Research Article Open Access
Obesity is a Risk Factor for Erosive Gastroesophageal Reflux Disease: Prospective Case-Control Study
Nicola de Bortoli1*, Guido Salvetti2, Lorenzo Bertani1, Irene Martinucci1, Edoardo Savarino3, Paola Fierabracci2, Roberta Jaccheri2, Jacopo Vitti2, Andrea Pucci2, Massimo Bellini1, Linda Ceccarelli1, Salvatore Russo1, Riccardo Franchi1, Solito Biagio4, Santi Stefano4, Marco Anselmino5, Ferruccio Santini2 and antino Marchi11Division of Gastroenterology, Department of Translational Research and New Technology in Medicine, University of Pisa, Pisa, Italy
2Obesity Center, Department of Internal Medicine, University of Pisa, Pisa, Italy
3Division of Gastroenterology, Department of Surgery, Oncology and Gastroenterology, University of Padua, Padua, Italy
4Division of Esophageal Surgery, Department of Gastroenterology, AOU Pisana, Pisa, Italy
5Division of Bariatric Surgery, Department of Gastroenterology, AOU Pisana, Pisa, Italy
- *Corresponding Author:
- Nicola de Bortoli
Gastroenterology Unit
Department of Translational Research and New Technology
University of Pisa, Italy
Cisanello Hospital, Via Paradisa 2 – 56124 Pisa (PI) – Italy
Tel: +39 050 997395
Fax: +39 050 997398
E-mail: nick.debortoli@gmail.com
Received date: June 06, 2014; Accepted date: June 17, 2014; Published date: June 25, 2014
Citation: Bortoli N, Salvetti G, Bertani L, Martinucci I, Savarino E, et al. (2014) Obesity is a Risk Factor for Erosive Gastroesophageal Reflux Disease: Prospective Case-Control Study. J Gastroint Dig Syst 4:194. doi:10.4172/2161-069X.1000194
Copyright: © 2014 Bortoli ND, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background and aim: An association between high body mass index (BMI) and gastroesophageal reflux disease (GERD) has been proposed but the relationship between the severity of obesity, the prevalence of symptoms and gravity of esophagitis is still unclear. Aim of this study was to evaluate the prevalence of symptomatic GERD and esophagitis in female obese subjects compared to a group of female with typical GERD symptoms. Material and methods: 193 obese women (Group A) scheduled for bariatric surgery and 193 normal weight female with typical GERD symptoms (Group B) were submitted to complete history (recording voluptuary habits) and validated questionnaire for symptomatic diagnosis of GERD (GIS: GERD Impact Scale). Each patient underwent upper GI endoscopy to evaluate the prevalence of erosive esophagitis. Erosive esophagitis was diagnosed according to Los Angeles Classification of esophagitis. Results: We enrolled 193 female patients in Group A and 193 patients in Group B. Mean age (± sd) was 48.6 ± 13.6 years in Group A and 51.4 ± 15.3 years in group B. Mean BMI was 43.6 ± 9.2 in group A and 23.6 ± 3.7 in Group B (P<0.001). The perception of GERD symptoms was higher in group B: the mean value of GIS was 1.72 when compared with 0.34 obtained in Group A (P<0.001). The mean value of score for typical GERD symptoms was 2.65 in group B and 0.85 in group A (P<0.001). All patients in Group B recorded at least one typical GERD symptom (heartburn and regurgitate) but only 26.9% of patients in Group A recorded these symptoms (P<0.001). Esophageal erosion were present in 97/193 (50.3%) in Group A and in 45/193 (23.3%) in Group B (P<0.001). Conclusions: We can conclude that the impact of erosive esophagitis in obese patients could be considered more severe than gravity and frequency of symptoms.
Keywords
GI endoscopy; Esophageal adenocarcinoma; Gastroesophageal reflux disease
Introduction
Population-based studies suggest that GERD, defined by at least weekly heartburn and/or regurgitation, is a common condition with an approximate prevalence of 10-20% in Western populations, whereas in Asia the prevalence is reported to be less than 5% [1]. Of note, the prevalence of GERD has been steadily increasing in the United States, Western Europe, and Scandinavian countries and has been associated with a range of risk factors, including obesity [1] Similarly, the prevalence of obesity, typically defined as a body mass index (BMI) = 30 kg/m2, has increased to epidemic proportions during the last two decades [2,3].
