Research Article Open Access
Nurses' Knowledge and Practice toward Gynecologic Oncology Palliative Care
Fatma Uslu-Sahan1 and Fusun Terzioglu2*1Department of Obstetrics and Gynecologic Nursing, Faculty of Nursing, Hacettepe University, Ankara, Turkey
2Dean of Faculty of Health Science and Director of Nursing Services of MLP Care, Istinye University, Istanbul, Turkey
- *Corresponding Author:
- Fusun Terzioglu, PhD, RN
Dean of Faculty of Health Science and Director of Nursing Services of MLP Care
Istinye University, Istanbul, Turkey
Tel: +90-212-481-3688
E-mail: fterzioglu@istinye.edu.tr
Received date: July 05, 2017; Accepted date: July 27, 2017; Published date: July 31, 2017
Citation: Uslu-Sahan F, Terzioglu F (2017) Nurses’ Knowledge and Practice toward Gynecologic Oncology Palliative Care. J Palliat Care Med 7:315. doi:10.4172/2165-7386.1000315
Copyright: © 2017 Uslu-Sahan F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objectives: Gynecologic cancers are the second main reasons for morbidity in women following breast cancer in Turkey and globally. The majority of patients with gynecologic cancer experience recurrence and die despite aggressive treatment. Because of this, patients with gynecologic cancers remain an ideal population for palliative care. Nurses are an essential part of the palliative care team in providing high standards of care since they spend the longest time with patients. The aim of the study to assess knowledge, practice and opinions about barriers toward palliative care among nurses working in gynecologic oncology units.
Methods: The cross-sectional survey-based study was conducted nurses (N=65) working in six tertiary care hospitals’ gynecologic oncology units in Ankara Province in Turkey. For data collection a survey was used. The descriptive statistics were used in data analysis.
Results: It was determined that 52.3% of the nurses did not receive any knowledge regarding palliative care. The knowledge nurses received was mostly about communication skills (96.8%), pain management (96.8%) and symptom control (96.8%). It was found that 73.8% of the nurses did not talk about death with patients and their families. One of the most common barriers faced by nurses was opioid phobia experienced by patients (66.2%) and healthcare professionals (41.5%).
Conclusions The current study indicates the need for wider coverage of palliative care in the education of preservice and in-service nurses to increase their knowledge and therefore practice. This education needs to be comprehensive in covering the basic principles of palliative care and symptom management and it should be distributed throughout the different courses to discuss palliative care within different contexts, such as gynecologic oncology setting.
Keywords
Palliative care; Palliative care nursing; Gynecologic neoplasms; Knowledge; Turkey
Introduction
It was estimated that 1,085,948 women in the world and 7,873 women in Turkey were diagnosed with gynecological cancer, approximately half of whom died of cancer [1]. Procedures of diagnosis and treatment applied for gynecologic cancers negatively influence patient and family quality of life in terms of body image, sexual identity, and ability of reproduction, in addition to the problems experienced in cancers in other organs [2,3]. Treatments administered during the disease process may remain ineffective [4-6], and the disease may progress or relapse [4,6,7]. Patients can experience numerous symptoms during the diagnosis and treatment process [3,5,6,8]. The symptom-related discomforts adversely affect the patients and their families and they result in poor treatment adherence [4,8].
In this respect, interest has increased in palliative care, which provides a holistic approach to patients with gynecologic cancer and their families [3,6-8]. The Society of Gynecologic Oncology (SGO) encourages maintaining and supporting qualified clinical care during the course of disease and states that it is important to integrate principles of palliative care into patient care [9]. In addition, the Society of Gynecologic Oncology (2013) emphasized that initiating basic palliative care in women with terminal or relapsed gynecologic cancer should not be delayed and these patients must be referred for special palliative care when appropriate [10]. Specialized palliative care has become a crucial part of healthcare systems and teamwork. The palliative care team is usually made up of medical doctors, dietetics, social workers and psychologists, nurses [11]. Nurses by the nature of their jobs play a major role in the palliative care team as they are usually in constant touch with patients and their families [11-14].
