Research Article Open Access
Nursing Staff’s Knowledge about and Skills in Providing Oral Hygiene Care for Patients with Neurological Disorders
Vanessa Hollaar1-3*, Claar van der Maarel-Wierink2,3, Gert-Jan van der Putten2,3, Berna Rood4, Hans Elvers5, Cees de Baat2,3 and Bert de Swart1,61Department of Neurorehabilitation, HAN University of Applied Sciences, The Netherlands
2BENECOMO, Flemish-Netherlands Geriatric Oral Research Group, The Netherlands
3Department of Oral Function and Prosthetic Dentistry, Radboud university medical center, The Netherlands
4Nijmegen Knowledge Centre of Neurorehabilitation, Radboud university medical center, The Netherlands
5Education of Dental Hygiene Department of Primary and Community Care, Radboud university medical center, The Netherlands
6Department of Rehabilitation, Radboud university medical center, The Netherlands
- *Corresponding Author:
- Vanessa Hollaar
HAN University of Applied Sciences
P.O. Box 6960, 6503 GL
Nijmegen, The Netherlands
Tel: +31 (0)24 361 63 65
E-mail: vanessa.hollaar@ radboudumc.nl
Received Date: October 08, 2015; Accepted Date: November 18, 2015; Published Date: November 26, 2015
Citation: Hollaar V, Maarel-Wierink Cvd, Putten Gvd, Rood B, Elvers H, et al. (2015) Nursing Staff’s Knowledge about and Skills in Providing Oral Hygiene Care for Patients with Neurological Disorders. J Oral Hyg Health 3:190. doi:10.4172/2332-0702.1000190
Copyright: © 2015 Hollaar V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Objectives: To determine nursing staff’s current knowledge on providing oral hygiene care to patients with neurological disorders, to develop a structured basic oral examination guideline and flowchart, to educate and train the nursing staff practically concerning performing a structured basic oral examination, and to compare their perceptions on their knowledge and skills before and after education and practical training. Methods: The study was performed at a hospital’s department for patients with neurological disorders in the Netherlands. The study was conducted in two Projects: (1) using a questionnaire, several aspects of providing oral hygiene care by the nursing staff were examined; (2) a guideline for a structured basic oral examination was developed, the nursing staff received training to use the guideline, the potential increase of the nursing staff’s knowledge and skills was evaluated using a scoring form before and after the education and practical training and their perception on performing this examination was assessed using 11 questions. Results: (1) The nursing staff experienced some problems during providing oral hygiene care and demonstrated a lack of knowledge on cleansing and handling removable dentures, whereas they considered themselves adequately skilled. (2) Education and practical training did not improve their knowledge and skills, but enhanced their perception of competence significantly. Conclusions: The nursing staff demonstrated a lack of knowledge. Education and practical training enhanced their perception of their knowledge and skills concerning performing a structured basic oral examination.
Keywords
Oral hygiene care; Oral examination; Nursing staff; Education; Knowledge; Skills; Guideline
Introduction
Several hospitalized patients with neurological disorders depend on nursing staff for their daily health care. Due to several functional limitations of the limbs, oral motor impairments, neglect, apraxia, and hemianopia, oral hygiene self-care is difficult to perform and therefore adequate oral health is difficult to maintain [1]. Next to that, oral dysfunction related to oral motor function, mastication, swallowing and saliva control may be affected and does not always recover completely during rehabilitation [2]. Due to both physical and oral dysfunction, adequate oral health may be threatened, because the affected functions hinder this population when performing daily oral hygiene self-care. Consequently, the responsibility for completing oral care in neurological patients often falls to the nursing staff. Oral health has not been given priority in nursing practice, because there are competing priorities regarding the care nurses provide, but it should become a task with higher priority [3,4].
The nursing staff plays an important role in the rehabilitation of patients with neurological disorders through re-teaching them the necessary skills to perform independent oral hygiene. By re-teaching these independent oral hygiene skills, there is potential to improve patients’ hand and oral motor functions, thus enabling improved coping and reduced resistant behavior associated with neurological complications. This will enable the patients to cope with the complications of their diseases [5]. Oral hygiene care can be further complicated by resistant behavior resulting in ineffective and labour intensive oral care [6-12]. This requires well-educated, trained and competent nursing staff that can provide oral hygiene care, taking into account the patients’ functional and behavioral limitations.