A wide variety of evidences (including review articles and meta-analysis) have estimated that obesity is associated with a significant increase in the risk for GERD symptoms, erosive esophagitis, and esophageal adenocarcinoma as compared to individuals with normal BMI [4-6].
Furthermore, a study performed on a large number of monozygotic twins, confirmed that BMI seems to be a risk factor for GERD symptoms [7]. Moreover, in patients with GERD, higher BMI was associated with more severe and more frequent reflux symptoms and esophagitis [8]. A newsworthy large cohort study showed that BMI was associated with GERD symptoms in both normal-weight and overweight/obese women. In particular, the authors demonstrated that even moderate weight gain (an increase in BMI of more than 3.5) among persons of normal weight might cause or exacerbate symptoms of reflux, thus contributing to the evidence for a possible dose-response relationship between increasing BMI and increasing GERD [9]. This is particularly interesting because it might suggest obesity as a pathogenetic event of GERD.
However, it has been hypothesized that obesity may promote the development of GERD symptoms and complications through mechanical and metabolic effects. An increase in BMI has been shown to positively correlate with an increase in esophageal acid exposure (AET) [10-12], and it has been observed that waist circumference might mediate a large part of the effect of obesity on esophageal AET [11], Pandolfino et al., [13] by means of high-resolution manometry, demonstrated that obese subjects are more likely to have esophagogastric junction disruption (leading to hiatal hernia) and an augmented gastroesophageal pressure gradient providing a perfect scenario for reflux to occur.
A mechanically defective lower esophageal sphincter was shown to be more frequent in patients with a higher BMI and obese patients were more than twice as likely to have a defective lower esophageal sphincter compared with normal weight patients [10]. Both intragastric pressure and the gastroesophageal pressure gradient were strongly correlated with both BMI and waist circumference. These findings support the concept that waist circumference is the mediator in the causal relationship between obesity and GERD [13]. Moreover, obesity also may alter the pharmacokinetics of acid suppressive therapies, including distribution (eg, poor blood flow in adipose tissue, obesity-related changes in plasma concentrations of binding proteins, variations in lipophilicity of drugs), metabolism (eg, fatty liver disease, common in obese patients, slowing the enzymatic metabolism of drugs), and elimination (eg, increased glomerular filtration rates and tubular secretion, associated with obesity, accelerating the elimination of some drugs) [14-16].
Another mechanism by which obesity can cause GERD is related to the metabolically active visceral fat that has been associated with low serum levels of protective cytokines, and high levels of inflammatory cytokines [17]. An increase in these inflammatory cytokines in patients with erosive esophagitis and Barrett’s esophagus has also been observed [18].
The aim of the present study was to evaluate the prevalence of symptomatic GERD and esophagitis in female obese subjects.
Material and Methods
Throughout 2012, we prospectively enrolled consecutive female patients presenting to the outpatient units at the Obesity Center and Division of Gastroenterology at the University of Pisa.
From the outpatient Obesity Center, the inclusion criteria were as follows: age higher than 18 years, BMI higher than 30 from a larger group of patients who were scheduled diagnostic work-up for bariatric surgery (Group A).
Sex-matched patients were enrolled from outpatient Gastroenterology Unit. The inclusion criteria were as follows: age higher than 18 years, complaining of heartburn, with or without regurgitation, at least twice a week for six months in the previous year, although not consecutively (Group B).
The exclusion criteria were as follows: pregnancy (excluded by urine analysis) and/or breast-feeding; eating disorders; history of thoracic, esophageal or gastric surgery; underlying psychiatric illness; use of non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin.
During the first visit, a distinct investigator completed a structured interview to all patients, including a careful medical history (with recording of height and weight), current medications, tobacco use and alcohol consumption. GERD symptoms were evaluated by means of a validated questionnaire (GERD impact Scale: GIS) [19-21]. GIS comprises eight questions about the frequency, over the previous 2 weeks, of the following items: acid-related symptoms; chest pain; extra-esophageal symptoms; impact of symptoms on sleep, work, meals and social occasions; use of additional non-prescription medications. Four response options were allowed to describe the frequency of the above items over the previous 2 weeks: 'none of the time' (1), 'a little of the time' (2), 'some of the time' (3) and 'all of the time' (4). All patients signed an informed consent before entering the study. The study was designed and carried out in accordance with the Helsinki Declaration (Sixth revision, Seoul 2008) approved by the institutional review boards.
