Research Article Open Access
Obesity Treatment in Children with Intellectual Impairment: Outcome of a Multidisciplinary Inpatient Program
Verreussel MJT1, Dieleman JP2, Rasenberg S1, Veen-Roelofs J1 and van Baak MA3*1De Hondsberg, Koraalgroep, Oisterwijk, The Netherlands
2Maxima Medisch Centrum, Veldhoven, The Netherlands
3Department of Human Biology, NUTRIM School of Nutrition and Translational Research in Metabolism, Maastricht University, Maastricht, The Netherlands
- *Corresponding Author:
- Prof. Dr. van Baak MA, MD
Department of Human Biology
NUTRIM School of Nutrition and Translational Research in Metabolism
Maastricht University, P.O. Box 616
6200-MD, Maastricht, The Netherlands
Tel: +31 43 3881630
Fax: +31 43 3690976
E-mail: m.vanbaak@maastrichtuniversity.nl
Received date: October 26, 2016; Accepted date: December 06, 2016; Published date: December 09, 2016
Citation: Verreussel MJT, Dieleman JP, Rasenberg S, Veen-Roelofs J, van Baak MA (2016) Obesity Treatment in Children with Intellectual Impairment: Outcome of a Multidisciplinary Inpatient Program. J Obes Weight Loss Ther 6:328. doi: 10.4172/2165-7904.1000328
Copyright: © 2016 Verreussel MJT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Obesity & Weight Loss Therapy
Abstract
Background: Obesity is common in children and adolescents with intellectual impairment. In this study the effects of an inpatient multidisciplinary weight control program on BMI-SDS, body weight and BMI in children and adolescents with overweight/obesity and intellectual impairment with or without behavioural problems were evaluated.
Methods: 101 overweight and obese children/adolescents with intellectual impairment with or without behavioural problems that were referred to an inpatient obesity treatment programme were included. The treatment was planned to last 9 months, but could be shortened or extended on an individual basis (mean 355 d, range 95 to 761 d). Data on age, sex, height, body weight and BMI were collected at entry and at the end of treatment.
Results: Initial BMI-SDS was 3.9 ± 0.9 (range 2.0 to 8.4). BMI-SDS was reduced by -1.4 ± 0.7 (P<0.001). Age, gender and the presence of psychiatric disorders did not affect treatment outcome. Being of non-Dutch ethnic origin had a negative effect on the change in BMI-SDS (P=0.029) and longer treatment duration was associated with a larger reduction in BMI-SDS (P=0.002).
Conclusions: The treatment program was effective in obtaining substantial and clinically relevant weight reduction in an inpatient setting in children with intellectual impairment with or without behavioural/psychiatric problems with different causes of obesity.
Keywords
Children/Adolescents; Obesity; Treatment; Mental disability/Impairment/Retardation
Introduction
In the general population, 15% of people have an IQ between 50 and 85. A higher rate of overweight and obesity is found in this specific group with intellectual impairment, also among children [1-4]. Adolescents with intellectual disabilities were recently estimated to be 1.8 times more at risk for obesity than typically developing adolescents [5]. Interestingly, within this group not only lifestyle-related but also genetic causes of overweight and obesity often occur [6].
Multiple intervention programs aiming at weight control are available for children and adolescents [7], but there is less attention for children and adolescents with intellectual impairment with or without behavioural problems. Institute De Hondsberg in the Netherlands addresses the complex problems of the young with intellectual impairment (IQ 50-85) and has built up expertise regarding behavioural, psychiatric and eating disorders in this group of children in an inpatient setting. To reduce weight in such children with obesity, a specialized treatment program was developed. The program is a combination of dietary energy restriction, a behaviour modification program, and an individual exercise program, with participation of all caretakers in- and outside the institute. This study evaluated the effect of this program on body weight of overweight and obese children and adolescents with intellectual impairment in an inpatient setting.
