Case Report Open Access
Non-Healing Wounds Associated with Klippel-Trenaunay Weber Syndrome: A Case Report
Paul A Andrew Stone1*, Kevin Blue1, Alan Synn2 and Alan Ng11Highlands Presbyterian St. Lukes Podiatric Medical and Surgical Residency, Denver CO, United States
2Vascular Institute of the Rockies, Clinical Instructor for the Highlands Presbyterian St. Lukes Podiatric Medical and Surgical Residency, Denver CO, United States
- *Corresponding Author:
- Stone PAA
Advanced Orthopedics and Sports Medicine Specialists, P.C.
Director Highlands Presbyterian St. Lukes Podiatric Medical and Surgical Residency
Denver CO United States Tel: +27219593229/2190
Fax: +278615107002
E-mail: ombamalu@uwc.ac.za
Received date: April 28, 2016; Accepted date: July 9, 2016 Published date: July 15, 2016
Citation: Stone PAA, Blue K, Synn A, Ng A (2016) Non-Healing Wounds Associated with Klippel-Trenaunay Weber Syndrome: A Case Report. Clin Res Foot Ankle 4:191. doi: 10.4172/2329-910X.1000191
Copyright: © 2016 Stone PAA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
A review of Klippel-Trenaunay Weber Syndrome (KTWS) precedes a case of a patient with Non-Healing Wounds secondary to the aforementioned rare congenital syndrome. Successful treatment for these ulcerations is then outlined. A discussion follows tying KTWS to modem venous hypertensive wound care techniques. We believe this is the only report of its type targeting lower extremity practitioners involved with wound care.
Keywords
Klippel-Trenaunay Weber Syndrome; Venous; Wound; Ulcer
Introduction
In 1900, two renowned French physicians, Maurice Klippel and Paul Trenaunay first described the syndrome that now bears their name. They termed the condition "naevus vasculosus osteohypertophicus" after reporting on two patients presenting with a port wine stain and varicosities of an extremity associated with hypertrophy of the affected limb's bone and soft tissue [1]. Seven years later, Weber reported on three patients with the aforementioned symptoms as well as arteriovenous malformation of the affected extremity [2]. Today, Klippel-Trenaunay-Weber Syndrome (KTWS) is described as a rare congenital medical condition in which blood vessels and/or lymph vessels fail to form properly and is characterized by the triad of a portwine stain or stains (nevus flemmeus), varicose veins and lymphatic malformations with bony and soft tissue hypertrophy involving only one extremity [3].
Several theories exist as to the exact etiology of KTWS. Bliznak and Staple suggest that KTWS is caused by intrauterine damage to the sympathetic ganglia or intermediolateral tract which leads to dilated microscopic arteriovenous anastomoses [4]. Baskerville et al. suggests that there is an embryological developmental abnormality of mesodermal tissues affecting angiogenesis [5]. Servelle believes that deep vein abnormalities, with resultant obstruction of venous flow, lead to venous hypertension, the development of varices, and limb hypertrophy [6]. Still further, McGrory and Amadilo contend that an underlying mixed mesodermal and ectodermal dysplasia is likely responsible for the development of KTWS [7].
Genetically, KTWS effects men and women equally and does not display racial predilection. Genetic testing continues to be ongoing but initial reports suggest that an association between angiogenic factor gene AGGF1 and KTWS exists [8].
KTWS is a rare and complex syndrome. Manifestations of the syndrome usually present at birth and 75% of patients have symptoms by the age of 10. Treatment is rendered on a case-by-case basis. The purpose of this study was to present a case of a young man who underwent endovascular treatment for KTWS as a 6 month old infant and presented to our wound healing center with manifestations of painful non-healing wounds at the age of 28. His case, including treatments rendered, is outlined and a discussion follows.
Case Presentation
A 28 y/o relatively healthy and active male mechanic with a history of Klippel Trenaunay Weber syndrome presented on referral from a respected local dermatologist to the wound healing center with a chief complaint of painful non-healing wounds on the outside of his right leg and ankle. The patient stated that the wounds had been present for approximately four years on his right lower leg and one month on his ankle. He reported that the lesion began as a flat quarter sized "mole" that was tender to touch. l-k initially presented to a dermatologist who promptly biopsied the lesion. The biopsy report was read as exhibiting extensive stasis changes and numerous siderophages (Macrophages containing hemosiderin). Prior treatments included antibiotic cream, moisturizing cream, and compression stockings. No debridement had been undertaken up to this point.