All patients discontinued PPI therapy at least 20 days before undergoing upper gastrointestinal endoscopy. All endoscopies were performed and recorded by two senior endoscopists, and videos were reviewed to reduce inter-operator variability. Endoscopies were performed with standard devices. The esophageal mucosal erosions, if present, were classified into four grades (from A to D) according to Los Angeles Classification [22].
Endoscopic Suspected Esophageal metaplasia (ESEM) was defined as a detectable upward displacement of the squamocolumnar junction (SCJ) at endoscopy, and it was histologically confirmed by the presence of IM. SCJ was defined as the point where the normal squamous epithelium joined the red mucosa of columnar-lined esophagus. Esophageal-gastric junction (EGJ) was defined as the level at which tubular esophagus joined saccular stomach. In patients with hiatal hernia, this junction was defined by the proximal margin of gastric folds. The length of BE was measured from EGJ to the most proximal extension of columnar epithelium. Systematic 4-quadrant biopsy specimens were collected with standard-size forceps at 2-cm intervals along the whole length of the ESEM segment, starting from the EGJ. Agreement on the presence and extension of BE mucosa and the degree of esophagitis was obtained in all cases. BE was defined as long segment when the length of ESEM was greater than 3 cm, otherwise it was defined as short segment. Biopsies were collected from ESEM to detect the presence of Barrett’s esophagus and from nodules or other mucosa abnormalities.
Biopsies were formalin-fixed and paraffin-embedded. All biopsies were then stained with hemathoxylin-eosin. BE was determined as the presence of specialized intestinal-type metaplasia with goblet cells [23].
Statistical Analysis
Data were expressed as mean and standard deviation (SD). Statistical tests to compare the two groups of subjects included Student’s t test for difference in mean values, Mann-Whitney U and Kruskal-Wallis tests for skewed variables, Pearson’s Chi-squared test (with Yates’s continuity correction as appropriated) for difference in counts and frequency. Pearson test has been performed between BMI and erosive esophagitis in group A patients to look for an association between these two variables. A multivariate analysis was performed to evaluate the “relative risk” and “attributable risk percent” for obesity to determine erosive esophageal erosion. A p-value less than 0.05 was considered statistically significant.
Results
We enrolled 193 female patients in Group A and 193 patients in Group B. Mean age (± sd) was 48.6 ± 13.6 years in Group A and 51.4 ± 15.3 years in group B. Mean BMI was 43.6 ± 9.2 in group A and 23.6 ± 3.7 in Group B (P<0.001). As expected, the body weight was higher in Group A 112.7 ± 31.6 than in Group B 68.8 ± 13.4 (P<0.001). Mean height was 159.3 ± 12.1 (cm) in group A and 171.8 ± 15.6 (cm) in group B (P <0.05).
There were no differences in voluptuary habits as coffee, tobacco and alcohol consumption between two groups (p=n.s.). Detailed results are reported in Table 1.
| Group A (193) | Group B (193) | P value | |
| Mean age (sd) | 48.6 ± 13.6 | 51.4 ± 15.3 | 0.0582 |
| Mean BMI (sd) | 43.6 ± 9.2 | 23.6 ± 3.7 | <0.0001 |
| Smoking (%) | 25 (12.9%) | 31 (16.1%) | 0.368 |
| Alcohol (2-3 unit/die) | 20 (10.4%) | 18 (9.3%) | 0.729 |
| Coffee (2 cup/die) | 49 (25.4%) | 53 (27.5%) | 0.646 |
Table 1: Epidemiological characteristic of population in obese patients (Group A) and patients with GERD symptoms and normal BMI (Group B).
The perception of GERD symptoms was higher in group B: the mean value of GIS was 1.72 in this group when compared with 0.34 obtained in Group A (P<0.001). The mean value of score for typical GERD symptoms was 2.65 in group B and 0.85 in group A (P<0.001).