Inadequate or absent oral hygiene care reduces oral health, may have a negative impact on general health and may cause serious complications [13]. Regular daily oral hygiene care reduces the concentration of oropharyngeal bacteria and the consequences of aspiration of oropharyngeal secretions. Given the fact that aspiration of oropharyngeal secretions is recognized as an important factor in the development of pneumonia, it is necessary to prevent this complication [14-19]. Dysphagia increases the risk of developing pneumonia [20,21]. Recent studies found a prevalence of dysphagia between 51 and 73% in stroke patients [22,23], illustrating the importance of developing and implementing routine oral hygiene care guidelines in order to prevent these high-risk patients from developing pneumonia [24,25].
Systematic approaches, such as evidence-based oral hygiene care guidelines, improve the quality of oral hygiene care, reduce complications such as ventilator induced aspiration pneumonia [26] and increase nursing staff’s awareness and knowledge [9]. Oral assessment is recommended for planning and providing appropriate oral hygiene care [27-29]. A randomised controlled clinical trial, using guidelines for oral hygiene care to care-dependent older people, showed a significant reduction of dental and denture biofilm in the experimental group [30]. Previous studies have recommended research on which nursing interventions are effective for oral hygiene care for stroke patients [17,31]. However, more research is needed to provide evidence-based oral hygiene care to patients with neurological disorders.
In general,oral healthand oral hygiene are overlooked in nursing education [32], as there is no particular module which pays special attention to the consequences of insufficient oral health for general health [33-36]. Therefore, providing the nursing staff with education about oral health and oral hygiene care is necessary. Park & Choi- Kwon (2011) showed that an oral hygiene care education programme for the nursing staff in nursing homes was effective in improving the oral hygiene care to the residents. This effect was achieved by the enhancement of the nursing staff’s knowledge, attitude and behavior. Systematic literature reviews showed that nursing staff’s knowledge and attitude towards oral hygiene care improved significantly after oral hygiene care education [17,37].
In order to determine which is the best practice approach to providing oral hygiene care to patients with neurological disorders, one needs information about the nursing staff’s current oral hygiene care knowledge and skills. Following this, a clinical guideline, flowchart and education should be provided in order to improve the knowledge and skills required to provide adequate oral hygiene. This article describes two distinct research projects which were performed at a