Methods
Participants
Between 2001 and 2011, 101 consecutive overweight/obese children and adolescents with intellectual impairment referred to De Hondsberg were included in the study. Referral of children for treatment at the institute was by general practitioners, pediatricians and associations caring for disabled children. All children had previously been treated for obesity without success. They had an intellectual impairment (IQ 50-70 or 70-85 with limitations in adaptive behaviour [8]) and were overweight or obese. Overweight was defined as Body Mass Index Standard Deviation Score (BMI-SDS) >1.1 or BMI above the reference curve of 25 kg/m2 and obesity as BMI-SDS >2.3 or BMI above the reference curve of 30 kg/m2 [9,10]. Children were classified as morbidly obese when their SDS-BMI was >3.0 or >2.3 with obesity-related co-morbidity 10. Also children with concomitant psychiatric disorders (ADHD, autism), weight problems due to medication and/or a genetic disorder were included in this study. Two (morbidly) obese children with a MC4R gene defect but with an IQ>85 (90 and 94 respectively) were also included. Pregnancy was an exclusion criterion.
The study was performed according to the Dutch Gedragscode Gezondheidsonderzoek (Federa 2004: https://www.federa.org/codegoed-gedrag), which a.o. means that parents/caregivers signed for the use of the files for scientific purposes and data were analysed anonymously.
Study setting
The study was performed in a specialized center for treatment of children with intellectual impairments. Children included in this study were, during their treatment, part of an inpatient orthopedagogic treatment group consisting of 10 children and/or adolescents. Aim of the treatment was to teach the children to adapt a healthier eating pattern, obtain a more healthy weight, to improve physical fitness and to stimulate involvement of parents. A multidisciplinary team, consisting of a dietician, psychologist, paediatrician, social worker, family coach and fitness instructor, and - if necessary - a psychiatrist and psychomotor therapist, was involved in the treatment. During their stay in the treatment center children went to a specialized school. Children went home during weekends (once every 2 weeks in the beginning of the program, each weekend after 3 months). School holidays were also partly spent at home.
Study design
This was an observational study. Participants, care takers, health professionals and investigators involved in the study were not blinded to the treatment for obvious reasons. Treatment duration was 9 months, but could be shortened or lengthened on an individual basis.
Data on age, sex, height, and weight were collected by a trained staff member at baseline, before starting multidisciplinary treatment, and shortly before dismissal.
Measurements
All anthropometric measurements were done in the morning, with children only wearing their underwear. A standard calibrated digital scale and a wall-mounted stadiometer were used to determine weight to the nearest 0.05 kg and height to the nearest 0.1 cm. BMI-SDS was calculated using Dutch growth charts and the web-based program Growth Analyser (https://groeiweb.pgdata.nl/calculator.asp), which contains age and sex specific data from the Fifth Dutch Growth Study [11].
Treatment program
The treatment consisted of four elements: 1) energy restriction, 2) behavior modification, 3) individual exercise program and 4) participation of all caretakers [12].
Energy restriction: The individually estimated energy need, which was based on height (15 kcal/cm) [13], was the basis of the dietary programme. For children with genetic defects characterized by low metabolic rate the energy requirement was reduced to 10-11 kcal/cm. This individual energy need was visualized for each child by a corresponding number of dots (each dot representing 25 kcal) on so called “dot cards”. A number of green or orange colored dots were awarded to all foods, depending on nutritional composition. To assist in choosing more healthy food options, more healthy foods (less energy dense and/or more healthy ingredients) obtain green dots and less healthy foods (more energy dense and/or less healthy ingredients) orange dots. In contrast to the traffic light method, there were no forbidden foods, so the color red was absent. Meal and snack times and the type of food products eaten at these specific times and the associated number and color of dots were visualized on special cards. At each meal and snack moment, the dot cards were filled in and the youngsters learned to choose the amount and composition of their meals and snacks based on the number and color of the dots.
Eating moments (meals and snacks) were standardized during the day. Evening meals were prepared in a central kitchen, but a (limited) choice for the food items in the evening meal was still possible. Total daily energy intake of each child had to remain within the maximum number of dots on his or her individual dot card, but individual preferences were accommodated in order to stimulate long-term adherence.
Behaviour modification: Eating habits were addressed by introduction of learning principles by cognitive behavioural therapy, using a personal contract followed by rewards. Step by step the participants learned to choose more optimal dietary components with a competency-based approach. This meant that the child, depending on his/her level and the phase of the program, could choose more independently and/or was given more choices. At the start, children exactly followed a sample menu for 2 weeks, followed by a gradual increase in own choices.