All patients in Group B recorded at least one typical GERD symptom (heartburn and regurgitate) but only 26.9% of patients in Group A recorded these symptoms (P<0.001). The GERD atypical and extra-esophageal symptoms were also more frequent in Group B (P<0.001). In the section of GIS questionnaire dedicated to explore the impact of GERD symptoms in quality of life showed that patients from Group B had more troublesome symptoms when compared with group A. In particular only 4/193 (2.1%) of patients in Group A recorded symptoms during eating period if compared with Group B in which 44 (22.8%) recorded symptoms in same time period. In Table 2 is summarized the symptom perception in both group (A and B) as recorded with GIS questionnaire.
| Group A mean value (sd) | Group B mean value (sd) | P value | |
| Chest pain | 0.3 (0.2) | 2.6 (0.8) | 0.0001 |
| Heartburn | 0.8 (0.5) | 2.9 (0.5) | 0.0001 |
| Regurgitation | 0.9 (0.4) | 2.4 (0.8) | 0.0001 |
| Upper stomach pain/burning | 0.4 (0.2) | 1.9 (0.4) | 0.0001 |
| Sore throat or hoarseness | 0.1 (0.1) | 0.7 (0.2) | 0.0001 |
| Symptoms during night’s sleep | 0.2 (0.1) | 1.3 (0.3) | 0.0001 |
| Symptoms during eating/drinking | 0.1 (0.1) | 0.7 (0.4) | 0.0001 |
| Symptoms during job/daily activities | 0.2 (0.1) | 1.1 (0.4) | 0.0001 |
| Additional medications | 0.1 (0.1) | 0.9 (0.4) | 0.0001 |
| Mean value (sd) | 0.34 (0.3) | 1.72 (0.4) | 0.0001 |
Table 2: Results of different symptom perception of GERD-related symptoms explored with GIS questionnaire between Group A and Group B.
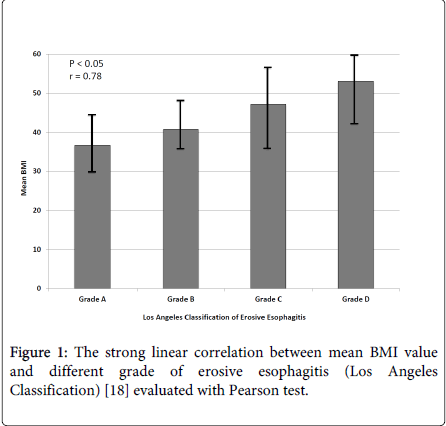
In Group A esophageal erosion were present in 97/193 (50.3%) and were so classified: 43/97 (44.3%) presented grade A (Los Angeles Classification), 27/97 (27.8%) grade B, 19/97 (19.6%) grade C and 8/97 (8.2%) grade D. In Group B esophageal erosion were present in 45/193 (23.3%) and classified: 27/45 (60%) presented grade A, 10/45 (22.2%) grade B, 6/45 (13.3%) grade C and 2/45 (4,4%). All patients from group A had higher prevalence of erosive esophagitis than Group B (P<0.001). In group A mean BMI was higher in patients with more severe esophageal erosion: mean BMI in A grade of esophagitis was 36.4; in grade B was 41.8; in grade C 47.8; in grade D 53.4. The Pearson linear correlation showed a strong correlation between BMI and risk of serious erosive esophagitis (r value of 0.78; P<0.05).
The multivariate analysis detected a Relative Risk (CI 5-95%) of obesity as independent variable in determining erosive esophagitis was 2.16 (1.61–2.89) and subsequently the Attributable Risk Percent was 54.2%.
Discussion
GERD is a chronic disease, which has an impact on the everyday lives of affected individuals, and obesity is found to be a significant risk factor in the development of severe forms of GERD. Changes in gastro-esophageal anatomy and physiology caused by obesity may explain the association [5,6]. Several mechanisms by means of obesity causes reflux disease have been proposed even if the pathogenetic pathway commonly suggested is the increased abdominal pressure that increases esophageal mucosal acid exposure [24].
Results of 24 h pH-monitoring studies have shown that obesity is associated with a significant increase in the number of reflux episodes [11].
Our study showed that patients with obesity had a higher risk for developing esophageal erosion when compared with patients with GERD symptoms but normal weight. The most important information of our study is that patients with obesity (increased BMI) and increased waist circumference showed low GERD-related symptoms perception when compared with esophageal findings. Moreover, the prevalence of esophageal erosion was higher between obese patients when compared with patients who underwent upper endoscopy for GERD symptoms (P<0.001).