The patient had a past medical history consisting of congenital Klippel-Trenaunay Weber Syndrome which affected his right leg and caused excessive swelling and girth since birth. Medical records were obtained from when the patient was six months old and underwent successful and uncomplicated embolization of arteriovenous malformations in his right posterior hip and thigh following a trial of steroids to decrease the size of the vessels.
The patient's medications consisted of lisinopril for mild hypertension and cardiomegaly. He had no known drug allergies. Socially, the patient denied alcohol or tobacco abuse.
He lived alone in a nearby apartment and worked full time on his feet as a car mechanic. His family history was positive for hypertension on his mother and father's side and diabetes mellitus on his father's side.
His review of systems was otherwise negative aside from the chief complaint and past medical history.
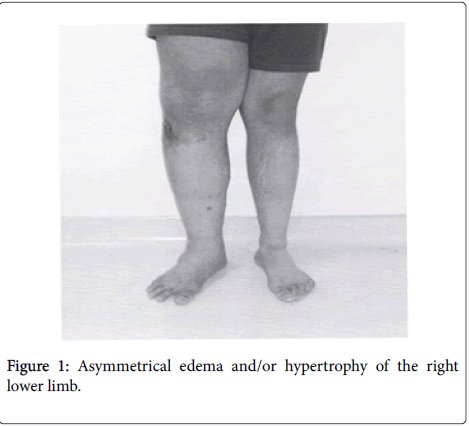
On physical exam the patient's vital signs were stable. Generally, he was alert and oriented, in no apparent distress, was well developed, well-nourished and appeared stated age. His axial exam was all within normal limits including a regular heart rate and rhythm and clear lung fields. His extremity exam demonstrated asymmetrical edema and hypertrophy of his right lower limb (Figure 1).
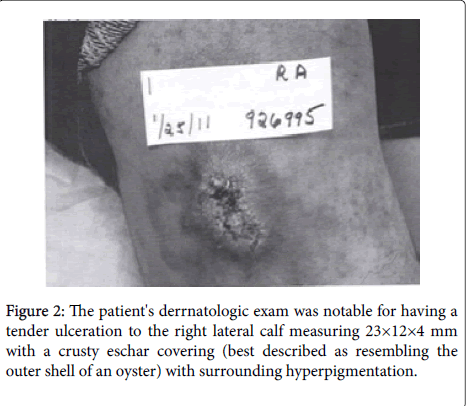
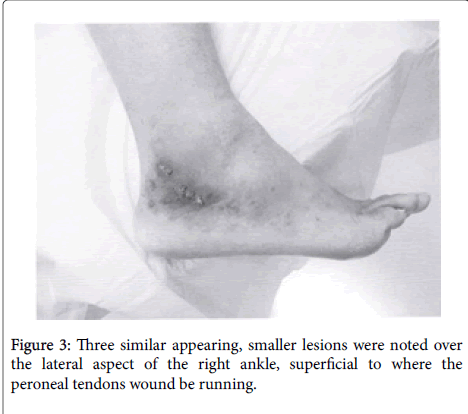
.His muscle strength was 5/5 in the affected limb both with extention and flexion at the knee and hip as well as in all four quadrants in the lower leg. His range of motion at the level of the hip, knee, ankle, sub talar joint and mid tarsal joint was all full and fluid. The patient's vascular exam demonstrated a palpable femoral pulse bilaterally, an absent popliteal pulse on the right and absent pedal pulses. The patient's dermatologic exam was notable for having a tender ulceration to the right lateral calf measuring 23×12×4 mm with a crusty eschar covering (best described as resembling the outer shell of an oyster) with surrounding hyperpigmentation (Figure 2). Three similar appearing but smaller lesions were noted over the lateral aspect of the right ankle, superficial to the peroneal tendons (Figure 3).
Follow up was scheduled for 1 week following the patient's initial appointment with instructions to keep the wound clean under sterile dressings and obtain non-invasive arterial and venous studies prior to his next appointment. The patient complied and pulse volume recordings completed bilaterally from the level of the ankle distally displayed bilateral waveforms within normal limits with dampening at the toe level. Bilateral resting ankle brachial index's were within normal limits as well and the exam findings were read as not suggestive of peripheral arterial disease. Venous ultrasound was also completed with no evidence to suggest deep or superficial venous thrombosis or superficial venous insufficiency involving the greater saphenous vein or lesser saphenous vein. Duplex findings did suggest however that deep venous insufficiency involving the femoral vein and popliteal vein existed with two incompetent perforators on the lateral aspect of the leg below the knee. The first measured 5 mm and was located approximaterly 30 cm proximal to the lateral malleolus in the region of the non-healing wound. The second measured 3.9 mm and was located at the lateral malleolus approximately 1-2 cm proximal to the ankle non-healing wound.
