Short Communication Open Access
Number of Circulating Apoptotic Endothelial Cell-Derived Micro Particles as a Predictor of Metabolically Unhealthy Obesity
1Private Medical Center “Vita-Center”, Zaporozhye, Ukraine
2Internal Medicine Department, State Medical University, Zaporozhye, Ukraine
- *Corresponding Author:
- Alexander E Berezin
Consultant of Therapeutic Unit
Internal Medicine Department
State Medical University of 26, Sedova str
3, Mayakovsky av, Zaporozhye, Ukraine
Tel: 380612894585
E-mail: dr_berezin@mail.ru
Received Date: February 02, 2017; Accepted Date: Apr 26, 2017; Published Date: May 02, 2017
Citation: Berezin AE (2017) Number of Circulating Apoptotic Endothelial Cell-Derived Micro Particles as a Predictor of Metabolically Unhealthy Obesity. J Mol Immunol 2:109.
Copyright: © Berezin AE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Molecular Immunology
Abstract
Obesity is considered a main factor contributing in diabetes mellitus development and a predictor of CV disease and events. Based on the Adult Treatment Panel-III criteria subjects with established obesity and co-existing other metabolic abnormalities including dyslipidaemia, insulin resistance (IR), increased fasting glucose and impaired glucose tolerance, are referred metabolically unhealthy obesity (Met-UHO), whereas obese individuals without these abnormalities might be defined as metabolically healthy obesity (Met-HO). The mechanisms underlying the change in phenotype from metabolically healthy to metabolically unhealthy obesity are still unclear. It has been postulated that apoptotic endothelial cell-derived micro particles (EMPs) might be a trigger of endothelial cell dysfunction and as well as a mediator on vascular repair. Moreover, the imbalance in circulating number of various types of EMPs may influence the risk of transformation of Met-HO into Met-UHO. The short communication is depicted the role of apoptotic EMPs in obesity phenotype modification.
Keywords
Metabolically healthy obesity; Metabolically unhealthy obesity; Endothelial cell-derived micro particles; Insulin resistance
Abbreviations
EMPs: Endothelial Cell-Derived Micro Particles; VAT: Visceral Adipose Dysfunction; CV: Cardiovascular; IR: Insulin Resistance.
Introduction
The prevalence of abdominal obesity has been raised worldwide achieving epidemic level [1]. Recent observation and clinical studies have clearly established that abdominal obesity especially morbid obesity (body mass index [BMI] more than 40 kg/m2) related strongly to all cause and cardiovascular (CV) morbidity and mortality, as well as closely associated with a risk of type 2 diabetes mellitus (T2DM) [2]. However, there is evidence regarding progressive annually increase of prediabetes/T2DM prevalence irrespectively BMI [3,4]. Additionally, obese individuals with similar BMI may be protected or opposite predisposed to obesity-related complications (i.e. T2DM, dyslipidaemia, and hypertension) and CV disease [5]. The speculations around so called a protective role of obesity in CV disease leaded to appearance of a term “obesity paradox”, which is referred as shaping Ucurve between BMI and CV mortality [6]. It is suggested that “obesity paradox” might be a mismatch between different definitions of obesity in particularly based on BMI measurement. Therefore, the heterogeneity of obesity induced the concept of emerging metabolic phenotypes associated with obesity e.g. metabolically unhealthy obesity (Met-UHO) and metabolically healthy obesity (Met-HO) distinguished from each other for CV risk [7]. Based on the Adult Treatment Panel-III criteria subjects with established obesity and coexisting other metabolic abnormalities including dyslipidaemia, insulin resistance (IR), increased fasting glucose and impaired glucose tolerance, are referred Met-UHO, whereas obese individuals without these abnormalities might be defined as Met-HO [8]. The mechanisms underlying the change in phenotype from metabolically healthy to metabolically unhealthy obesity are still unclear. Whether Met-HO is an early stage and transient state in the pathway to Met-UHO and T2DM is not understood.
Micro particles (MPs) are defined a heterogeneous sub-population of extracellular vesicles with diameter average from 100 to1000 nm originated from plasma membranes of mother’ cells [9]. As a derivate of cellular membrane MPs are discussed powerful paracrine regulators of target cell structure and functions. MP released by apoptotic endothelial cells posse a wide spectrum of biological effects on intercellular communication by transferring different active molecules (proteins, peptides, hormones, growth factors, microRNAs) exhibiting coagulation activity, mediating cell growth and tissue differentiation [10]. Additionally, apoptotic endothelial cell-derived MPs (EMPs) may directly worse endothelial integrity and vascular function playing a pivotal role in development of micro vascular inflammation and IR [11].