Exercise program: For all participants an individual exercise program was constructed by a professional exercise instructor. Each child was encouraged to exercise at least half an hour per day at moderate intensity. Some children preferred exercising in groups, others chose an individual sport. Individual preferences were accommodated as much as possible in order to stimulate long-term adherence. If necessary, the child could be coached by a psycho-motor therapist. Apart from this the children were encouraged to be physically active throughout the day, especially after each meal. The activities were monitored on a physical activity card. Good behaviour was praised and documented on a reward card.
Participation of all caretakers: The approach was system-based, i.e. the social network of the child was involved in the treatment. Together with caretakers and the child the possibilities for the best possible result were discussed (solution-oriented approach). Active participation of all caretakers is needed to stimulate the participant. The family was visited by a social worker or family coach if needed. Also cooking and shopping lessons for parents were introduced. The same procedure was used in school or at work by teaching the school caretakers.
Statistical analysis
The change in BMI-SDS was the primary outcome. In addition changes in weight and BMI were analysed. Baseline values are expressed as mean ± SD and treatment effects as means ± 95% confidence intervals. With linear regression analysis we tested for factors that significantly influenced the change in BMI-SDS. A P value<0.05 was considered statistically significant.
Results
Participant characteristics at baseline
Baseline characteristics of the inpatient population are shown in Table 1. Eighty-seven participants (88%) were morbidly obese, 3 (3%) were overweight and the remaining group (10%) was obese. Among them were 12 children (6 girls, 6 boys) with Prader-Willi syndrome, 1 girl with Bardet-Biedl syndrome, 2 boys with a (1 homozygous, 1 heterozygous) MC4R gene defect, 1 boy with an XYY chromosome pattern and 1 girl with a small duplication of chromosome 2q31.3 with unknown clinical relevance. Besides genetic causes, there were illnesses causing obesity: 1 boy was known with hypothalamic dysfunction after removal of a brain tumor, 1 boy was being treated for hypothyroidism. The remaining group had no specific obesity-related genetic or endocrine disorders. Seventy-two of the participants had a concomitant behavioural and/or psychiatric diagnosis (9 ADHD, 15 ASS, 23 other (such as PTSS, NLD, dysthymic disorder, anxiety disorder, depression and others). Behavioural problems were present in 50 children. 71 children were of Dutch descent, 13 were Turkish, 6 Moroccan and 11 were of Antillean or other descent. There was no correlation between IQ and level of obesity.
| Characteristics | Total group (N=101) | Boys (N=44) | Girls (N=57) | Prader-Willi syndrome (N=12) | BardetBiedlsyndrome (N=1) | MC4R genedefect (N=2) |
|---|---|---|---|---|---|---|
| Age (years) | 13.7 ± 3.2 | 13.8 ± 3.1 | 13.7 ± 3.4 | 10.8 ± 3.4 | 14 | 10.1; 14.9 |
| BMI-SDS | 3.9 ± 0.9 | 4.0 ± 1.0 | 3.8 ± 0.8 | 3.9 ± 1.1 | 2.9 | 8.4; 2.6 |
| BMI (kg/m2) | 36.5 ± 8.5 | 35.5 ± 8.1 | 37.2 ± 8.8 | 34.2 ± 11.2 | 29.3 | 36.6; 23.7 |
| Weight (kg) | 97.3 ± 31.4 | 94.9 ± 34.4 | 99.2 ± 29.1 | 68.9 ± 27.3 | 66.2 | 48.8; 51.2 |
| IQ | 69.6 ± 13.4 | 68.9 ± 14.4 | 70.1 ± 12.7 | 50.6 ± 3.6 | 52 | 90; 94 |
| Behavioural and/or psychiatric problem(s) | 73 | 32 | 41 | 7 | 1 | 1 |
Table 1: Baseline characteristics of the included children and adolescents (mean ± SD or individual values or number).
Average length of stay was 355 days, range 95 to 761 days. 23 children left the institution before 9 months for various reasons (e.g. young age, motivational problems, vacation, problems with implementation of the program in the home environment, treatment for psychiatric disorders in another setting). 37 children (9 with Prader-Willi syndrome) stayed longer than 12 months because of difficulties in placing them back in the home environment. In none of these cases the amount of weight loss was the reason for a shorter or longer stay. Because food intake in the institution was largely supervised, compliance during the week was high. No data on food intake during the weekends at home or during holidays away from the institution was collected.