The national cancer control program was started in 2009 and palliative care was integrated into the program in 2010 in Turkey. In addition, the national palliative care program was prepared in 2009 and the Pallia-Turk project, which is a nurse-based, population-based project, was started in 2011 [15]. Along with these studies, palliative care units has been established in a few tertiary health care facilities recently and palliative care services have started to be provided in oncology units [13-15]. Although many positive developments related to the provision of services in some hospitals exist, lack of palliative care education and training opportunities is the most frequently reported barrier to the development of palliative care in Turkey [13,16,17]. Palliative care is general has not been yet integrated into the curriculum of nursing at both undergraduate and postgraduate level [13,17]. There is little palliative care education for undergraduate and postgraduate nursing students in some nursing schools [13,16] and this palliative care education is provided by faculty members who carry out studies in the field of oncology within the scope of undergraduate and/or graduate education programs [16]. Some nurses improve their knowledge and skills about palliative care by participating in congresses, symposiums, meetings, courses and workshops organized in our country and international meetings. These postgraduate learning programs rely mostly on reading material without clinical training [13,16].
To the best of our knowledge, in Turkey and recent literature, the knowledge, practice and opinions about barriers toward palliative care among nurses working in gynecologic oncology units have not previously been investigated. Previous works relating to palliative have been centered on the history and challenges of palliative care [8,13,18], and knowledge, attitude of nurses but non-specific to nurses working in gynecological oncology and the other health care professionals to palliative care [18-22]. Therefore, the value of the gynecologic oncology palliative care to nurses’ is unquestionable, and there is a need to support and educate nurses for the provision of high quality palliative care. Hence, the first step in developing a strategy to support and educate nurses about palliative care is to assess their current knowledge, practice and opinions about barriers. To this end, the aim of this is study was to assess knowledge, practice, and opinions about barriers toward palliative care among nurses working in gynecological oncology units.
Research questions
A cross-sectional survey-based study was used to answer the following research questions:
1. What is the current level of knowledge status regarding palliative care in this nurses sample?
2. Are demographic features of the nurses related to the knowledge status of palliative care?
3. What is the nurses' status of practice about nursing interventions regarding palliative care?
4. What are the nurses’ opinions about barriers toward palliative care?
Design, population and sample
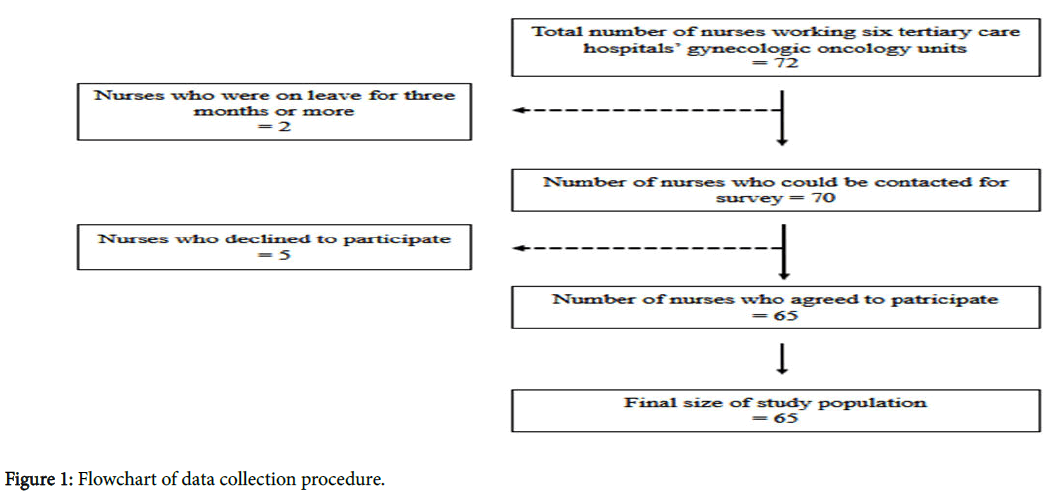
The current study was conducted in six tertiary care hospitals’ gynecologic oncology units in Ankara Province in Turkey. Ankara is the capital of Turkey and the country's second largest city. Almost all the patients with cancer in the Central Anatolia region of Turkey, particularly those living in the vicinity of Ankara, receive cancer treatment in these hospitals. These hospitals also provide palliative care to gynecologic cancer patients. The study was done with totally 72 nurses working in all gynecological oncology units these hospitals, sampling method was not used, because it was possible to reach all the samples. Because five nurses declined to participate and two nurses were on leave for three months or more, the study was performed with 65 nurses (respond rate 90%) (Figure 1).
