Nodular Hidradenoma Mimicking Breast Cancer: Diagnostic Conundrum
Received: 03-Mar-2018 / Accepted Date: 12-Mar-2018 / Published Date: 16-Mar-2018 DOI: 10.4172/2161-0681.1000341
Abstract
A nodular hidradenoma, clear cell hidradenoma or eccrine acrospiroma is an exceedingly rare entity in the breast tissue. It is a benign adnexal cell tumor derived from eccrine sweat gland.
To our knowledge approximately thirty cases are reported in English literature. The aim of this article is to raise the awareness of this tumor so that patients can receive appropriate diagnosis and therapy. Herein we report a case of 51-year-old female who underwent complete wide excision of left lateral breast mass. Two years ago the left lateral breast biopsy was diagnosed as an atypical papillary lesion. Essentially, this diagnosis was inconclusive and the breast mass resection followed and the final diagnosis was nodular hidradenoma.
Keywords: Nodular hidradenoma; Mimicker of breast cancer
Introduction
Core breast biopsy and fine needle aspiration are the accepted methods of initial assessment of breast masses. For common breast tumors these initial screening tests can be diagnostic. However, due to rarity and frank unfamiliarity of this entity this can prove to be challenging and sometimes lead to misdiagnosis. There are reports in literature of misdiagnosis of hidradenoma as a breast carcinoma both clinically as well as pathologically [1-5].
Case Presentation
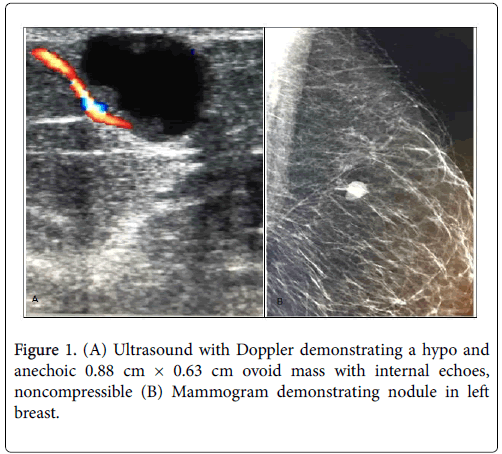
A 51 year old female with a two year history of painless lump in left breast measuring 2.3 cm in greatest dimension. Initially, an ultrasound was read as BIRADS IV (Figure 1). A core needle biopsy followed which was read as atypical papillary lesion. The diagnosis was interpreted as inconclusive; thus, a wide excision of the lump was performed and the diagnosis was rendered of a nodular hidradenoma. The specimen consisted of a pink-tan bilocular cystic lesion measuring 2.3 cm × 2.1 cm × 1.8 cm located immediately beneath the epidermis.
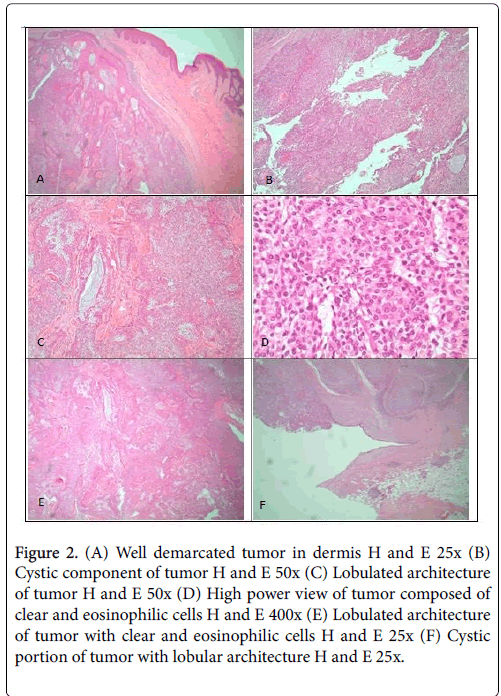
A minimal straw colored fluid was expressed from the mass. Microscopically, the mass had two components: cystic and solid. On low power view, the mass was conspicuously demarcated from the rest of breast parenchyma (Figure 2). In addition, the lesion on low power displayed prominent lobulated architecture. The tumor comprised of two cell types: clear cells and eosinophilic cells. The clear cells are smaller polyhedral cells with round nuclei and larger cells with clear cytoplasm and distinct cell membranes [3].
Figure 2: (A) Well demarcated tumor in dermis H and E 25x (B) Cystic component of tumor H and E 50x (C) Lobulated architecture of tumor H and E 50x (D) High power view of tumor composed of clear and eosinophilic cells H and E 400x (E) Lobulated architecture of tumor with clear and eosinophilic cells H and E 25x (F) Cystic portion of tumor with lobular architecture H and E 25x.