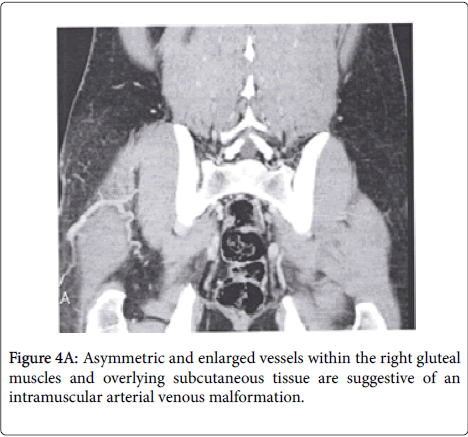
In response to the patient's abnormal venous ultrasound, a CT venogram of the abdomen and pelvis was ordered in order to discern whether a congenital anomaly of venous outflow of the right lower extremity remained despite his history of embolism of AVmalformations as a child. The exam was completed as ordered prior to his third clinic visit and demonstrated symmetric and enlarged vessels within the right gluteal muscles and overlying subcutaneous tissue which were suggestive of an intramuscular arterial venous malformation. Additionally, there were enlarged right external iliac, internal iliac, and common femoral veins.
Though no discreet arterial venous connection was identified, the magnitude of these veins suggested this possibility.
Also of note was a duplicated left sided inferior vena cava, which drained into the left renal vein (Figure 4).
A diagnostic aortogram with bilateral runoff and concurrent inferior vena cavogram with bilateral lower extremity venogram to rule out any AV-malformations in his iliac region on the right was performed. The intent was to possibly embolize any arterial flow into a vascular malformation.
The patient's study, as read by the senior author (A.S.), showed sizable trans-pelvic collaterals flowing from left to right in the venous plexus emanating between the internal iliac veins. Also, a persistent left sided vena cava was realized as previously visualized on the CT scan. There was no evidence of arteriovenous fistula however, even though the right iliac venous system was markedly enlarged with multiple collateral vessels (Figure 5).
Wound care throughout the patients course focused on the theory that venous hypertension was the driving force behind the inability for these wounds to heal.Having excluded residual arteriovenous malformations, the clinical focus remained local wound care rather than complex endovascular interventions.
Compressive stockings at 30-40 mmHg were ordered to control edema, at first to the level of the knee and then up the hip when the knee-highs were found to be intolerable.
Although uncomfortable, and with the aid of a 5% emulsion preparation, containing 2.5% each of lidocaine/prilocaine as local anesthetic, sharp debridement of the ulcerations were undertaken with a 15 blade through the subcuticular layer.
No cellulitis or purulent drainage was noted upon debridement and all wounds continued to granulate nicely underneath the overlying eschar. Initially, Promogran, (Ethicon, a division of Johnson and Johnson, New Brunswick, New Jersey) a sterile, freeze dried matrix composed of collagen and oxidised regenerated cellulose, formed into a sheet approximately 3 mm thick, was utilized as dressing under his compressive stockings. Neoprene pads were added at the level of the ankle to increase the effectiveness of his compressive stockings.
When the calf wound transitioned from deep full thickness to superficial, which occurred 3 months following his initial presentation and one month following resolution of his ankle wounds, an antimicrobial wound gel (Anacept, Anacapa Technologies Inc, San Dimas, CA) was added in place of Promogran in an attempt to help moisten the superficial wound bed and keep debris from forming the eschar following his debridements. This proved successful and the patient was healed and discharged from clinic in 4 months time (Figure 6).
Discussion
Non-healing ulcerations secondary to venous hypertension have long been and continue to be a challenge for wound care physicians around the world. Bandaging venous leg ulcers in compressive stockings is an ancient treatment and has been used since 3500 BC. Randomized double-blinded prospective evidence is available which demonstrates that compressive bandaging promotes healing of venous ulcers.
Recently Partsch et al. concluded in an extensive review of 2548 patients that compression stockings, particularly those of 20-30 mm Hg or greater, and compression bandaging lead to reductions in edema, venous diameter, venous reflux and to improvement in the function of the calf muscle pump [9]. Dressings applied under compressive dressings have long been utilized as a means to wick away excess moisture and drainage from venous wounds, most of which currently incorporate a topical impregnated antibiotic to lessen bioburden. A recent Cochrane Database Systematic Review identified 42 randomized controlled studies comparing commonly utilized dressings for venous ulcerations. The main dressing types evaluated were hydrocolloids (n = 23), foams (n = 6), alginates (n = 4), hydrogel dressings (n = 6) and a group of miscellaneous dressings (n = 3). In none of the comparisons was there evidence that any one dressing type was better than others in terms of number of ulcers healed, as long as the dressings were applied under compression [10].