Intervention outcomes
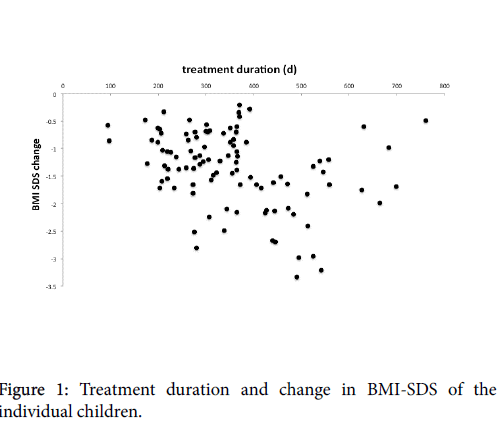
BMI-SDS: Initial BMI-SDS was 3.9 ± 0.9 (range 2.0 to 8.4). BMISDS was reduced significantly (mean -1.4 (95% CI -1.5 to -1.2), P<0.001) (range -0.2 to -3.3) (Table 2). Participants with Prader-Willi syndrome had a similar rate of weight reduction. Their mean BMI-SDS was reduced from 3.9 ± 1.1 to 2.2 ± 1.4 (P<0.001). Age, gender and the presence of psychiatric and/or behavioural disorders did not affect the treatment outcome significantly. Being of non-Dutch origin had a negative effect on the change in BMI-SDS (P=0.029). A longer treatment duration was associated with more reduction in BMI-SDS (P=0.002) (Figure 1).
| Variable | change from baseline | P value |
|---|---|---|
| BMI-SDS | -1.4 (-1.5 to -1.2) | <0.001 |
| BMI (kg/m2) | -8.5 (-9.3 to -7.6) | <0.001 |
| Body weight (kg) | -20.7 (-23.1 to -18.3) | <0.001 |
Table 2: Changes in anthropometric variables from baseline to the end of treatment (mean (95% confidence interval)).
Weight and BMI
Initial weight was 97.3 ± 3.2 kg (range 37.0 kg to 184.8 kg). Average weight reduction for the entire group of patients was -20.7 kg (95%CI -23.1 to -18.3, P<0.001) (range +0.3 to -55.7 kg) (Table 2). Initial BMI was 36.5 ± 8.5 kg/m2 (range 19.7 kg/m2 to 68.7 kg/m2). Average BMI reduction was -8.4 kg/m2 (95% CI -9.3 to -7.6, P<0.001) (range -1 kg/m2 to -20.7 kg/m2) (Table 2).
Adverse effects
There were no major side effects during treatment, but in some participants with huge weight loss surplus of abdominal skin remained. Another adverse effect of the inpatient program was homesickness. This resulted in premature departure from the institution in 2 children. Two girls tried to commit suicide: one because of her underlying psychiatric disorder, the second because of severe psychotic periods known in Prader-Willi syndrome. Both children were treated by a psychiatrist. Nevertheless they showed considerable weight loss (body weight -26.3 kg, BMI-SDS -1.3 and body weight -16.8 kg, BMI-SDS -1.7 respectively).
Discussion
To our knowledge this is the first study investigating inpatient treatment results in obese children and adolescents with intellectual impairment. The results of this study show that the treatment program was effective in reducing BMI-SDS, BMI and body weight in intellectual impaired participants with overweight or obesity. Age, gender and the presence of psychiatric disorders did not affect the treatment outcome significantly. As to be expected, treatment duration was positively associated with the reduction of BMI-SDS. Being of non-Dutch descent had a negative effect on the change in BMI-SDS.
As far as we are aware, no data on inpatient obesity treatment programs in children and adolescents with intellectual disabilities have been reported. Maïano et al. recently reviewed the impact of outpatient lifestyle interventions targeting changes in body weight in youth with intellectual disability [14]. The findings were suggestive of positive effects of such interventions on weight loss. However, most of the reviewed studies were small, were of limited duration and mostly focussed on increased physical activity alone [14].