Furthermore, the cells can be characterized by the immunohistochemistry. Hidradenomas are known to be immunoreactive to EMA, CK and S-100 but known to be negative for ER, GCDFP-15 and SMA [1].
Discussion
A nodular hidradenoma is a benign adnexal tumor of eccrine sweat gland origin. Hidradenomas are commonly encountered on face, upper extremity, axilla, trunk, thigh, scalp and pubis [2]. Hidradenoma presenting in a breast is exceedingly rare and this can potentially lead to misdiagnosis. The aim of this paper is to convey awareness of this entity and its histological and cytological features in order to preclude misdiagnosis of breast malignancy. The nodular hidradenomas of breast have predilection for nipple and subareolar area but it can also occur deep in the breast tissue parenchyma. Although it is more common in females (75%), both genders are affected [1]. It has a proclivity to affect the left breast and the average age of patient is 50.3 ± 14.6 at presentation [1]. Usually the breast mass is around 2 cm and the commonest symptom is nipple discharge and/or painless lump. There is only 5% chance of nodular hidradenoma transforming to a malignancy.
Macroscopically, the tumor presents as a well demarcated nodule partially cystic or solid. It is composed of two cell types. The smaller cells are the eosinophilic darker (paroid) and the larger ones are clear (cuticular) ones with conspicuous cell membranes [1]. In addition, an occasional tubular structure was noted with luminal eosinophilic contents. The immunohistochemical profile of hidradenoma is positive for the following antibodies EMA, CK and S-100 but negative for ER, GCDFP-15 and SMA.
Fine needle aspiration can be particularly challenging and be a potential diagnostic pitfall for misdiagnosing hidradenomas as breast carcinomas. Cytologically, the hidradenoma presents as a cellular aspirate. The cells are arranged in prominent cohesive sheets with or without papillae with scattered rare singular cells. The cells are polyhedral with abundant to moderate eosinophilic granular to clear cytoplasm [6]. The nuclei are round to oval with smooth contours and conspicuous nucleoli. The background usually possesses a modicum degree of hemorrhage.
There are some overlapping features between hidradenomas and breast carcinomas which can lead the pathologist astray to a misdiagnosis. Both of these entities present as cellular aspirates and both harbor to some degree scattered individual cells. The cohesive clusters are the hallmark of hidradenomas, not of breast carcinomas. Scattered individual cells and discohesion predominate in the breast carcinoma milieu. Necrosis and mitotic activity can be appreciated in breast malignancies but are not apparent in adnexal tumors. In addition, the nuclear atypia tends to be more pronounced in carcinomas. Hidradenomas can harbor vesicular nuclei with coarse chromatin and conspicuous nucleoli [4].
In conclusion, adnexal tumors should be entertained in the differential diagnosis when a breast lump is detected in both genders especially in the nipple/subareolar region. It is imperative to be cognizant of both cytological and histological features of nodular hidradenomas so that misdiagnosis of breast cancer does not occur. A correct diagnosis is essential since it leads to an appropriate treatment plan for the patient.
Conflict of Interest
The authors declare that there is no conflict regarding the publication of this paper. Supported by the Lake Erie College of Osteopathic Medicine (LECOM) and the Lake Erie Consortium for Osteopathic Medical Training (LECOMT).
References
- Domoto H, Terahata S, Soto K, Tamai S (1998) Nodular hidradenoma of the breast: Report of two cases with literature review. Pathol Int 48: 907-911.
- Mote DG, Ramamurti T, Naveen Babu B (2009) Nodular hidradenoma of the breast: case report with literature review. Ind J Surg 71: 43-45.
- Ilie B (1986) Neoplasms in Skin and Subcutis Over the Breast, Stimulating Breast Neoplasms:Case Reports and Literature Review. J Surg Oncol 31: 191-198.
- Kumar N, Verma K (1996) Clear cell hidradenoma: a diagnostic pitfall in fine-needle aspiration of breast. Diagn Cytopathol 15: 70-72.
- Ives CL, Donnelly PK, Ryley N, Green R, Bliss P Eliss I (2013) Nenign Hidradenoma Masquerading as Ductal Breast Cancer-A Rare Case of False Positive Recurrence in Cancer Follow-up. Breast J 19: 670-671.
- Grampurohit VU, Dinesh US, Rao R (2011) Nodular hidradenoma of male breast: cytohistological correlation. J Cytol 28: 235-237.
Citation: Tynski Z, Barrett AJ, Chiang W (2018) Nodular Hidradenoma Mimicking Breast Cancer: Diagnostic Conundrum. J Clin Exp Pathol 8: 341. DOI: 10.4172/2161-0681.1000341
Copyright: © 2018 Tynski Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5639
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 4834
- PDF downloads: 805