hospital’s department for patients with neurological disorders in The Netherlands during the period 2008-2011. The objective of Project 1 was to investigate the current nursing staff’s knowledge of oral hygiene care. The first objective of Project 2 was to examine the use of a clinical guideline and flowchart for performing a structured basic oral examination before and after education and training. The second objective of Project 2 was to compare the nursing staff’s perception of their knowledge and skills with regard to performing a structured basic oral examination before and after education and practical training.
Methods
Setting and sample
Both Projects of the study were carried out in the Department of Neurology of a hospital in The Netherlands. Participants of both Projects were the nursing staff of the Department of Neurology, which included 38 members. Because both Projects were aimed at the nursing staff, patients were not recruited.
Data collection tools
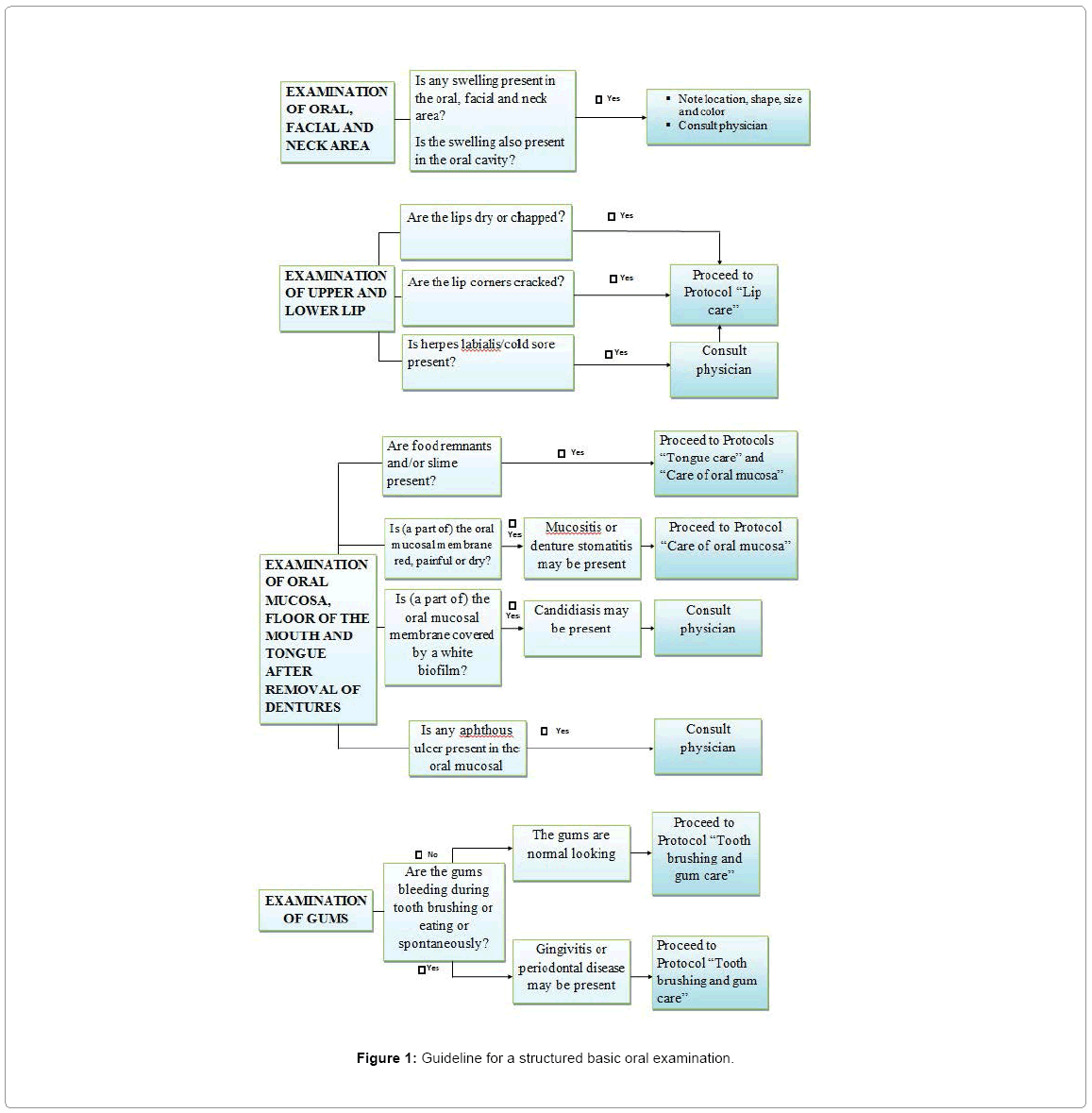
Project 1 involved a questionnaire to be completed by all members of the nursing staff of the Department of Neurology. The questionnaire was originally in Dutch and was (later) translated into English for the purpose of this article. For Project 2 a newly developed structured basic oral examination was used (Figure 1) and the participating members of the nursing staff also completed an 11-item questionnaire using Visual Analogue Scale (VAS) before and after their education and training.
Ethical considerations
The head of the nursing staff of the Department of Neurology approved the study and collaboration was granted. During Project 2, patients received their usual nursing care and were not involved in testing any new care interventions. Collected data of patients during basic oral examination were only used to check whether the same data were found by the nursing staff and the investigators.
Data collection
For Project 1, a questionnaire was developed by the research team in order to evaluate general information, experiences and knowledge of the provided oral hygiene care. Questionnaires were distributed to all members of the nursing staff. The data collection took place in January 2008. All members had four weeks to complete the questionnaire. The questionnaire contained three general questions and nine questions about several aspects of providing oral hygiene care to patients with neurological disorders (Table 1):
• Three general questions about gender, age and number of years of working experience respectively;
• Four questions about experiences during providing oral hygiene care, three with two response options and one open question;
• Four statements about one’s knowledge of providing oral hygiene care with two response options;
• One question about the currently recommended oral examination guideline, with two response options.