Recent clinical studies have shown that the circulating levels of apoptotic EMPs were significantly increased in T2DM patients as compared with healthy volunteers [12] and they mediated CV risk in patients with established metabolic syndrome (MetS) and T2DM [13-15]. Probably apoptotic EMPs may involve in the transformation of Met-HO into Met-UHO determining the risk of T2DM and CV disease. Indeed, the increased number of CD31+/Annexin V+ and CD144+/Annexin V+EMPs much more pretty accurate predicted Met- UHO and closely associated with IR [16]. Thus, the most important factor that affects metabolic dysregulation in obesity is IR, which probably appears to be predominantly early stage of the Met-HO.
There is evidence that an accumulation of visceral adiposity tissue (VAT) might associate with over-production of pro-inflammatory cytokines including hs-CRP, leptin and vistafin and induce IR [17].
Therefore, infiltration of the sub-intima by LDL cholesterol may induce production of free radicals, oxidation of cytoskeleton and membrane vesiculation of endothelial cells. Finally, membrane vesiculation of endothelial cells is enhanced by inflammatory cytokines in conveying of VAT accumulation.
Interestingly, the circulating number of apoptotic EMPs has well associated with conventionally obesity biomarkers (adiponectin, leptin, vistafin) in Met-UHO patients, but did not in Met-HO individuals. Indeed, in Met-HO patients we did not find severe metabolic abnormalities apart from leptin elevation compared with Met-UHO, however, IR was determined as common finding for both Met-UHO and Met-HO individuals without a difference in BMI.
The increased amount of VAT together with a chronic inflammation and IR predisposes to the development of endothelial dysfunction through attenuation synthesis and secretion of apoptotic EMPs. Indeed, pro-inflammatory cytokines, i.e. interleukin-6, tumor factor necrosis-alpha, leptin, and vistafin, may directly influence structure of endothelial cells and trigger a secretion of apoptotic EMPs [18-20]. The main biological function of this process is an attenuation of endothelial cell repair and recovery of vascular function [21]. Unfortunately, coexisting IR affects endothelial progenitor cells and they are not able to differentiate into functionally mature endothelial cells even after stimulation by apoptotic EMPs [22]. As a result, apoptotic EMPinduced endothelial dysfunction and IR may become an early predictor of shaping Met-UHO.
Recently it has reported that apoptotic EMPs may independent predict asymptomatic atherosclerosis and CV disease in T2DM patients [23], while their role in individuals with different phenotypes of obesity has remained controversial. First, it is not clear whether increased number of apoptotic EMPs is adaptive mechanism of vascular repair or factor of endothelial injury. Indeed, circulating EPMs, which are enhanced in a large number of metabolic disorders including abdominal obesity, associated with IR and this has been linked to deleterious effects on endothelial cells [24,25]. At the same time, apoptotic EPMs are powerful factor contributing in endothelial progenitor cell mobbing and differentiation. Secondary, it is not fully understand the innate molecular mechanisms, which correspond to triggers of secretion of these apoptotic MPs.
Apoptotic MPs as cargo microvesicles consist of a variety of biomolecules including regulated proteins, DNA, mRNA, and noncoding RNA [23]. The proportion of these components as well as an entire secretome is under a tight control of autocrine/paracrine mechanisms and inflammatory factors (i.e. tumor necrosis factoralpha, interleukin-2, -6), which induces EMP formation in a timedependent manner [9,10,5]. Consequently, the final reply of the recipient cells, such as endothelial progenitor cells, is depends on epigenetic regulation of secretome secretion and primary trigger, which affects vesiculation [10].