A number of studies have evaluated the effectiveness of inpatient treatment progams in obese children with normal cognitive function [15-18]. In the study by Van der Baan-Slootweg et al. [18] evaluating an intensive inpatient life-style program for children with obesity and normal cognitive function and without significant behavioural/ psychiatric problems the decline in BMI-SDS was -0.7 compared to -1.4 in our study. However, the average stay at the institution in our study was longer than the stay in the other treatment centre (9-12 vs. 6 months respectively). Since treatment outcome in our study was significantly associated with treatment duration, these results are not entirely comparable. Braet et al. found an average BMI reduction of -48% after 10 months of intervention [15]. Rolland-Cachera et al. reported a mean BMI-SDS reduction of -1.7 ± 0.6 after 10 months intervention [17]. Dao et al. found a mean BMI reduction in boys of -9 kg/m2 and in girls of -10 kg/m2 after 6-12 months of treatment [16].
In our study children from families of non-Dutch descent did less well than children from Dutch families. The impression was that parents from families of non-Dutch ethnical background were less supportive of the eating and physical activity behaviour requirements of the treatment program when the children were at home, even though they were given additional advice when their child showed weight gain after a stay at home. Less positive obesity treatment results in ethnic minorities is a common finding and may be related to socioeconomic, educational, cultural and communication issues [19].
Although not systematically measured as a secondary outcome, improvements in quality of life were almost always mentioned in the data records: after weight reduction the children showed more selfesteem and the entire group moved more easily and their condition was markedly better. Participants with obstructive sleep apnoea syndrome (1 girl, 1 boy) were able to breathe without support during night.
An obvious limitation of this study is the lack of a control group. However, previous (outpatient) attempts to lower body weight in these children in the regular health care system had not been effective.
Unfortunately, currently no follow-up data of the children in this study after treatment are available. Several studies in children and adolescents with normal cognitive function reported long-term followup data after an inpatient obesity treatment [20,21]. Approximately one-third of the SDS-BMI loss was regained one year after the end of the treatment program, but loss to follow-up was large in both studies [20,21]. When comparing the long-term effects of in- and outpatient treatment programs, equivocal results are found, despite initially better weight loss in the inpatient group [18,22]. Such data are not available for children and adolescents with intellectual disabilities. Especially for some categories of such children (e.g. with Prader-Willi syndrome or MC4R disorder) ongoing inspiring supervision is necessary because of their food obsession. On the other hand autism seems helpful because these children will continue to repeat gathered skills. For all children continued understanding and support is obligatory, especially at home where food is often too easily available. These children need lifelong support with coaching by parents, teachers and other caretakers. In this respect, parents and caretakers from ethnic minorities may require extra attention.
Conclusion
This is the first study on the results of an inpatient multidisciplinary obesity treatment program for overweight and obese children and adolescents with intellectual impairment. The data demonstrate that such a program is effective in attaining a substantial and clinically relevant reduction of body weight in these children and adolescents, also in those with obesity due to a single gene defect. Obesity in combination with psychiatric or behavioural problems in this target group is common, but in this study psychiatric or behavioural problems did not have a negative effect on treatment results.
Acknowledgements
The study was funded by De Hondsberg, the Netherlands.
Conflict of interest
JV is owner of the Happy Weight Stippenplan, the commercial follow-up of the program used in this study. The other authors report no conflict of interest.
References
- De S, Small J, Baur LA (2008) Overweight and obesity among children with developmental disabilities. J Intellect DevDisabil 33: 43-47.
- Maïano C (2010) Prevalence and risk factors of overweight and obesity among children and adolescents with intellectual disabilities. Obes Rev 12: 189-197.
- Neter JE, Schokker DF, de Jong E, Renders CM, Seidell JC, et al. (2011) Theprevalence of overweight and obesity and its determinants in children with and without disabilities. J Pediatr 158: 735-739.
- Goldberg S, Werbeloff N, Fruchter E, Portuguese S, Davidson M, et al. (2014) IQ and obesity in adolescence: a population-based, cross-sectional study. PediatrObes 9: 419-426.
- Maïano C, Hue O, Morin AJS, Moullec G (2016) Prevalence of overweight and obesity among children and adolescents with intellecual disabilities: a systematic review and meta-analysis. Obes Rev 17: 599-611.
- O'Rahilly S, Farooqi IS (2006) Genetics of obesity. Phil Trans Royal Soc London B BiolSci 361: 1095-1105.
- Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, et al. (2006)Interventions for treating obesity in children. Cochr Database Syst Rev CD001872.