| Topics and questions | Response options | Responses | Responses to open questions | Numbers (%) |
|---|---|---|---|---|
| General | ||||
| Gender | Female /Male | Women 16 (89%) | ||
| Age | Mean: 37.4 ± 9.7 | |||
| Years of working experience | Mean: 14.2 ± 10.1 | |||
| Experiences with providing oral hygiene care | ||||
| Do you experience specific problems when providing oral hygiene care? | Restricted mouth opening | 11 (61%) | ||
| Tongue cleaning is unpleasant for patients and nurses | 11 (61%) | |||
| Some patients refuse | 4 (22%) | |||
| Fear that the patient will choke | 4 (22%) | |||
| Tongue coating | 3 (17%) | |||
| Patients with decreased | 2 (11) | |||
| consciousness | ||||
| Do you have sufficient knowledge about providing oral hygiene care? | Yes/No | Yes: 15 (83%) | ||
| Do you have sufficient skills to provide oral hygiene care? | Yes/No | Yes: 12 (67%) | ||
| Do you perceive yourself competent to perform an oral examination? | Yes/No | Yes: 11 (61%) | ||
| Knowledge about providing oral hygiene care | ||||
| Removable dentures should be cleansed with toothpaste. | Correct/Not correct | Not correct: 16 (89%) | ||
| Removable dentures should not be worn overnight. | Correct/Not correct | Not correct: 14 (78%) | ||
| Removable dentures should be stored dry overnight. | Correct/Not correct | Not correct: 14 (78%) | ||
| Poor oral hygiene care can cause aspiration pneumonia. | Correct/Not correct | Correct: 18 (100%) | ||
| Guideline | ||||
| Is the currently recommended guideline forperforming an oral examination familiar to you? | Yes/No | No: 15 (83%) |
Table 1: Topics of the questionnaire on oral hygiene care and answers given by the nursing staff.
At the start of Project 2 a guideline for a structured basic oral examination of patients with neurological disorders was developed by a dental hygienist and two nurses of the Department of Neurology. This teamwork guaranteed the multidisciplinary character of the guideline by combining the knowledge and the practical experience of the three health care providers. The guideline includes information on the relevant extra and intra oral anatomical structures, information on the (sequence of the) examination to be performed and instructions on how to use the result of the examination for deciding on the appropriate individual oral hygiene care. When additional individual oral hygiene care is needed, protocols are available for lip, tongue and oral mucosa care and for tooth brushing and gum care. The development of the guideline and protocols took place from September 2008 till July 2009. The protocols are not presented in this article.
Four investigators were trained to use the guideline and they tested it by independently performing structured basic oral examinations of four patients with neurological disorders, using a scoring form containing nine items which need to be assessed when performing an oral examination (Table 2). After each sequence of oral examinations of one patient by the four investigators, they compared their scores of the nine items of the scoring form. The differences were discussed and minor adjustments of the guideline were made in order to improve the guideline. Subsequently, the four investigators were educated to observe the members of the nursing staff when they performed a structured basic oral examination, using the scoring form. They were calibrated by subsequently observing five members of the nursing staff independently. After each sequence of oral examinations of one patient by the four investigators, the results were compared. The differences were discussed and minor adjustments of the observation instructions and the guideline as well as the scoring form were made in order to improve the inter investigator reliability and face validity.
| Item | Before | After |
|---|---|---|
| Is any swelling present in the oral, facial and neck area? | 19 (95%) | 19 (95%) |
| Are the lips dry or chapped? | 16 (80%) | 15 (75%) |
| Are the lip corners cracked? | 20 (100%) | 20 (100%) |
| Is herpes labialis/cold sore present? | 20 (100%) | 19 (95%) |
| Are food remnants and/or slime present? | 17 (85%) | 18 (90%) |
| Is (a part of) the oral mucosal membrane red, painful or dry? | 18 (90%) | 17 (85%) |
| Is (a part of) the oral mucosal membrane covered by a white biofilm? | 17 (85%) | 20 (100%) |
| Is any aphthous ulcer present in the oral mucosal membrane? | 15 (75%) | 20 (100%) |
| Are the gums bleeding during tooth brushing or eating or spontaneously? | 19 (95%) | 19 (95%) |
Table 2: Conformity level of the nine items of the structured basic oral examination by the 20 members of the nursing staff and the four investigators before and after education and practical training.
The education and practical training and data collection took place from January 2010 till April 2010. For the main part of Project 2, every member of the nursing staff did two individual standardized practical training sessions with the four calibrated investigators on performing a structured basic oral examination in accordance with the newly developed guideline. To examine whether the knowledge and skills with regard to the performance of a structured basic oral examination would improve after the education and practical training, the nursing staff as well as the investigators performed structured basic oral examinations using the scoring form before and 12 weeks after the education and practical training. The results of the examinations by a member of the nursing staff and by an investigator were compared. A conformity level of 80% for each item on the scoring form was considered acceptable. On top of that, the nursing staff’s perception of their knowledge and skills concerning the performance of a structured basic oral examination was assessed before and after the education and practical training, using 11 questions whose answer scores were shown on a visual analogue scale (VAS) [38]. Nine questions were about the nursing staff’s perception of having sufficient knowledge about several extra and intra oral anomalies and pathologic conditions and two questions were about their perception of being competent in judging a removable denture’s condition and an oral hygiene condition (Table 3).
