 (3.2) | 2 (3.7) | ||
| NR | 33 (15.6) | 6 (6.3) | 26 (41.2) | 1 (1.9) | ||
| Medical Co-morbidities | ||||||
| Any medical co-morbidity | 122 (57.6) | 57 (60.0) | 41 (65.1) | 24 (44.4) | 0.06 | |
| Overweight or obesity | 157 (74.1) | 76 (80.0) | 53 (84.1) | 28 (51.9) | <0.0001 | |
| Obesity | 108 (50.9) | 54 (56.8) | 38 (60.3) | 16 (29.6) | 0.001 | |
| Type II Diabetes | 15 (7.1) | 10 (10.5) | 3 (4.8) | 2 (3.7) | 0.21 | |
| Hypertension | 24 (11.3) | 12 (12.6) | 4 (6.3) | 8 (14.8) | 0.31 | |
| Pregnancy Complications | ||||||
| Gestational diabetes | 26 (12.3) | 8 (8.4) | 6 (9.5) | 12 (22.2) | 0.04 | |
| Smoke0.9 | ||||||
| Yes | 19 (9.0) | 9 (9.5) | 2 (3.2) | 8 (14.8) | 0.09 | |
| Self reported health status0.005 | ||||||
| Good | 177 (83.5) | 76 (80.0) | 47 (74.6) | 54 (100.0) | ||
| Fair/Poor | 33 (15.6) | 18 (18.9) | 15 (23.8) | 0 (0.0) | ||
| Sleep Quality0.04 | ||||||
| Good | 114 (53.8) | 60 (63.2) | 28 (44.4) | 26 (48.1) | ||
| *Numbers not adding to N in sample, and percentages not leading to 100% are due to non-responses. a) English Language Proficiency defined as adequate vs not adequate b) Childcare: Yes defined as childcare other than parents obtained, not needed defined as no children in need of childcare, no defined as childcare provided by parents c) Based on respondents only Abbreviations: GED=Graduate Equivalency Degree |
||||||
Table 1: Characteristics of pregnant and postpartum women by race/ethnicity.*
Pregnancy status and medical co-morbidities were binary variables based on responses to a question “Have you been told that you have had any of these health problems? Check all that apply: overweight or obese, type 2 diabetes, gestational diabetes (diabetes in pregnancy), high blood pressure, preeclampsia or toxemia, and none of the above.” A binary variable was created for smoking, in which a yes response represents any smoking.
Analysis
Descriptive analyses were used to explore the data by race and obesity categories, and to describe the proportion who endorsed barriers to healthy behaviors. We utilized univariate and multivariate logistic regression models to evaluate for confounders [29]. Age, marital status, English language proficiency, presence of a child under age 5 at home, and education level were included in the model based on our review of the literature. Financial strain was included as the financial variable, rather than income, due to concerns about differential bias as a result of the large percentages of Black (23%) and Hispanic (37%) who declined to answer the question on income.
To evaluate the role of obesity in the relationship between race/ ethnicity and dietary behaviors, we assessed effect modification using stratified samples by BMI ≥ 30 and <30. The rationale was that obesity may be the result of poor dietary behaviors but obese pregnant women may be more likely to receive behavioral counseling and thus make lifestyle changes. While we do not know of any specific data examining the role of race in these behaviors, there is data demonstrating racial and cultural differences in body image [30] which could potentially lead to modification of racial differences fast food and sugar sweetened beverage intake, based on obesity.
We performed two sensitivity analyses. First we limited the sample to include only the pregnant women (n=179) as pregnant and postpartum women may report different behaviors. The percentage of postpartum women was so small (16%), that we were unable to compare these two groups. We compared the results in just pregnant women, to the results in the entire model to assess for differences. Second, we changed the cut-point of sugar-sweetened beverage intake to assess daily not weekly intake, ≥1 versus <11 sugar-sweetened beverage daily and re-evaluated our model
Results
Table 1 shows the characteristics of the 212 women in our sample by race/ethnicity.