An important meta-analysis by Hampel et al. [4] has documented the association between a BMI = 25 kg/m2 and erosive esophagitis. This association was confirmed by Kim et al. [25] who observed, in 27319 subjects, an association between an increasing BMI and abnormal endoscopic findings in particular reflux esophagitis (OR 1.61, 95%CI 1.42-1.83, P<0.001 for overweight subjects; OR 2.23, 95%CI 1.59-3.11, P<0.001 for obese patients). Moreover, Nocon et al. [8] showed that higher BMI in patients with GERD was associated with more severe and frequent reflux symptoms (OR 2.11) and esophagitis (OR 2.51). Similarly, Lee et al. [26] described in patients with GERD, that obese men had the most severe endoscopic and clinical presentation than non-obese.
Recently Savarino and co-worker enrolled 295 patients with GERD-related symptoms, off PPI-therapy, and confirmed that BMI was significantly greater in patients with erosive esophagitis than in those with no mucosal breaks at upper endoscopy [27] In the same study the authors found an higher BMI in patients with abnormal esophageal acid exposure (NERD) when compared with patients with physiologic acid exposure but positive association between symptoms and refluxes (hypersensitive) and patients with functional heartburn [27] Similarly, two different population-based case-control endoscopic studies found a strong and dose-dependent association between BMI and reflux esophagitis, particularly in women rather than men, and hypothesized that this might be caused by increased estrogen activity in overweight and obese females [28,29].
As evidenced the pathogenetic role of obesity in GERD is actually well defined and it has been clearly defined that obese patients with GERD-related symptoms had more esophagitis when compared with non-obese. In our study, we found a strong correlation (r=0.78; P<0.05) between higher BMI and a more severe esophagitis (grade C-D Los Angeles Classification) as showed in Figure 1.
The evidenced epidemiological study that underlined the strong correlation between GERD and BMI has been performed in patients with typical GERD-related symptoms in which the higher body weight has been found as strong risk factor for developing symptoms and erosive esophageal lesions. Differently, we evaluated the risk of erosive esophagitis in strong obese patients (BMI>40) regardless of the presence of GERD-related symptoms as selection criteria. The calculated RR shows that obese patients (BMI>30) has 2.16 higher risk to develop esophageal erosion when compared with a control group. In this regard, Pandolfino et al. [13] reviewed high-resolution manometry recordings in 285 patients, focusing on pressure changes across the esophagogastric junction during respiratory cycles, measuring intragastric and intraesophageal pressures and calculating the gastroesophageal pressure gradient. In this study the authors evidenced that obesity was associated with separation of the esophagogastric junction pressure components (BMI, r=0.17, P<0.005; WC, r=0.21, P<0.001) and it could be suggestive of temporal developing hiatal hernia and they concluded that obese subjects are more likely to have esophagogastric junction disruption (leading to hiatal hernia), and augmenting the gastroesophageal pressure gradient provided a perfect scenario for reflux to occur.
The most important epidemiologic study in GERD patients found that impact of heartburn is more frequent than presence of esophageal erosion [1,30,31]. Prevalence of esophageal erosion ranging between 35-38% [1,30,31].
On the other hand, this is the first study that strongly evidences that obese patients have low impact in symptom perception but more frequent esophageal erosion. The GIS questionnaire underline that the frequency of GERD-related symptoms and their impact in quality of life in obese patients is less frequent than in patients with normal weight (P<0.0001). In obese group (group A) patients reported heartburn at least once in a week in 26.9% versus 100% of control group (group B) who referred to perform endoscopy for GERD-related symptoms.
In the Nurses’ Health Study focusing on risks for cancer and cardiovascular diseases 12,192 participants where evaluated for GERD-related symptoms. A total of 10,545 (86%) returned the questionnaires, with 2306 (22%) participants reporting GERD symptoms at least once a week, 256 (11%) of whom with severe to very severe (ie, affecting/greatly affecting lifestyle) symptoms [9]. In 2005 El-Serag found similar results describing that 26% (118/453) obese patients reported weakly heartburn [32]. The authors summarized these findings as indicative that higher BMI increases the risk of GERD symptoms independent of demographic features and dietary intake.