| Item | Mean before-Mean after | Mean increase |
|---|---|---|
| Do you have sufficient knowledge aboutfacial anomalies? | 42 – 63 | 21 ± 4.1 |
| Do you have sufficient knowledge about oral labial pathology? | 44 – 69 | 25 ± 4.2 |
| Do you have sufficient knowledge about buccal mucosal pathology? | 38 – 67 | 29 ± 4.1 |
| Do you have sufficient knowledge about n palatal pathology? | 33 – 62 | 29 ± 4.3 |
| Do you have sufficient knowledge aboutthe potential conditions of dentate gums? | 45 – 68 | 23 ± 4.1 |
| Do you have sufficient knowledge about salivary anomalies? | 33 – 63 | 30 ± 5.3 |
| Do you have sufficient knowledge about tongue pathology? | 35 – 68 | 33 ± 4.3 |
| Do you have sufficient knowledge about pathologic condition of teeth? | 41 – 62 | 21 ± 3.6 |
| Do you have sufficient knowledge about pathology of edentulous gums? | 25 – 60 | 35 ± 5.1 |
| Do you perceive yourself competent to judge a removable denture’s condition? | 27 – 58 | 31 ± 4.8 |
Table 3: Means in mm on the VAS of items of the nursing staff’s perception of their knowledge and skills concerning the performance of a structured basic oral examination before and after education and practical training and the mean increases with standard deviations (±).
Data analysis
The quantitative research data of Project 1 from the completed questionnaires were analyzed using SPSS 18.0.
For Project 2, data were also analyzed using SPSS 18.0. A Sign test was used to compare the results of the structured basic oral examinations by the investigators and the nursing staff (α = 0.05). The VAS scores at baseline and at 12 weeks were analyzed by the Paired-t test (α = 0.05).
Results
Project 1: Questionnaire about knowledge of oral hygiene care
Thirty-eight questionnaires were distributed and 18 members of the nursing staff (47%) completed the questionnaire. The results are presented in Table 1. The nursing staff experienced some specific practical problems when providing oral hygiene care due to their patients’ neurological disorders, such as restricted mouth opening (61%), refusing oral hygiene care (22%) and decreased consciousness (11%). Tongue cleansing was experienced as unpleasant by both the nursing staff and their patients (61%). A remarkable finding was that all respondents indicated correctly that poor oral hygiene might cause aspiration pneumonia. More than 75% of the respondents did not know the relevant aspects of handling and cleansing removable dentures. However, 83% of the respondents considered themselves sufficiently skilled to provide oral hygiene care and 67% considered their knowledge of providing oral hygiene care as sufficient. Furthermore, eleven respondents (61%) perceived themselves competent to perform an oral examination. More than 80% answered that the currently recommended guideline for performing an oral examination was not familiar to them.
Project 2: Structured basic oral examination
At the start of Project 2, 26 members of the nursing staff of the Department of Neurology were available for the education and practical training. During Project 2, six members were excluded because they were transferred to another department, quit their job or did not finish the practical training, leaving data available of 20 members of the nursing staff. Eighteen of these 20 participating members of the nursing staff also participated in Project 1.
Before the education and practical training, the scores of all members of the nursing staff and investigators were identical on two items on the scoring form and at least 16, but not all members of the nursing staff scored the same as the investigators on six items on the scoring form. This means that the required conformity level of 80% was achieved in eight of the nine items (Table 2).
After the education and practical training, the scores of all members of the nursing staff and investigators were identical on three items on the scoring form. At least 16, but not all members of the nursing staff scored the same as the investigators on five items on the scoring form. This means that the required conformity level of 80% was achieved in eight of the nine items. Before the education and practical training there was agreement between 15 members of the nursing staff and investigators on the item ‘Is any aphthous ulcer present in the oral mucosal membrane?’ After the education and practical training there was agreement between all 20 of them: a significant improvement (Table 2).
Before the education and practical training, the nursing staff expressed their incompetence regarding knowledge and skills concerning the performance of a structured basic oral examination. The lowest mean VAS score (25) was found on the item ‘Do you have sufficient knowledge about pathology of edentulous gums?’, whereas the highest mean VAS score (48) was found on the item ‘Do you perceive yourself competent to judge an oral hygiene condition?’ (Table 3). After the education and practical training, the nursing staff expressed, for almost all items, that they had sufficient knowledge and perceived themselves competent to perform a structured basic oral examination. On all items statistically significant improvements were found after the education and practical training, when compared to the situation before these took place ( α = 0.05; P < 0.05) (Table 3).