Data were collected between July and September 2012. For data collection, a survey was used. This survey administered through faceto- face interviews. The interviews were conducted in time slots appropriate to the nurses’ time schedule, in a private room, and each interview took about 45 minutes.
Instrument
The survey was developed from tools used in previous studies, an extensive review of the literature, and clinical experience. Content validity was established through comparisons with the palliative care literature, with input from nationally recognized and published experts in gynecological oncology care. A small group (N=7) of nurses caring for gynecologic cancer patients from palliative care unit in other tertiary care hospital pilot-tested the survey. On the basis of their input, questions that seemed repetitive were deleted and the remaining questions were grouped in tabular format according to the topic, to improve clarity. Most questions were structured as Likert-scale responses.
The survey included four sections
The first section of the questionnaire is about the demographic features of the nurses (6 items): age, gender, occupation, educational status, the number of years on the job, and the period of time they have been working in a gynecological oncology unit.
The second section of the questionnaire includes 6 items pertaining the nurses’ knowledge status regarding palliative care: “Have you ever received knowledge about palliative care?”, “If yes, where?”, “What was the content of the knowledge?”, etc.
The third section includes items to examine the nurses’ status of practice about nine nursing interventions regarding palliative care: “I inform the patients and their relatives about the course of the disease as well as the treatment”, “I talk to the patients and their families about death”, “I provide support to the family after death”, etc.
The fourth section includes 10 items regarding the nurses’ opinions about barriers toward palliative care: “Lack of knowledge about palliative care by health care professionals”. ; “The standards regarding the symptom control are not known”; “Some palliative care programs, such as home care, are not covered by health insurance”, etc.
Statistical analysis
Study data were evaluated using the SPSS 21 statistics program (), and the number, percentage, and Chi-square test were used in the analysis. The significance level used was p<0.05.
Ethical considerations
Ethical approval was obtained from Non-interventional Clinical Trials Ethics Committee of Hacettepe University (number: # B. 30.2.HAC.0.05.07.00/663, date: July 26, 2012). All the nurses were given the right to choose whether or not to participate. However, completing the questionnaire was considered as an implicit agreement to take part in the study. Further, the identities (no names were requested) and hospitals of nurses were not revealed; only aggregate data was reported and nurses were assured that their responses would remain confidential.
Results
The mean age of the nurses was 33.2 years and most of them were female (98.5%). The average number of years the nurses have been on the job was 12.9 and the average time period they have been in a gynecological oncology unit was 4.4 years.
More than half of the nurses (52.3%) did not receive any knowledge regarding palliative care. Nurses’ who received knowledge regarding palliative care sources of knowledge was mostly during in-service education (71.0%). The knowledge they received was mostly about communication skills (96.8%), pain management (96.8%) and symptom control (96.8%). On the other hand, 67.7% of the nurses stated that the education they received regarding palliative care was not sufficient (Table 1).
| Nursing intervention regarding palliative care practices | Yes (%) | Partially (%) | No (%) |
|---|---|---|---|
| I apply nursing intervention to improve the quality of life of families | 30.8 | 35.4 | 33.8 |
| I inform the patients and their relatives about the course of the disease as well as the treatment | 21.5 | 43.1 | 35.4 |
| I talk to the patients and their families about death | 6.2 | 20 | 73.8 |
| I recognize impending death | 95.4 | 4.6 | 0 |
| I get the patients and their families ready for death by talking about it | 15.4 | 16.9 | 67.7 |
| I am sensitive to the patients' and families'spirutual requirements and cultural values | 72.3 | 27.7 | 0 |
| I observe the end-of-life ethical principles in palliative care | 100 | 0 | 0 |
| I know which unit of the hospital they could refer to in case of an ethical dilemma | 40 | 15.4 | 44.6 |
| I provide support to the family after death | 47.7 | 20 | 32.3 |
Table 1: Nurses’ knowledge status regarding palliative care.
There was no significant differences knowledge regarding palliative care status and in terms of age (χ²=1.976), educational level (χ²=0.444), the number of years on the job (χ²=1.061), the time period they have worked in a gynecological oncology unit (χ²=4.665) in the nurses (p>0.05).