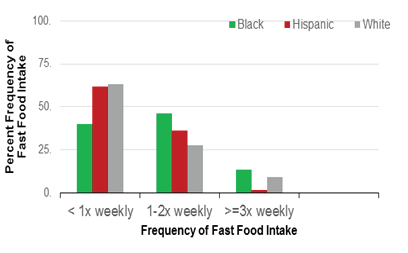
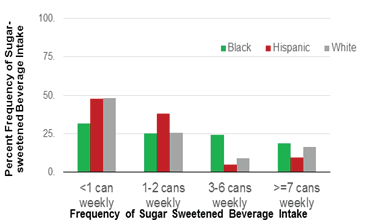
Figures 1a and 1b show the pre-adjustment frequency of fast food (Panel 1) and sugar-sweetened beverage (Panel 2) intake by race/ ethnicity. Overall, 52% of women reported fast food intake less than once weekly or never, 39% reported intake 1-2 times weekly, and 9% reported intake ≥3 times weekly. In terms of sugar-sweetened beverage intake, the plurality (40.6%) reported less than 1 serving weekly, while 29.3% reported 1-2 servings and 14.6% reported 3-6 servings weekly.
Adjusted analyses to assess racial and ethnic differences in the odds of fast food and sugar-sweetened beverage intake
Table 2 shows the results of our adjusted logistic regression models. With respect to fast food intake, black women had 2.38 higher odds of consumption once or more weekly, when compared to White women (CI=1.08, 5.23). We did not detect differences in fast food frequency between Hispanic and White women (CI=0.45, 2.70). Women aged 30-34 had 2.6 times higher odds when compared to women 18-24 years old (CI=1.02, 6.62). There were no other differences in intake by age group. Women reporting financial strain had 1.4 times greater odds of fast food intake than those who did not report financial strain (CI=1.01, 1.93). Women who were married or lived with a partner had 0.4 reduced odds of consuming fast food (CI=0.21, 0.85), when compared to those without a spouse or live-in partner.
| Fast Food Intake ≥1 time weekly |
Sugar Sweetened Beverage Intake ≥1 time weekly |
|
|---|---|---|
| Socio- Demographic Covariates | OR (CI) | OR (CI) |
| Maternal Race, White (REF) | ||
| Black | 2.38 (1.08, 5.23)* | 0.91 (0.38, 2.17) |
| Hispanic | 1.10 (0.45, 2.70) | 0.57 (0.20, 1.49) |
| Maternal Age, 18-24 (REF) | ||
| 25-29 | 1.09 (0.53, 2.25) | 1.08 (0.49, 2.38) |
| 30-34 | 2.60 (1.02, 6.62) | 1.01 (0.39, 2.63) |
| >=35 | 1.03 (0.41, 2.59) | 0.38 (0.15, 0.99) |
| Marital Status | ||
| Married/Living with Partner | 0.43 (0.21, 0.85)* | 0.30 (0.13, 0.68) |
| Child under 5 years old, Yes | 1.20 (0.64, 2.26) | 3.04 (1.54, 6.00) |
| Education | ||
| <Grade 12 | 1.73 (0.74, 4.07) | 1.42 (0.56, 3.59) |
| High school graduate/GED | 1.13 (0.47, 2.73) | 0.52 (0.20, 1.32) |
| ≥1 year college | 1.32 (0.06, 26.9) | 0.27 (0.01, 6.17) |
| Financial Strain, Yes | 1.40 (1.01, 1.93) | 1.04 (0.79, 1.38) |
| Sub-sample with BMI≥30 | n=75 | n=75 |
| Maternal Race, White (REF) | ||
| Black | 0.46 (0.10, 2.00) | 0.28 (0.05, 1.47) |
| Hispanic | 0.27 (0.05, 1.33) | 0.25 (0.04, 1.38) |
| Sub-sample with BMI<30 | n=99 | n=99 |
| Maternal Race, White (REF) | ||
| Black | 4.66 (1.49, 14.5) | 1.85 (0.57, 6.03) |
| White | 1.39 (0.36, 5.33) | 0.71 (0.18, 2.87) |
| Boldface denotes statistical significance; Abbreviations: BMI=Body Mass Index, CI=Confidence Interval, GED=Graduate Equivalency Degree, OR=Odds Ratio, EF=Reference | ||
Table 2: Adjusted odds of fast food and sugar sweetened beverage intake.