Discussion
The objective of Project 1 was to determine the nursing staff’s current knowledge about providing oral hygiene care. A significant lack of knowledge of the relevant aspects of handling and cleansing removable dentures was found. Furthermore, they experienced several problems when providing oral hygiene care, predominantly a restricted mouth opening and the unpleasantness of tongue cleansing, experienced by both patients and themselves. Moreover, the currently recommended guideline for performing an oral examination was not familiar to most of them. The nursing staff reported problems with patients who refused oral health care. Refusing patients cause perceptions of insecurity among the nursing staff during the providing of oral hygiene care, inducing them to consider performing oral hygiene care as an unpleasant care task [3,6-12,39,40].
Despite the lack of knowledge, a majority of the nursing staff expressed that they had sufficient knowledge and skills concerning providing oral hygiene care and that they perceived themselves competent to perform an oral examination. These results revealed an objective lack of knowledge among the members of the nursing staff, which was not experienced subjectively by the majority of them, suggesting that education in providing oral hygiene care is required. The requirement of education together with the fact, that the currently recommended guidelines for performing an oral examination was not familiar to most of the members of the nursing staff, were the incentives to start the education at the very beginning. Surely, to determine which oral hygiene care is needed, first a structured basic oral examination must be performed. Therefore, a new flowchart and a guideline for a structured basic oral examination were developed, which enabled the nursing staff to determine and provide individual oral hygiene care.
The first objective for Project 2 was to examine the use of a clinical guideline and flowchart for performing a basic oral examination before and after education and training. Actually, the education and practical training did not improve their practical performances. Probably, they were already able to perform a structured basic oral examination adequately before the education and practical training took place. A potential explanation for this result is that the newly developed structured basic oral examination is easy to use, enabling the nursing staff to follow the guideline without education and practical training. More research is needed to confirm this potential explanation.
The second objective of Project 2 was to compare the nursing staff’s perception of their knowledge and skills with regard to performing a structured basic oral examination before and after the education and practical training. The results showed that the education and practical training had enhanced the nursing staff’s perception of their knowledge and skills in a statistically significant way. However, before the education and practical training, they had already proven in practice, that they were able to do this adequately. A recent study demonstrated that perceptions of insecurity about being well-trained practically can create barriers when providing oral hygiene care [12]. Probably, in the current study, education and practical training were needed to enhance the nursing staff’s perception of competence.
It is of great concern to repeat the oral hygiene care education and practical training. Through repeated education and practical training, the nursing staff will be encouraged to improve their knowledge and skills concerning individual oral hygiene care [23,41,42]. Repeated education and practical training ensure that the nursing staffs have up-to-date evidence-based knowledge about individual oral hygiene care. However, a recent systematic review showed that oral health care education may have a positive effect on nurses’ oral health care knowledge and attitude, but any effect on nurses’ oral hygiene care skills could not yet be found in the literature [37].
There were certain limitations to both Projects in this study. Project 1 had the limitation that only a small number of questionnaires were completed and returned by the members of the nursing staff. Another limitation was that the results may have been influenced by socially desirable responses by the nursing staff. Furthermore, this study took place in one hospital and, therefore, the findings cannot be generalized. Similar research at Departments of Neurology in other hospitals is needed to confirm the findings. Limitations of Project 2 were that the group of participating members of the nursing staff was relatively small and that not every member of the nursing staff had taken part in the education and practical training. Next to that, there was no control group available. Besides the education, unknown variables may have influenced the participating members of the nursing staff and may have caused some bias. A future study or project could assess knowledge and skills together with the practical performance of the individual oral hygiene care by the nursing staff.
Conclusions
Project 1 of this study has demonstrated a significant lack of knowledge about oral hygiene care among the nursing staff, whereas, contradictorily, this lack of knowledge was not experienced subjectively by the majority of them. Moreover, the nursing staff experienced several specific practical problems when providing oral hygiene care. Project 2 has demonstrated that before the education and practical training took place, the nursing staff had expressed that they did not have sufficient knowledge and perceived themselves not competent to perform a structured basic oral examination of patients with neurological disorders. Nevertheless, they showed that they were able to perform a structured basic oral examination adequately and the education and practical training did not improve their examination performances. The education and practical training did enhance their perception of their knowledge and skills concerning the performance of a structured basic oral examination in a statistically significant manner. Education and practical training for nursing staff in order to provide individual oral hygiene care adequately is needed to diminish any barriers which are experienced when providing individual oral hygiene care. Repeated education ensures that the nursing staffs have up-to-date evidence based knowledge.