Recent animals and pre-clinical studies have shown that some epigenetic changing affected both histone H3K4me3 and H3K9me2 have significantly modified in isolated adipocytes that derived from abdominal obesity individuals with T2DM [26]. However, in patients with Met-HO, there was no a sufficient difference of the levels of H3K4me3 and H3K9me2 compared with normal healthy ones. Thus, these findings indicated that alternation of chromatin structures is involved in the transformation from obesity to T2DM, even plays a pivotal role for the development of metabolic disorder. Additionally, since H3K4me3 and H3K9me2 is associated with gene activation and suppression respectively [27], understanding the chromatin loci that displayed differentially established H3K4me3 and H3K9me2 in Met- UHO and Met-HO patient. Interestingly, as recent study also indicated that the modifier of H3K9me2 also interacts with DNA methyltransferases and protects DNA methylation [28], investigation the patterns of DNA methylation in obesity patient derived adipocytes might also shed light on the potential targets that involved in the processing of T2DM. On the other hand, DNA methyltransferases is considered an innate mechanism, which plays an important role in modification of secretome including MPs. Probably, genetic modification of MPs might be a sufficient component of switching Met-HO to Met-UHO and T2DM development.
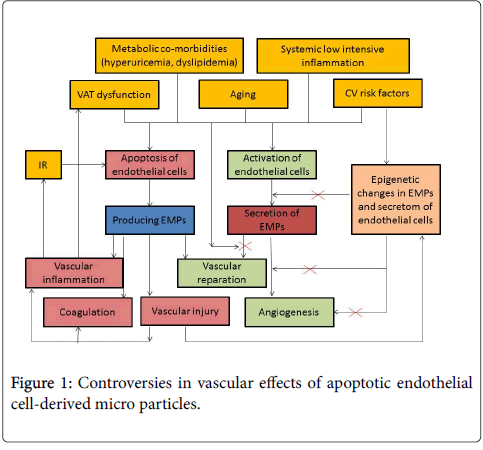
Thus, apoptotic endothelial cell-derived micro particles (EMPs) might be a trigger of endothelial cell dysfunction and as well as a mediator on vascular repair (Figure-1).
Obviously, an ability of apoptotic EMPs to modulate immune and inflammatory processes, coagulation and vascular function, angiogenesis and vascular injury may interact with other regulatory mechanisms the role of witch in the pathogenesis of abdominal obesity requires still being determined. It is no excluded that release of apoptotic EMPs might act as a direct endogenous survival signal for target cells.
In conclusion, measurement of circulating apoptotic EMP number would be useful tool for stratification amongst obesity individuals at higher risk of T2DM and CV, especially when conventional biomarkers of obesity are not detected in appropriate diagnostic level. Large investigations are required to understand the role of apoptotic EMPs in pathogenesis of different phenotypes of abdominal obesity, because they may be a target of the therapy as well as predictive biomarkers.
References
- Flegal KM, Carroll MD, Ogden CL, Curtin LR (2010) Prevalence and trends in obesity among US adults, 1999-2008. JAMA 303: 235-241.
- Vanuzzo D, Pilotto L, Mirolo R, Pirelli S (2008) Cardiovascular risk and cardiometabolic risk: an epidemiological evaluation. G ItalCardiol 9: 6S-17S.
- Rey-López JP, de Rezende LF, Pastor-Valero M, Tess BH (2014) The prevalence of metabolically healthy obesity: a systematic review and critical evaluation of the definitions used. Obesity Reviews 15: 781-790.
- Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, et al. (2011) on behalf of the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 377: 557-567.
- Rydén L, Grant PJ, Anker SD, Berne C, Cosentino F, et al. (2013) ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 34: 3035-3087.
- Brede S, Serfling G, Klement J, Schmid SM, Lehnert H (2016) Clinical Scenario of the Metabolic Syndrome. Visc Med 32: 336-341.
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) (2002) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report, Circulation 106: 143-421.
- Ashwell M, Gunn P, Gibson S (2012) Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev 13: 275-286.
- Berezin A, Zulli A, Kerrigan S, Petrovic D, Kruzliak P (2015) Predictive role of circulating endothelial-derived microparticles in cardiovascular diseases. ClinBiochem 48: 562-568.
- Alexandru N, Badila E, Weiss E, Cochior D, Stępień E, (2016) Vascular complications in diabetes: Microparticles and microparticle associated microRNAs as active players. BiochemBiophys Res Commun 472: 1-10.
- Berezin AE, Kremzer AA, Cammarota G, Zulli A, Petrovic D, et al. (2016) Circulating endothelial-derived apoptotic microparticles and insulin resistance in non-diabetic patients with chronic heart failure. ClinChem Lab Med 54: 1259-1267.