As above described, our obese patients (group A) showed a high prevalence of erosive esophagitis and low prevalence of heartburn or other GERD-related symptoms. We can speculate that the chronic high esophageal acid exposure time [27] in obese patients might result in a reduced esophageal mucosal perception for acid as frequently described in patients with Barrett esophagus [33]. A similar result was observed in a population-based study in Korea, in which only 58% of patients with erosive esophagitis showed GERD-related symptoms [34]. It is possible that the frequent food intake in obese patients might reduce their symptom perceptions; indeed they reported less symptom perception during eating/drinking (as showed in GIS questionnaire) than non-obese patients.
This study interestingly shows the strong correlation between BMI and erosive esophagitis, but it has a limitation is due to the lack of pathophysiological evaluations (esophageal manometry and pH-metry/impedance-pH 24-h) that could better explained the differences between patients with erosive esophagitis and those without. On the other hand, the primary aim was to correlate symptoms with the risk of esophageal erosion in obese patients, who demand great care from their physicians in erosive esophagitis diagnosis, independently from the prevalence of their symptoms perception.
In conclusion, obese patients evaluated for bariatric surgery showed a higher prevalence of esophageal erosion and lower symptom perception when compared with a control group of patients with heartburn. Obesity could be considered a serious risk factor for erosive esophagitis and these patients should be endoscopically evaluated independently of the presence of GERD symptoms. Diet, cognitive behavior therapy or bariatric surgery should be strongly recommended to reduce evolution of the acid-related esophageal disease.
References
- Dent J, El-Serag HB, Wallander MA, Johansson S (2005) Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 54: 710-717.
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, et al. (2004) Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA 291: 2847-2850.
- Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, et al. (2006) Prevalence of overweight and obesity in the United States, 1999-2004. JAMA 295: 1549-1555.
- Hampel H, Abraham NS, El-Serag HB (2005) Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med 143: 199-211.
- El-Serag H (2008) The association between obesity and GERD: a review of the epidemiological evidence. Dig Dis Sci 53: 2307-2312.
- Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J (2003) Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA 290: 66-72.
- Zheng Z, Nordenstedt H, Pedersen NL, Lagergren J, Ye W (2007) Lifestyle factors and risk for symptomatic gastroesophageal reflux in monozygotic twins. Gastroenterology. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't Twin Study]132: 87-95.
- Nocon M, Labenz J, Jaspersen D, Meyer-Sabellek W, Stolte M, et al. (2007) Association of body mass index with heartburn, regurgitation and esophagitis: results of the Progression of Gastroesophageal Reflux Disease study. J Gastroenterol Hepatol 22: 1728-1731.
- Jacobson BC, Somers SC, Fuchs CS, Kelly CP, Camargo CA Jr (2006) Body-mass index and symptoms of gastroesophageal reflux in women. N Engl J Med 354: 2340-2348.
- Ayazi S, Hagen JA, Chan LS, DeMeester SR, Lin MW, et al. (2009) Obesity and gastroesophageal reflux: quantifying the association between body mass index, esophageal acid exposure, and lower esophageal sphincter status in a large series of patients with reflux symptoms. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 13:1440-1447.
- El-Serag HB, Ergun GA, Pandolfino J, Fitzgerald S, Tran T, et al. (2007) Obesity increases oesophageal acid exposure. Gut 56: 749-755.
- Crowell MD, Bradley A, Hansel S, Dionisio P, Kim HJ, et al. (2009) Obesity is associated with increased 48-h esophageal acid exposure in patients with symptomatic gastroesophageal reflux. Am J Gastroenterol 104: 553-559.
- Pandolfino JE, El-Serag HB, Zhang Q, Shah N, Ghosh SK, et al. (2006) Obesity: a challenge to esophagogastric junction integrity. Gastroenterology 130: 639-649.
- Blouin RA, Warren GW(1999) Pharmacokinetic considerations in obesity. J Pharm Sci. [Research Support, U.S. Gov't, P.H.S.Review] 88: 1-7.
- Jacobson BC (2008) Body mass index and the efficacy of acid-mediating agents for GERD. Dig Dis Sci 53: 2313-2317.
- Barak N, Ehrenpreis ED, Harrison JR, Sitrin MD (2002) Gastro-oesophageal reflux disease in obesity: pathophysiological and therapeutic considerations. Obes Rev 3: 9-15.
- Cnop M, Landchild MJ, Vidal J, Havel PJ, Knowles NG, et al. (2002) The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations : distinct metabolic effects of two fat compartments. Diabetes. [Comparative Study Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S. Research Support, U.S. Gov't, P.H.S.] 51:1005-1015.