In adjusted analyses, we did not detect racial/ethnic differences in sugar-sweetened beverage intake. Compared to those without young children at home, women with a child under age 5 at home were 3.0 times more likely to drink sugar-sweetened beverages once or more weekly (CI=1.54, 6.00). Married women and those living with a partner had reduced odds of drinking sugar-sweetened beverages (OR=0.30, CI=0.13, 0.68) compared with unmarried and single women. Lastly women 35 or older had lower odds of sugar sweetened beverage intake when compared to women 18-24 (CI=0.15 0.99).
In stratified analyses, we did not detect racial/ethnic differences in fast food intake among obese women. However, non-obese Black women had 4.66-fold greater odds of fast food intake once or more weekly, when compared to non-obese White women (CI=1.49, 14.5). There were no significant racial/ethnic differences in sugar-sweetened beverage intake in the stratified obese or non-obese subgroups. Results were otherwise very similar to those seen in the analysis of the entire cohort.
The first sensitivity analysis, in which we excluded postpartum women and examined the adjusted odds of fast food and sugarsweetened beverage intake, showed that Black women had a 2.6 higher odds of fast food intake once or more weekly when compared with white women (CI=1.10, 6.06), confirming our findings from the entire sample. Results were also similar for the other variables (data not shown).
In the second sensitivity analysis, we assessed a daily cut-point for sugar-sweetened beverage intake, comparing the 18% of our sample that reported daily vs. non-daily sugar-sweetened beverage intake. Even with this different cut-point, we confirmed a null association between race and ethnicity and the odds of drinking one or more sugar-sweetened beverages daily.
Discussion
In a cross sectional analysis of 212 pregnant and postpartum women, 47.7% of women reported eating fast food one or more times weekly, but only 1.9% consumed it one or more times daily. In contrast 59% reported drinking one or more sugar sweetened beverages per week, with 15.6% drinking at least one can daily. We found significant racial and ethnic differences in fast food, but not sugar-sweetened beverage, intake. Black women had 2-fold greater odds of fast food intake once or more weekly when compared with White women. The increased strength of the association among non-obese Black women, was interesting in light of previous studies demonstrating that normal and overweight women are at greater risk of excess gestational weight gain, than obese women [2,16]. This emphasizes the need for inclusion of non-obese women in discussions around dietary habits, healthy gestational weight gain, and postpartum weight loss. Our data provides new information about racial differences in dietary behaviors, and highlights the need for interventions to target obesogenic dietary behaviors in pregnancy and postpartum, as failure to lose gestational weight during the first year postpartum is associated with worsened cardiovascular risk markers [31] and overweight at 15 years postpartum [32,33].
Marriage or living with a partner was associated with reduced odds of both fast food and sugar sweetened beverage intake [34-36]. Our finding may represent increased financial means, improved social support, or factors not measured in our study. This data adds new information to existing literature on marriage and pregnancy related health behaviors. Prior data has shown decreased use of tobacco and drugs during pregnancy [34] increased prenatal care [35] and improved pregnancy outcomes [36] among women who have a good relationship with the father of their child, when compared to those without such a relationship.
Financial strain was associated with increased odds of both fast food and sugar sweetened beverage intake when compared with women who did not report financial strain. This finding was expected given that healthier foods are often more expensive and less available in lower income neighborhoods lacking a grocery store with healthy food options. Fast food and sugar sweetened beverages may represent less expensive alternatives to grocery purchased food for low-income families.