Surgical intervention for venous ulcers has also been used for many years. Deep venous insufficiency, as witnessed in the non-invasive venous exam ordered for our case study, may be addressed surgically. Masuda et al. ran a clinical series on 51 limbs with severe venous disease that were managed with deep vein valvuloplasty and observed good outcomes in primary non-thrombotic deep vein incompetence in 73% of the limbs [11]. Perrin undertook a clinical series involving 144 limbs demonstrating severe venous disease that were either managed by valvuloplasty (n = 85), transposition (n = 18), transplantation (n = 32), or Psathakis' technique II (n = 9). Duplex ultrasound showed that valvular competence was restored in 79% of limbs with valvuloplasty, 71% of limbs with valve transposition, and 48% of limbs with transplantation. Leg ulcers healed and remained healed for 75% of the limbs with primary valvular incompetence [12]. Despite the relative success of these procedures. this treatment remains in limited clinical use in specialized centers.
Complicating the patient's diagnosis of venous hypertension is his congenital Klippel-Trenaunay Weber Syndrome, which is described as a rare congenital medical condition in which blood vessels and/or lymph vessels fail to form properly. The triad of a port-wine stain or stains (nevus flemmeus), varicose veins and lymphatic malformations, and bony and soft tissue hypertrophy involving only one extremity characterize the syndrome [3]. The existence of refractory arterio venous malformations despite a known history of embolization as a child would have greatly complicated our patient's course and would have required additional embolization therapy. Despite the working conclusion that the ulcerations were mainly caused by venous hypertension, the ulcerations themselves did not present as a typical venous wound with weeping serous drainage, asymmetrical borders and yellow slough covering the base. Instead, the patient presented with an eschar, which was raised from the level of the skin and could be described visually as resembling "the outer shell of an oyster". The atypical presentation of the wound is difficult to explain and warrants the biopsy that was taken early on in the patient's care. The reason for the ulcerations odd appearance remains a mystery.
Perhaps the addition of soft tissue hypertrophy to venous hypertension or the fact that the wound was overlying a port wine stain could be part of the answer. Despite the wounds' characteristics, they responded well to a regimen centered on compression therapy and the patient was healed and pain free in 4 months.
The purpose of this report was to present an atypical lower extremity ulceration treated successfully with a full vascular work up and compression therapy. No other similar case reports are known to the authors and it is our hope that future practitioners may use this model as a possible starting point for a treatment protocol of their own for non-healing wounds associated with KIWS.
References
- Klippel M, Trenaunay P (1900)Nouvauxvariqueuxosteohyper- trophiques. ArchGen Med 185:641
- Weber FP (1907) Angioma-formation in connection with hypertrophy of limbs and hemi√?¬¨hypertrophy. British Journal of Dermatology 19: 231-235.
- James W, Berger T, Elston D (2005) Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.) Saunders. p: 585.
- Bliznak J, Staple TW (1974) Radiology of angiodysplasias of the limb. Radiology 110: 35-44.
- Baskerville PA, Ackroyd JS, Browse NL (1985) The etiology of the Klippel-Trenaunay syndrome. Ann Surg 202: 624-627.
- Servelle M (1985) Klippel and Tr√?¬©naunay's syndrome 768 operated cases. Ann Surg 201: 365-373.
- McGrory BJ, Amadio PC (1993) Klippel-Trenaunay syndrome: orthopaedic considerations. Orthop Rev 22: 41-50.
- Barker KT, Foulkes WD, Schwartz CE, Labadie C, Monsell F, et al. (2006) Is the E133K allele of VG5Q associated with Klippel-Trenaunay and other overgrowth syndromes? J Med Genet 43: 613-614.
- Partsch H, Flour M, Coleridge Smith P, International Comression Club (2008) Indications for compression therapy in venous and lymphatic disease consensus based on experimental data and scientific evidence. Under the auspices of the TUP. IntAngiol 27:193-219.
- Palfreyman SJ, Nelson EA, Lochiel R, Michaels JA (2006) Dressings for healing venous leg ulcers. Cochrane Database Syst Rev 19.
- Masuda EM, Kistner RL (1994) Long-term results of venous valve reconstruction: a four- to twenty-one-year follow-up. J VascSurg 19: 391-403.
- Perrin M (2000) Reconstructive surgery for deep venous reflux: a report on 144 cases. CardiovascSurg 8: 246-255.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13530
- [From(publication date):
July-2016 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 12590
- PDF downloads : 940