In the current study it was stated that nurses fully adhered to the ethical principles of the end-of-life care practices (100.0%), they partly informed the patients and their families regarding the course of disease and treatment (43.1%), and they did not talk about death at all with the patients and their families (73.8%) (Table 2).
| Barriers toward Palliative Care Practice | I agree (%) |
I partially agree (%) |
I do not agree (%) |
I have no idea (%) |
|---|---|---|---|---|
| The health care professionals lack the knowledge regarding palliative care | 6.2 | 24.6 | 69.2 | 0 |
| The general public lacks the knowledge regarding palliative care | 4.6 | 15.4 | 80 | 0 |
| Lack of laws and regulation about palliative care | 3.1 | 10.8 | 46.2 | 40 |
| Some palliative care programs are not covered by health insurance | 16.9 | 6.2 | 35.4 | 41.5 |
| Opioid tolerance and addiction are usually mixed up by doctors | 32.3 | 36.9 | 27.7 | 3.1 |
| The standards regarding the symptom control are not known | 30.8 | 30.8 | 33.8 | 4.6 |
| The healthcare professionals have opioid phobia | 41.5 | 27.7 | 30.8 | 0 |
| The patients have opioid phobia | 66.2 | 15.4 | 18.5 | 0 |
| The availability of few numbers of opioid varieties | 43.1 | 26.2 | 29.2 | 1.5 |
| The availability of few numbers of opioid varieties and the difficulty in obtaining drugs from pharmacies | 36.9 | 26.2 | 33.8 | 3.1 |
Table 2: Nurses’ opinions about barriers toward palliative care practice.
The nurses agreed with the statement regarding the barriers that “the patient has opioid-phobia” (66.2%). They partially agreed with the statement “opioid tolerance and addiction are usually mixed up by doctors” (36.9%). The nurses did not agree with the statement “the general public lacks the knowledge regarding palliative care” (80.0%). The nurses had no idea about the statement “Some palliative care programs, such as home care, are not covered by health insurance” (41.5%) (Table 3).
| Nursing intervention regarding palliative care practices | Yes (%) | Partially (%) | No (%) |
|---|---|---|---|
| I apply nursing intervention to improve the quality of life of families | 30.8 | 35.4 | 33.8 |
| I inform the patients and their relatives about the course of the disease as well as the treatment | 21.5 | 43.1 | 35.4 |
| I talk to the patients and their families about death | 6.2 | 20 | 73.8 |
| I recognize impending death | 95.4 | 4.6 | 0 |
| I get the patients and their families ready for death by talking about it | 15.4 | 16.9 | 67.7 |
| I am sensitive to the patients' and families'spirutual requirements and cultural values | 72.3 | 27.7 | 0 |
| I observe the end-of-life ethical principles in palliative care | 100 | 0 | 0 |
| I know which unit of the hospital they could refer to in case of an ethical dilemma | 40 | 15.4 | 44.6 |
| I provide support to the family after death | 47.7 | 20 | 32.3 |
Table 3: Nurses’ nursing intervention regarding palliative care practices (N=65).
Discussion
Palliative care is one of the most important building blocks of the fight against cancer [9,11,23]. The World Health Organization projects the development of palliative care services for all countries and even recommends the establishment of a palliative care services network for low-income underdeveloped countries [23]. However, palliative care has traditionally not been one of the priority subjects in the training and work programs for healthcare professionals [21,22]. Few studies highlighted that healthcare professionals lack the training and knowledge regarding symptom management and palliative care skills [12,18-22]. In the present study, it was found that the nurses did not possess sufficient palliative care knowledge, and those who received education believed that the education they received was not sufficient. Turgay and Kav reported that 57.3% of the healthcare professionals received no palliative care education and 76.6% of those who received education believed that the education they received was not sufficient [22]. Prem et al. reported that 64.2% of the nurses did not have sufficient knowledge about palliative care [12]. The nurses’ lack of palliative care knowledge may negatively affect their communication patterns with the patients and their families, and reduce the quality of service provided to patients who are in need of palliative care.