The finding that women having children under age 5 in the home were more likely to drink sugar sweetened beverages was counterintuitive. This was especially true given that this conflicted with existing literature demonstrating decreased intake among women with small children in the home. One possible explanation might be parental fatigue, leading to higher intake of caffeinated beverages that contain sugar. Another possible explanation might be having the sugary drinks on hand for children, leading to increased intake on the part of the parent.
The findings of increased fast food intake among women 30-34, and decreased sugar sweetened beverage intake month women 35 and over were unexpected. Further study is needed to confirm and further evaluate these findings.
While the majority of data on postpartum weight loss interventions have focused on middle class White women [37-40] studies in the general population have shown that culturally tailoring interventions can result in significant weight loss in low-income and racial and ethnic minority groups [41-44]. Concern exists, however, that Black women lose less weight than their white counterparts [45] and dropout rates for all participants remain high [40,46]. Several qualitative studies have examined barriers to, and facilitators of healthy lifestyles in pregnant and postpartum populations, and these results should be considered when designing dietary interventions [47-49].
A successful approach to changing high risk dietary behaviours would have culturally tailored interventions, addressing the specific barriers faced by pregnant and postpartum women. Recruitment from trusted community sources may be important for participation [50-52] and may also improve retention. Healthy adaptations of culturally appropriate foods may increase personal and family satisfaction as well as family and social support for weight loss interventions [50-52]. Due to the time constraints faced by pregnant and postpartum women, in person educational interventions, such as guided grocery shopping, should be practical, high-yield, and in a group format to enhance social support. Online follow up can be used to reinforce in person educational activities and provide ongoing motivation. Online formats can also be used for group activities such as meal planning, recipe sharing, and peer support. Concurrent policy initiatives should be employed to complement the clinical interventions, ensuring access to healthier, more affordable foods [53-56] decreasing access to unhealthy foods through taxation [57] as well as insurance reimbursement for successful weight loss programs [58-61].
The major strengths of our study were in the diverse sample of of Black, Hispanic and white participants to evaluate racial and ethnic differences, while controlling for key socioeconomic variables and preconception BMI. This study has several limitations. This was a small study. Our survey was based on a convenience sample. Some groups may have been under or over represented as a result of not using probability samples. We are unable to report how many women declined to participate, or how those who chose to participate differ from those who did not. This can introduce bias; however this also allowed us to evaluate real-world clinical populations. High nonresponse rates occurred with some of our key variables. Higher percentages of Hispanic (41%) and Black (6.5%) women did not answer the self-report question pertaining to pre-conception weight and height, as compared to 1.9% of White women. Hispanic women were also less likely to be insured or have a PCP, which may lead to a lack of knowledge of weight, and preconception medical diagnoses. These results suggest that the preconception rates of overweight and obesity may be higher in both groups than reported. To address this limitation, we compared our results to national survey data on obesity for women age 20-39 years [61] and found similar obesity rates for Black and White women, but underestimated rates for Hispanic women, likely as a result of missing data. Likewise, incomplete responses to certain socioeconomic variables limited their use as covariates in our study. Notably 36.5% of Black women, 23.2% of Hispanic women and 11.1% of White women declined to answer the question about income. We thus used financial strain as a measure of wealth in its stead.
Conclusions
We found significantly increased odds of fast food among pregnant and postpartum Black women when compared to White women, with an even stronger association among non-obese Black women. We found high intake of sugar-sweetened beverages among all women. These results suggest the need for nutritional counselling about fast food intake targeted at Black women, including non-obese women, and about sugar-sweetened beverage intake in all women.