Implications for Nursing Practice
After education and practical training for the nursing staff, the clinical guideline and flowchart for performing a basic oral examination of patients with neurological disorders are useful instruments.
Author Contributions
VH was responsible for the study conception and design. VH performed the data collection. VH, BS and BR performed the data analysis. BR was responsible for the contacts with the nursing staff on the hospital ward. BS and BR supervised the study. BS, CvdM, GJvdP, BR, HE and CB made critical remarks on this article, adding important intellectual content.
Acknowledgements
The authors would like to thank the nursing staff and all members of the participating Department of Neurology for their cooperation. Special thanks go to Grada Nederl of (senior nurse) for her commitment and support. Next to that, the contributions by research associates Eefje Clermonts, Claire Nijenhuis, Stephanie Oudeman and Lenny Schot are acknowledged.
Conflict of interest
No conflict of interest has been declared by the authors.
References
- Scannapieco FA, Papandonatos GD, Dunford RG (1998) Association between oral conditions and respiratory disease in a national sample survey population. Ann Periodontol 3: 251-256.
- Smithard DG1 (2002) Swallowing and stroke. Neurological effects and recovery.Cerebrovasc Dis 14: 1-8.
- Allen Furr L, Binkley CJ, McCurren C, Carrico R (2004) Factors affecting quality of oral care in intensive care units.J Adv Nurs 48: 454-462.
- Dolce MC1 (2012) Nurse faculty enrichment and competency development in oral-systemic health.Nurs Res Pract 2012: 567058.
- Brady MC, Stott DJ, Norrie J, Chalmers C, St George B, et al. (2011) Developing and evaluating the implementation of a complex intervention: using mixed methods to inform the design of a randomised controlled trial of an oral healthcare intervention after stroke. Trials 12: 168.
- Costello T, Coyne I (2008) Nurses' knowledge of mouth care practices.Br J Nurs 17: 264-268.
- Kullberg E, Sjögren P, Forsell M, Hoogstraate J, Herbst B, et al. (2010) Dental hygiene education for nursing staff in a nursing home for older people.J Adv Nurs 66: 1273-1279.
- Forsell M, Sjögren P, Kullberg E, Johansson O, Wedel P, et al. (2011) Attitudes and perceptions towards oral hygiene tasks among geriatric nursing home staff.Int J Dent Hyg 9: 199-203.
- Chan EY, Hui-Ling Ng I (2012) Oral care practices among critical care nurses in Singapore: a questionnaire survey.Appl Nurs Res 25: 197-204.
- Hanne K, Ingelise T, Linda C, Ulrich PP (2012) Oral status and the need for oral health care among patients hospitalised with acute medical conditions.J Clin Nurs 21: 2851-2859.
- Wårdh I, Jonsson M, Wikström M (2012) Attitudes to and knowledge about oral health care among nursing home personnel--an area in need of improvement.Gerodontology 29: e787-792.
- Willumsen T, Karlsen L, Naess R, Bjørntvedt S (2012) Are the barriers to good oral hygiene in nursing homes within the nurses or the patients?Gerodontology 29: e748-755.
- Rautemaa R, Lauhio A, Cullinan MP, Seymour GJ (2007) Oral infections and systemic disease--an emerging problem in medicine.Clin Microbiol Infect 13: 1041-1047.
- Scannapieco FA1 (1999) Role of oral bacteria in respiratory infection.J Periodontol 70: 793-802.
- Yoneyama T, Yoshida M, Ohrui T, Mukaiyama H, Okamoto H, et al. (2002) Oral care reduces pneumonia in older patients in nursing homes.J Am Geriatr Soc 50: 430-433.
- Brady M, Furlanetto D, Hunter RV, Lewis S, Milne V (2006) Staff-led interventions for improving oral hygiene in patients following stroke.Cochrane Database Syst Rev : CD003864.
- Scannapieco FA1 (2006) Pneumonia in nonambulatory patients. The role of oral bacteria and oral hygiene.J Am Dent Assoc 137 Suppl: 21S-25S.
- Pace CC, McCullough GH (2010) The association between oral microorgansims and aspiration pneumonia in the institutionalized elderly: review and recommendations.Dysphagia 25: 307-322.
- van der Maarel-Wierink CD, Vanobbergen JNO, Bronkhorst EM, Schols JMGA, de Baat C (2013) Oral health care and aspiration pneumonia in frail older people: a systematic literature review. Gerodontology 30: 3-9.