There was no significant differences knowledge regarding palliative care status and in terms of age, educational level, the number of years on the job, the time period they have worked in a gynecological oncology unit in the nurses. Palliative care has become popular in recent years in Turkey, and the nurses working in the field of oncology especially have shown interest in it. It may be because palliative care traditionally has not been part of the priority subjects in healthcare professionals’ education programs and the nurses who received education believed that it was not sufficient.
Palliative care is a set of services provided to both patients and their families [11,14]. The aim of palliative care is to separate the terminal patients and to prepare them for death in peace, and to increase the life quality of patients and their families [11]. All of the nurses that participated in the present study stated that they observed the end-oflife ethical principles in palliative care; however, most of them did not know which unit of the hospital they could refer to in case of an ethical dilemma. Besides, they stated that they did not practice most of the nursing interventions, such as getting the patients and their families ready for death by talking about it. In the literature it has been reported that healthcare professionals do not feel comfortable talking about death [18] and they do not receive adequate training about the management of death and dying [24]; however, it has also been reported that it is crucial to get the palliative care patients and their families ready for imminent death to increase their quality of life [19-21]. This condition may be a result of the nurses’ lack of knowledge about palliative care and the lack of communication among nurses, patients, and their families.
There are numerous barriers to providing high-quality palliative care [8,18,20,21,24]. In the effective practice of palliative care, there are many barriers, such as pain management [8,18,20,21], miscommunication with the patients and their families and inappropriate announcement [18,20], legal issues [18,20,21], and the lack of knowledge experienced by doctors [8,18,20,21,24], nurses [18,20,21,24], patients [18,20,24] and the general society [18,20]. Most of the nurses in the current study stated that they face challenges about pain management in palliative care, such as the availability of few numbers of opioid varieties, the difficulty in obtaining drugs from pharmacies (36.9%) and the difficulties in prescribing medicine (43.1%). Mıyashıta et al. identified 95 barriers to providing effective palliative care (N=426) and highlighted the following barriers regarding pain management: there exists no effective pain control (N=35) and the medications are inadequate, too costly, or not covered by health insurance (N=27) [20]. Most of the nurses in the present study stated that patients (66.2%) and healthcare professionals (41.5%) have opioid phobia. Silbermann et al. studied the barriers in palliative care practices in the Middle East, including Turkey, and reported that the patients (97.5%) avoid the use of analgesics for fear of addiction and the healthcare professionals (97.7%) avoid administering analgesics for the same reason [18]. Furthermore, most of the nurses in the present study did not cite the lack of knowledge experienced by the general public and the healthcare professionals as one of the barriers toward palliative care. However, previous studies have reported healthcare professionals’ lack of knowledge and skills (47.7%-97.7%) [18,20], and the general public’s lack of knowledge (28.6%) [20] and awareness (98.1%) [18] regarding palliative care among the barriers providing palliative care. Identification and elimination of barriers experienced in palliative care play a crucial role in providing effective palliative care.
Limitations of the study
The present study has some limitations. The study included nurses working in gynecological cancer units at the participating hospitals. The study data included only the self-report of the nurses that participated in the study. Therefore, the results of our study may not be generalized for the whole nurses working with cancer patients, it may reflect the nurses working with gynecological cancer patients. Furthermore, this study conducted in one city of the Turkey, which may limit the generalizability of its findings and therefore further research is required to explore national trends.
Conclusion
The literature suggest that nurses who provide palliative care for patients with gynecologic cancer and their families can have a prominent role in palliative care. Hence it is important to assess nurses’knowledge, practice and opinions about barriers to help them handle such cases. The result of this study suggested that the nurses working in gynecological oncology units lack the knowledge and did not practice interventions about palliative care that were reported in the literature regarding palliative care. Besides, they were observed to face barriers adversely affecting the quality of palliative care provided to the patients with gynecologic cancer. In conclusion, the current study indicates the need for wider coverage of palliative care in the education of pre-service and in-service nurses to increase their knowledge and therefore practice. In addition, this education needs to be comprehensive in covering the basic principles of palliative care and it should be distributed throughout the different courses to discuss palliative care within different contexts, such as gynecologic oncology setting.