Acknowledgements
Ashley Harris was supported by Hopkins HRSA NRSA Primary Care Health Services Fellowship Training Program T32HP10025BO-20, Behavioural Research in Heart and Vascular Disease Fellowship Training Program T32HL007180-39, and a National Institute of Health Loan Repayment Program Award, Health Disparities Loan Repayment Program, National Institute on Minority Health and Health Disparities. This funding was used to design the study, analyse and interpret the data, prepare, and review the manuscript, as well as the decision to submit the manuscript for publication.
References
- Chu SY, Kim SY, Bish CL (2009) Prepregnancy obesity prevalence in the United States, 2004-2005.Matern Child Health J 13: 614-620.
- Chu SY, Callaghan WM, Bish CL, D'Angelo D (2009) Gestational weight gain by body mass index among US women delivering live births, 2004-2005: fueling future obesity.Am J ObstetGynecol 200: 271.
- Ogden CL, Yanovski SZ, Carroll MD, Flegal KM (2007) The epidemiology of obesity.Gastroenterology 132: 2087-2102.
- Metzger BE, Buchanan TA, Coustan DR, de Leiva A, Dunger DB, et al. (2007) Summary and recommendations of the Fifth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 30: S251-260.
- Wallis AB, Saftlas AF, Hsia J, Atrash HK (2008) Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987-2004.Am J Hypertens 21: 521-526.
- Sibai BM (2003) Diagnosis and management of gestational hypertension and preeclampsia.ObstetGynecol 102: 181-192.
- Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, et al. (2006) Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002.Diabetes Care 29: 1263-1268.
- Gillespie CD, Hurvitz KA; Centers for Disease Control and Prevention (CDC) (2013) Prevalence of hypertension and controlled hypertension - United States, 2007-2010. MMWR pp: 144-148.
- 9. Go AS, Mozaffarian D, Roger VS, Benjamin EJ (2014) on behalf of the American Heart Association Statistics Committee and Stroke Statsitics Subcommittee. Heart disease and stroke statistics -2014 update: a report from the American Heart Association. Circulation 129: e28-e292
- Mamun AA, Kinarivala M, O'Callaghan MJ, Williams GM, Najman JM, et al. (2010) Associations of excess weight gain during pregnancy with long-term maternal overweight and obesity: evidence from 21 y postpartum follow-up.Am J ClinNutr 91: 1336-1341.
- Oken E, Kleinman KP, Belfort MB, Hammitt JK, Gillman MW (2009) Associations of gestational weight gain with short- and longer-term maternal and child health outcomes.Am J Epidemiol 170: 173-180.
- 12. Volgyi E, Carroll KN, Hare ME, Ringwald-Smith K (2013) Dietary patterns in pregnancy and effects on nutrient intake in the mid-South: The conditions affecting neurocognitive development and learning in early childhood (CANDLE) study. Nutrients 5: 1511-1530.
- Esperat C, Du Feng, Zhang Y, Owen D (2007) Health behaviors of low-income pregnant minority women.West J Nurs Res 29: 284-300.
- Kominiarek MA (2014) A survey of health behaviors in minority women in pregnancy: the influence of body mass index.Womens Health Issues 24: e291-295.
- Laraia BA, Bodnar LM, Siega-Riz AM (2007) Pregravid body mass index is negatively associated with diet quality during pregnancy.Public Health Nutr 10: 920-926.
- Rothberg BEG, Magriples U, Kershaw TS (2011) Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. American Journal of Obstetrics and Gynecology 204:e1-e11.
- Duffey KJ, Gordon-Larsen P, Shikany JM, Guilkey D, Jacobs DR Jr, et al. (2010) Food price and diet and health outcomes: 20 years of the CARDIA Study.Arch Intern Med 170: 420-426.
- Pereira MA, Kartashov AI, Ebbeling CB, Van Horn L, Slattery ML, et al. (2005) Fast-food habits, weight gain, and insulin resistance (the CARDIA study): 15-year prospective analysis.Lancet 365: 36-42.
- Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, et al. (2004) Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women.JAMA 292: 927-934.