- Tselepis C, Perry I, Dawson C, Hardy R, Darnton SJ, et al. (2002) Tumour necrosis factor-alpha in Barrett's oesophagus: a potential novel mechanism of action. Oncogene 21: 6071-6081.
- Ferrús JA, Zapardiel J, Sobreviela E; SYMPATHY I study group (2009) Management of gastroesophageal reflux disease in primary care settings in Spain: SYMPATHY I study. Eur J Gastroenterol Hepatol 21: 1269-1278.
- Martinucci I, de Bortoli N, Savarino E, Piaggi P, Bellini M, et al. (2014) Esophageal baseline impedance levels in patients with pathophysiological characteristics of functional heartburn. Neurogastroenterology and motility : the official journal of the European Gastrointestinal Motility Society 26: 546-55.
- de Bortoli N, Martinucci I, Savarino E, Bellini M, Bredenoord AJ, et al. (2014) Proton pump inhibitor responders who are not confirmed as GERD patients with impedance and pH monitoring: who are they? Neurogastroenterol Motil 26: 28-35.
- Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, et al. (1999) Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 45: 172-180.
- Sampliner RE (1998) Practice guidelines on the diagnosis, surveillance, and therapy of Barrett's esophagus. The Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol 93: 1028-1032.
- El-Serag HB, Tran T, Richardson P, Ergun G (2006) Anthropometric correlates of intragastric pressure. Scand J Gastroenterol 41: 887-891.
- Kim HJ, Yoo TW, Park DI, Park JH, Cho YK, et al. (2007) Influence of overweight and obesity on upper endoscopic findings. J Gastroenterol Hepatol 22: 477-481.
- Lee SW, Lien HC, Chang CS, Peng YC, Ko CW, et al. (2012) Impact of body mass index and gender on quality of life in patients with gastroesophageal reflux disease. World J Gastroenterol 18: 5090-5095.
- Savarino E, Zentilin P, Marabotto E, Bonfanti D, Inferrera S, et al. (2011) Overweight is a risk factor for both erosive and non-erosive reflux disease. Digestive and liver disease : official journal of the Italian Society of Gastroenterology and the Italian Association for the Study of the Liver 43: 940-945.
- Stene-Larsen G, Weberg R, Frøyshov Larsen I, Bjørtuft O, Hoel B, et al. (1988) Relationship of overweight to hiatus hernia and reflux oesophagitis. Scand J Gastroenterol 23: 427-432.
- Nilsson M, Lundegardh G, Carling L, Ye W, Lagergren J(2002) Body mass and reflux oesophagitis: an oestrogen-dependent association? Scandinavian Journal of Gastroenterology. [Comparative Study Research Support, Non-U.S. Gov't] 37:626-630.
- Malfertheiner P, Nocon M, Vieth M, Stolte M, Jaspersen D, et al.(2012) Evolution of gastro-oesophageal reflux disease over 5 years under routine medical care--the ProGERD study. Alimentary pharmacology & therapeutics. [Multicenter Study Research Support, Non-U.S. Gov't] 35: 154-164.
- Hartmann D, Kudis V, Jakobs R, Riemann JF, Schilling D(2006) Course of erosive gastroesophageal reflux disease (ERD)--a prospective examination under therapeutic daily life conditions with a mean follow-up of 6.5 years. Zeitschrift fur Gastroenterologie. [Clinical Trial] 44: 1039-1042.
- El-Serag HB, Graham DY, Satia JA, Rabeneck L (2005) Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol 100: 1243-1250.
- Coleman HG, Bhat SK, Murray LJ, McManus DT, O'Neill OM, et al. (2014) Symptoms and endoscopic features at barrett's esophagus diagnosis: implications for neoplastic progression risk. The American journal of gastroenterology. [Evaluation Studies Research Support, Non-U.S. Gov't] 109: 527-534.
- Kim N, Lee SW, Cho SI, Park CG, Yang CH, et al. (2008) The prevalence of and risk factors for erosive oesophagitis and non-erosive reflux disease: a nationwide multicentre prospective study in Korea. Alimentary pharmacology & therapeutics. [Multicenter Study] 27: 173-185.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15584
- [From(publication date):
June-2014 - Jul 02, 2025] - Breakdown by view type
- HTML page views : 10907
- PDF downloads : 4677