In 2015, “Palliative Care Nursing Certificate Program” including clinical practice started by the Turkish Ministry of Health [25]. This program with an aim to embellish the palliative care nurses with the knowledge, skills, and attitudes required by their profession. Via this certification program, all palliative care nurses in all provinces of Turkey are aimed to be covered. The nurses working in palliative care units and oncology units have started to get certificates. To increase the quality of palliative care to patients with gynecologic cancer and their families, nurses working in gynecologic oncology should get the Palliative Care Nursing Certificate and evidence-based palliative care practices protocols should be developed.
Acknowledgment
The authors are grateful to all the nurses who participated in this study and the authorities of the hospitals who supported the study.
References
- http://globocan.iarc.fr/Pages/summary_table_site_sel.aspx
- Nazik E, Ozdemir F, Soydan S (2014) Social support and quality of life in Turkish patients with gynecologic cancer. Asian Pac J Cancer Prev 15: 3081-3086.
- Terzioglu F, Sahan Uslu F (2016) Palliative Care in Gynecologic Cancers. J Palliat Care Med 6: 1-3
- Zakhour M, LaBrant L, Rimel BJ, Walsh CS, Li, AJ, et al. (2015) Too much, too late: aggressive measures and the timing of end of life care discussions in women with gynecologic malignancies. Gynecol Oncol 138: 383-387.
- Pathy S, Raheja SG, Rakhi S (2008) Palliative care in advanced gynecological cancers: institute of palliative medicine experience. Indian J Palliat Care 14: 86-89.
- Mishra K (2011) Gynaecological malignancies from palliative care perspective. Indian J Palliat Care 17: 45-51.
- Eskander RN, Osann K, Dickson E (2014) Assessment of palliative care training in gynecologic oncology: A gynecologic oncology fellow research network study. Gynecol Oncoly 134: 379-384
- Rezk Y, Timmins PF, Smith HS (2011) Palliative care in gynecologic oncology. Am J Hosp Pallıat Care 28: 356-374.
- Smith TJ, Temin S, Alesi ER, Abernethy AP, Balboni TA (2012) American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 30: 880-887.
- https://www.sgo.org/choosing-wisely/
- http://www.who.int/cancer/media/FINAL-PalliativeCareModule.pdf
- Prem V, Karvannan H, Kumar SP, et al (2012) Study of nurses’ knowledge about palliative care: a quantitative cross-sectional survey. Indian J Palliat Care 18: 122-127.
- Terzioglu F, Sahan Uslu F, Boztepe H (2015) Palliative care to the cancer patient: Turkish perspectives. J Palliat Care Med 5:1-4.
- Wheeler, MS (2016) Primary palliative care for every nurse practitioner. J Nurse Pract. 12: 647-653
- http://kanser.gov.tr/Dosya/NCCP_2013-2018.pdf
- Can, G (2015) The implementation and advancement of palliative care nursing in Turkey. J Palliat Care Med 5: 1-8.
- Kebudi R, Çakır FB, Gultekin M (2014) Palliative care to the cancer patient in Turkey, Sılbermann M (eds) palliative care to the Cancer Patient New York.193-210.
- Silbermann M, Fink RM, Min SJ (2015) Evaluating palliative care needs in middle eastern countries. J Palliat Med 18:18-25.
- Ferrell B, Virani R, Mallay P (2010) The preparation of oncology nurses in palliative care. Semin Oncol Nurs 26: 259- 265
- Miyashita M, Sanjo M, Morita T (2007) Barriers to providing palliative care and priorities for future actions to advance palliative care in Japan: a nationwide expert opinion survey. J Palliat Med 10: 390-399.
- Paıce JA, Ferrell BR, Coyle N (2008) Global efforts to ımprove palliative care: The international end-of-life nursing education consortium training programme. J Adv Nurs 61: 173–180.
- Turgay G, Kav S (2012) Turkish healthcare professionals' views on palliative care. J Palliat Care 28: 267-273.
- Boyle P, Levin B (2008) World cancer report. Lyon: IARC Press.
- Ahmed N, Bestall JC, Ahmedzai SH (2004) Systematic review of the problems and issues of accessing specialist palliative care by patients carers and health and social care professionals. Palliat Med 18: 525–542
- The Turkish Ministry of Health (2015) Palliative care nursing certificate program.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 4139
- [From(publication date):
July-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 3237
- PDF downloads : 902