- Martino R, Foley N, Bhogal S, Diamant N, Speechley M, et al. (2005) Dysphagia after stroke: incidence, diagnosis, and pulmonary complications.Stroke 36: 2756-2763.
- van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de Baat C (2011) Meta-analysis of dysphagia and aspiration pneumonia in frail elders.J Dent Res 90: 1398-1404.
- Baroni AF, Fábio SR, Dantas RO (2012) Risk factors for swallowing dysfunction in stroke patients.Arq Gastroenterol 49: 118-124.
- Sørensen RT, Rasmussen RS, Overgaard K, Lerche A, Johansen AM, et al. (2013) Dysphagia screening and intensified oral hygiene reduce pneumonia after stroke.J Neurosci Nurs 45: 139-146.
- Berry AM, Davidson PM, Nicholson L, Pasqualotto C, Rolls K (2011) Consensus based clinical guideline for oral hygiene in the critically ill.Intensive Crit Care Nurs 27: 180-185.
- Yildiz M, Durna Z, Akin S (2013) Assessment of oral care needs of patients treated at the intensive care unit.J Clin Nurs 22: 2734-2747.
- Prendergast V, Kleiman C, King M (2013) The Bedside Oral Exam and the Barrow Oral Care Protocol: translating evidence-based oral care into practice.Intensive Crit Care Nurs 29: 282-290.
- White R1 (2000) Nurse assessment of oral health: a review of practice and education.Br J Nurs 9: 260-266.
- Huskinson W, Lloyd H (2009) Oral health in hospitalised patients: assessment and hygiene.Nurs Stand 23: 43-47.
- Ozveren, H, Ozden, D (2015) Turkish nurses' attitudes and practices regarding oral care. Int J Nurs Knowl 26: 163-169.
- van der Putten GJ, Mulder J, de Baat C, De Visschere LM, Vanobbergen JN, et al. (2013) Effectiveness of supervised implementation of an oral health care guideline in care homes; a single-blinded cluster randomized controlled trial.Clin Oral Investig 17: 1143-1153.
- Kelly T1 (2010) Review of the evidence to support oral hygiene in stroke patients.Nurs Stand 24: 35-38.
- Jablonski RA1 (2012) Oral health and hygiene content in nursing fundamentals textbooks.Nurs Res Pract 2012: 372617.
- Durgude Y, Cocks N (2011) Nurses' knowledge of the provision of oral care for patients with dysphagia.Br J Community Nurs 16: 604-610.
- Forsell M, Kullberg E, Hoogstraate J, Johansson O, Sjögren P (2011) An evidence-based oral hygiene education program for nursing staff.Nurse Educ Pract 11: 256-259.
- Dolce MC, Haber J, Shelley D (2012) Oral health nursing education and practice program.Nurs Res Pract 2012: 149673.
- Park MS, Choi-Kwon S (2011) [The effects of oral care education on caregivers' knowledge, attitude, & behavior toward oral hygiene for elderly residents in a nursing home].J Korean Acad Nurs 41: 684-693.
- de Lugt-Lustig KH, Vanobbergen JN, van der Putten GJ, De Visschere LM, Schols JM, et al. (2014) Effect of oral healthcare education on knowledge, attitude and skills of care home nurses: a systematic literature review.Community Dent Oral Epidemiol 42: 88-96.
- Miller MD, Ferris DG (1993) Measurement of subjective phenomena in primary care research: the Visual Analogue Scale.Fam Pract Res J 13: 15-24.
- Kullberg E, Forsell M, Wedel P, Sjögren P, Johansson O, et al. (2009) Dental hygiene education for nursing staff.Geriatr Nurs 30: 329-333.
- Kuramoto C, Watanabe Y, Tonogi M, Hirata S, Sugihara N, et al. (2011) Factor analysis on oral health care for acute hospitalized patients in Japan.Geriatr Gerontol Int 11: 460-466.
- Clemmens DA, Kerr AR (2008) Improving oral health in women: nurses' call to action.MCN Am J Matern Child Nurs 33: 10-14.
- Lin YS, Chang JC, Chang TH, Lou MF (2011) Critical care nurses' knowledge, attitudes and practices of oral care for patients with oral endotracheal intubation: a questionnaire survey.J Clin Nurs 2 0: 3204-3214.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 14856
- [From(publication date):
December-2015 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 13511
- PDF downloads : 1345