- Schalock RL, Borthwick-Duffy SA, Bradley VJ, Buntinx WHE, Coulter DL, et al. (2010) Intellectual disability: diagnosis, classification and systems of supports. (11th edn), AAIDD, Washington DC, USA.
- Cole TJ, Bellizi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. Brit Med J 320: 1240-1243.
- Van der Baan-Slootweg OH, Nollet MN, Weller FR, Benninga MA,van Aalderen WMC (2010) Severe childhood obesity: a question of weight. TijdschrKindergeneesk 78: 106-113.
- Schönbeck Y, Talma H, van Dommelen P, Bakker P, Buitendijk SE, et al. (2011) Increase in prevalence of overweight in Dutch children and adolescents: a comparison of nationwide growth studies in 1980, 1997 and 2009. PlosOne 6: e27608.
- Descheemaeker MJ, Swillen A, Pissart L, Borghgraef M, Rasenberg S, et al. (1994) The Prader-Willi syndrome: a self supporting program for children, youngsters and adults. Genet Couns 5: 199-205.
- Culley WJ, Middleton TO (1969) Caloric requirements of mentally retarded children, with and without motor dysfunction. J Pediatr 75: 380-384.
- Maïano C, Normand CL, Aimé A, Bégarie J (2014) Lifestyle interventions targeting changes in body weight and composition among youth with an intellectual disability: a systematic review. Res DevDisabil 35: 1914-1926.
- Braet C, Tanghe A, Bode PD, Franckx H, Winckel MV (2003) Inpatient treatment of obese children: a multicomponent programme without stringent caloric restriction. Eur J Pediatr 162: 391-396.
- Dao HH, Frelut ML, Oberlin F, Peres G, Bourgeois P, et al. (2004) Effects of a multidisciplinairy weight loss intervention on body composition in obese adolescents. Int J Obes 28: 290-299.
- Rolland-Cachera MF, Thibault H, Souberbielle JC, Soulié D, Carbonel P, et al. (2004) Massive obesity in adolescents: dietary interventions and behaviours associated with weight regain at 2 y follow-up. Int J Obes 28: 514-519.
- Van der Baan-Slootweg OH, Benninga MA, Beelen A, van der Palen J, Tamminga-Smeulders C, et al. (2014) Inpatient treatment of children and adolescents with severe obesity in the Netherlands. A randomized clinical trial.JAMA Pediatr 168: 807-814.
- Lewis KH, Edwards-Hampton SA, Ard JD (2016) Disparities in treatment uptake and outcomes of patients with obesity in the USA. CurrObes Rep 5: 282-290.
- Halberstadt J, van Strien T, de Vet E, Eekhout I, Braet C, et al. (2016) The association of eating styles with weight change after an intensive combined lifestyle intervention for children and adolescents with severe obesity. Appetite 99: 82-90.
- Rank M, Wilks DC, Poley L, Jiang Y, Langhof H, et al. (2014) Health-related quality of life and physical activity in children and adolescents 2 years after an inpatient weight-loss program. J Pediatr 165: 732-737.
- Rank M, Siegrist M, Wilks DC, Haller B, Wolfarth B, et al. (2012) Long-term effects of an inpatient weight-loss program in obese children and the role of genetic predisposition – rationale and design of the LOGIC-trial. BMC Pediatr 12: 30.
Relevant Topics
- Android Obesity
- Anti Obesity Medication
- Bariatric Surgery
- Best Ways to Lose Weight
- Body Mass Index (BMI)
- Child Obesity Statistics
- Comorbidities of Obesity
- Diabetes and Obesity
- Diabetic Diet
- Diet
- Etiology of Obesity
- Exogenous Obesity
- Fat Burning Foods
- Gastric By-pass Surgery
- Genetics of Obesity
- Global Obesity Statistics
- Gynoid Obesity
- Junk Food and Childhood Obesity
- Obesity
- Obesity and Cancer
- Obesity and Nutrition
- Obesity and Sleep Apnea
- Obesity Complications
- Obesity in Pregnancy
- Obesity in United States
- Visceral Obesity
- Weight Loss
- Weight Loss Clinics
- Weight Loss Supplements
- Weight Management Programs
Recommended Journals
Article Tools
Article Usage
- Total views: 3201
- [From(publication date):
December-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 2376
- PDF downloads : 825