- (2006) Coronary Artery Risk Development in Young Adults (CARDIA).
- Behavioral risk factor surveillance system (2013) Centers for Disease Control and Prevention.
- (2005) HRSA My bright future: Physical activity & healthy eating for adult women.
- (1998) Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults-The Evidence Report. National Institutes of Health.Obes Res 6: 51S-209S.
- Obesity: preventing and managing the global epidemic. Report of a WHO consultation.World Health Organ Tech Rep Ser 894: 1-253.
- Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB (2011) Changes in diet and lifestyle and long-term weight gain in women and men.N Engl J Med 364: 2392-2404.
- de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, et al. (2012) Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation 125: 1735-1741.
- Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, et al. (2009) Sweetened beverage consumption and risk of coronary heart disease in women.Am J ClinNutr 89: 1037-1042.
- Shin H, Bruno R (2000) Language use and English-speaking ability. United States Census 2000, US Census Bureau.
- Bliss R, Weinberg J, Vieira V, Webster T (2011) Detecting Confounding and Evaluating the 10% Rule. Joint Statistical Meetings. Brigham and Women√ʬ?¬?s Hospital and Boston University School of Public Health.
- Le YC, Rahman M, Berenson AB (2010) Perceived weight gain as a correlate of physical activity and energy intake among white, black, and Hispanic reproductive-aged women.J Womens Health (Larchmt) 19: 1987-1993.
- Kew S, Ye C, Hanley AJ, Connelly PW, Sermer M (2014) Cardiometabolic implications of postpartum weight changes in the first year after delivery.Diabetes Care 37: 1998-2006.
- R√?¬∂ssner S (1992) Pregnancy, weight cycling and weight gain in obesity.Int J ObesRelatMetabDisord 16: 145-147.
- Linn√?¬© Y, Dye L, Barkeling B, R√?¬∂ssner S (2004) Long-term weight development in women: a 15-year follow-up of the effects of pregnancy.Obes Res 12: 1166-1178.
- Bloch JR, Webb DA, Mathew L, Dennis EF, Bennett IM, et al. (2010) Beyond marital status: the quality of the mother-father relationship and its influence on reproductive health behaviors and outcomes among unmarried low income pregnant women.Matern Child Health J 14: 726-734.
- Teitler J (2001) Father Involvement, child health and maternal healthbehavior. Child Youth Serv Rev 23: 403-425.
- Padilla Y, Reichman NE (2001) Low birthweight: Do unwed fathers help? Child Youth Serv Rev 23: 427-452.
- Colleran HL, Lovelady CA (2012) Use of MyPyramid Menu Planner for Moms in a weight-loss intervention during lactation.J AcadNutr Diet 112: 553-558.
- Davenport MH, Giroux I, Sopper MM, Mottola MF (2011) Postpartum exercise regardless of intensity improves chronic disease risk factors.Med Sci Sports Exerc 43: 951-958.
- Dewey KG, Lovelady CA, Nommsen-Rivers LA, McCrory MA, L√?¬∂nnerdal B (1994) A randomized study of the effects of aerobic exercise by lactating women on breast-milk volume and composition.N Engl J Med 330: 449-453.
- Leermakers EA, Anglin K, Wing RR (1998) Reducing postpartum weight retention through a correspondence intervention.Int J ObesRelatMetabDisord 22: 1103-1109.
- Stolley MR, Fitzgibbon ML, Schiffer L, Sharp LK, Singh V, et al. (2009) Obesity reduction black intervention trial (ORBIT): six-month results.Obesity (Silver Spring) 17: 100-106.
- Svetkey LP, Stevens VJ, Brantley PJ, Appel LJ, Hollis JF, et al. (2008) Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial.JAMA 299: 1139-1148.
- Faucher MA, Mobley J (2010) A community intervention on portion control aimed at weight loss in low-income Mexican American women.J Midwifery Womens Health 55: 60-64.