- Berezin AE, Kremzer AA, Berezina TA, Martovitskaya YV (2016) The pattern of circulating microparticles in patients with diabetes mellitus with asymptomatic atherosclerosis. ActaClinBelg 71: 38-45.
- Berezin AE, Kremzer AA, Martovitskaya YV, Berezina TA, Gromenko EA (2016) Pattern of endothelial progenitor cells and apoptotic endothelial cell-derived microparticles in chronic heart failure patients with preserved and reduced left ventricular ejection fraction. EBioMedicine 4: 86-94.
- Berezin AE, Kremzer AA, Berezina TA, Martovitskaya YV (2015) Pattern of circulating microparticles in chronic heart failure patients with metabolic syndrome: Relevance to neurohumoral and inflammatory activation. BBA Clin 4: 69-75.
- Agouni A, Andriantsitohaina R, Martinez MC (2014) Microparticles as biomarkers of vascular dysfunction in metabolic syndrome and its individual components. CurrVascPharmacol 12: 483-492.
- Berezin A, Kremzer A, Berezina T, Martovitskaya Y, Samura T (2017) Circulating apoptotic endothelial cell-derived micro particles are predicted metabolically unhealthy obesity. Biomed Res Ther 4: 1110-1128.
- Berezin A (2016) Endothelial progenitor cells dysfunction and impaired tissue reparation: the missed link in diabetes mellitus development. Diabetes & Metabolic Syndrome: Clinical Research & Reviews.
- Rautou PE, Vion AC, Amabile N, Chironi G, Simon A, (2011) Microparticles, vascular function, and atherothrombosis. Circ Res 109: 593-606.
- Jansen F, Yang X, Baumann K, Przybilla D, Schmitz T, et al. (2015) Endothelial microparticles reduce ICAM-1 expression in a microRNA-222-dependent mechanism. J Cell Mol Med 19: 2202-2214.
- Tetta C, Bruno S, Fonsato V, Deregibus MC, Camussi G (2011) The role of microvesicles in tissue repair. Organogenesis 7: 105-115
- Martinez MC, Andriantsitohaina R (2011) Microparticles in angiogenesis: therapeutic potential. Circ. Res 109: 110-119.
- Berezin A (2016) Biomarkers for cardiovascular risk in diabetic patients. Heart 102: 1939-1941.
- Montoro-García S, Shantsila E, Marín F, Blann A, Lip GY (2011) Circulating microparticles: new insights into the biochemical basis of microparticle release and activity. Basic Res. Cardiol 106: 911-923.
- Berezin AE, Kremzer AA, Samura TA, Berezina TA, Kruzliak P (2015) Immune phenotypes of endothelial-derived microparticles in dysmetabolic patients. J Proteomics Bioinformatics 8: 60-66.
- Berezin A (2016) Cardiac biomarkers in diabetes mellitus: new dawn for risk stratification? Diabetes & Metabolic Syndrome: Clinical Research & Reviews.
- Jufvas A, Sjödin S, Lundqvist K, Amin R, Vener AV, (2013) Global differences in specific histone H3 methylation are associated with overweight and type 2 diabetes. Clin Epigenetics 5: 15.
- Portela A, Esteller M (2010) Epigenetic modifications and human disease. Nat Biotechnol 28: 1057-1068.
- Zhang T, Termanis A, Özkan B, Bao XX, Culley J, et al. (2016) G9a/GLP Complex Maintains Imprinted DNA Methylation in Embryonic Stem Cells. Cell Rep 15: 77-85.
Relevant Topics
- Bacteriostatic antibiotics
- Cell signaling and activation
- Chemokines
- Class I MHC molecules
- Class II MHC molecule
- Colitis Antibiotics
- Immune response
- Immunochemistry
- Immunogenicity of biopharmaceuticals
- Immunogenomics
- Immunoglobulins
- Immunoglycomics
- Immunomodulatory xenobiotics
- Immunopharmacology
- Immunoproteomics
- Immunosenescence
- Immunotolerance
- Molecular Immunology
- Non classical MHC class I molecules
Recommended Journals
Article Tools
Article Usage
- Total views: 2504
- [From(publication date):
June-2017 - Apr 01, 2025] - Breakdown by view type
- HTML page views : 1741
- PDF downloads : 763