- Weerts SE, Amoran A (2011) Pass the fruits and vegetables! A community-university-industry partnership promotes weight loss in African American women.Health PromotPract 12: 252-260.
- West DS, Prewitt TE, Bursac Z, Felix HC (2008) Weight loss of black, white, and Hispanic men and women in the Diabetes Prevention Program.Obesity (Silver Spring) 16: 1413-1420.
- O'Toole ML, Sawicki MA, Artal R (2003) Structured diet and physical activity prevent postpartum weight retention.J Womens Health (Larchmt) 12: 991-998.
- √?¬?stbye T, Krause KM, Brouwer RJ, Lovelady CA, Morey MC, et al (2008) Active Mothers Postpartum (AMP): rationale, design, and baseline characteristics.J Womens Health (Larchmt) 17: 1567-1575.
- Hoedjes M, Berks D, Vogel I (2008) Motivators and barriers to a healthy postpartum lifestyle in women at increased cardiovascular and metabolic risk: a focus group study.
- Carter-Edwards L, √?¬?stbye T, Bastian LA, Yarnall KS, Krause KM, et al (2009) Barriers to adopting a healthy lifestyle: insight from postpartum women.BMC Res Notes 2: 161.
- Nicklas JM, Zera CA, Seely EW, Abdul-Rahim ZS, Rudloff ND, et al (2011) Identifying postpartum intervention approaches to prevent type 2 diabetes in women with a history of gestational diabetes.BMC Pregnancy Childbirth 11: 23.
- Parikh P, Simon EP, Fei K, Looker H, Goytia C, et al. (2010) Results of a pilot diabetes prevention intervention in East Harlem, New York City: Project HEED. Am J Public Health 100: S232-239.
- Langellier BA, Garza JR, Prelip ML, Glik D, Brookmeyer R, et al. (2013) Corner Store Inventories, Purchases, and Strategies for Intervention: A Review of the Literature.Calif J Health Promot 11: 1-13.
- Cavanaugh E, Green S, Mallya G, Tierney A, Brensinger C, et al. (2014) Changes in food and beverage environments after an urban corner store intervention.Prev Med 65: 7-12.
- Gittelsohn J, Suratkar S, Song HJ (2010) Process evaluation of Baltimore healthy stores: A pilot health intervention program with supermarkets and corner stores in Baltimore City. Health Promotion Practice 11: 723-732.
- Shin A, Surkan PJ, Coutinho AJ, Suratkar SR, Campbell RK, et al (2015) Impact of Baltimore Healthy Eating Zones: an environmental intervention to improve diet among African American youth.Health EducBehav 42: 97S-105S.
- Meyer KA, Guilkey DK, Ng SW, Duffey KJ, Popkin BM, et al (2014) Sociodemographic differences in fast food price sensitivity.JAMA Intern Med 174: 434-442.
- Batsis JA, Huyck KL, Bartels SJ (2015) Challenges with the Medicare obesity benefit: practical concerns & proposed solutions.J Gen Intern Med 30: 118-122.
- Slusser W, Staten K, Stephens K (2001) Payment for obesity services: Examples and recommendations for Stage 3 comprehensive multidisciplinary intervention programs for children and adolescents. Pediatrics 128: S78-85.
- Ades PA (2015) A lifestyle program of exercise and weight loss is effective in preventing and treating type 2 diabetes mellitus: Why are programs not more available?Prev Med 80: 50-52.
- Herman WH, Hoerger TJ, Brandle M, Hic ks K, Sorensen S, et al. (2005) The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance.Ann Intern Med 142: 323-332.
- Ogden CL, Carroll MD, Flegal KM (2014) Prevalence of obesity in the United States.JAMA 312: 189-190.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11161
- [From(publication date):
April-2016 - Jul 01, 2025] - Breakdown by view type
- HTML page views : 10231
- PDF downloads : 930