Case Report Open Access
New-Onset Focal Nodular Hyperplasia in a Patient with Viral Hepatitis: A Case Report
Zhang Y1, Ding H1,2*, Peng SY1, Ji Y3 and Wang WP11Department of Ultrasound, Zhongshan Hospital, Shanghai Institute of Medical Imaging, Fudan University, Shanghai 200032, China
2Department of Ultrasound, Qingpu Branch of Zhongshan Hospital, Fudan University, Shanghai 201700, China
3Department of Pathology, Zhongshan Hospital, Fudan University, Shanghai 200032, China
- Corresponding Author:
- Hong Ding
Department of Ultrasound, Zhongshan Hospital,
Shanghai Institute of Medical Imaging,
Fudan University, 180 Fenglin Road, Shanghai 200032, China
Tel: +86-136-5188-6013
E-mail: ding.hong@zs-hospital.sh.cn
Received Date: October 24, 2016; Accepted Date: November 15, 2016; Published Date: November 18, 2016
Citation: Zhang Y, Ding H, Peng SY, Ji Y, Wang WP (2016) New-Onset Focal Nodular Hyperplasia in a Patient with Viral Hepatitis: A Case Report. OMICS J Radiol 5:239. doi: 10.4172/2167-7964.1000239
Copyright: © 2016 Zhang Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Background: New-onset hepatic nodules mostly are hepatocellular carcinomas in patients with viral hepatitis. Focal Nodular Hyperplasia (FNH) is the second most common benign liver tumor, which usually does not recur after surgical resection. We present a case of hepatitis B virus infected female with a new-onset FNH during pregnancy, which has not been reported before, to not only put an emphasis on the diagnostic accuracy of FNH but also avoid unnecessary surgical intervention. Case presentation: The 28-year-old Chinese female with chronic hepatitis B virus infection who underwent a resection of FNH in the left lobe of the liver three years ago, was found to present with a new-onset solid lesion in the right lobe of the liver. Contrast-Enhanced Ultrasound (CEUS) demonstrated a typical FNH of spoke wheel pattern enhancement in the arterial phase, still enhanced during the portal venous and delayed phases with a central stellate scar, which showed a similar enhancement pattern on contrast-enhanced CT and MRI. Finally, a core needle biopsy of the suspected lesion was confirmed to be FNH. Conclusion: Regenerate of FNH may also occur in patients with chronic hepatitis B, which was known as a risk factor for the occurrence of hepatocellular carcinoma. Diagnosis of FNH can be made definitely and non-invasively through the appliance of modern imaging modalities with typical performance of imaging features.
Keywords
Focal Nodular Hyperplasia (FNH); Recurrence; Diagnosis; Hepatitis; Case report
Abbreviations
FNH: Focal Nodular Hyperplasia; MRI: Magnetic Resonance Imaging; CT: Computed Tomography; AFP: Alpha-Fetoprotein; CA19-9: Carbohydrate Antigen 19-9; CEA: Carcinoembryonic Antigen; CEUS: Contrast-Enhanced Ultrasound; GS: Glutamine Synthetase
Introduction
New-onset hepatic nodules mostly are hepatocellular carcinomas or dysplastic or regenerative nodules in patients with viral hepatitis B. Focal nodular hyperplasia (FNH) is the second most common benign liver tumor [1], which usually won’t get a recurrence after surgical resection. Differential diagnosis of new-onset hepatic nodules based on imaging features remains the great concern for physicians. To our knowledge, no cases of new-onset FNH in patients with hepatitis B virus have been reported, therefore we present a case of hepatitis B virus infected female with a new-onset FNH during pregnancy, so as to not only raise clinicians' attention of the importance in the diagnosis of FNH through the appliance of modern imaging modalities even in the patients with viral hepatitis but also avoid unnecessary surgical intervention.
Case Report
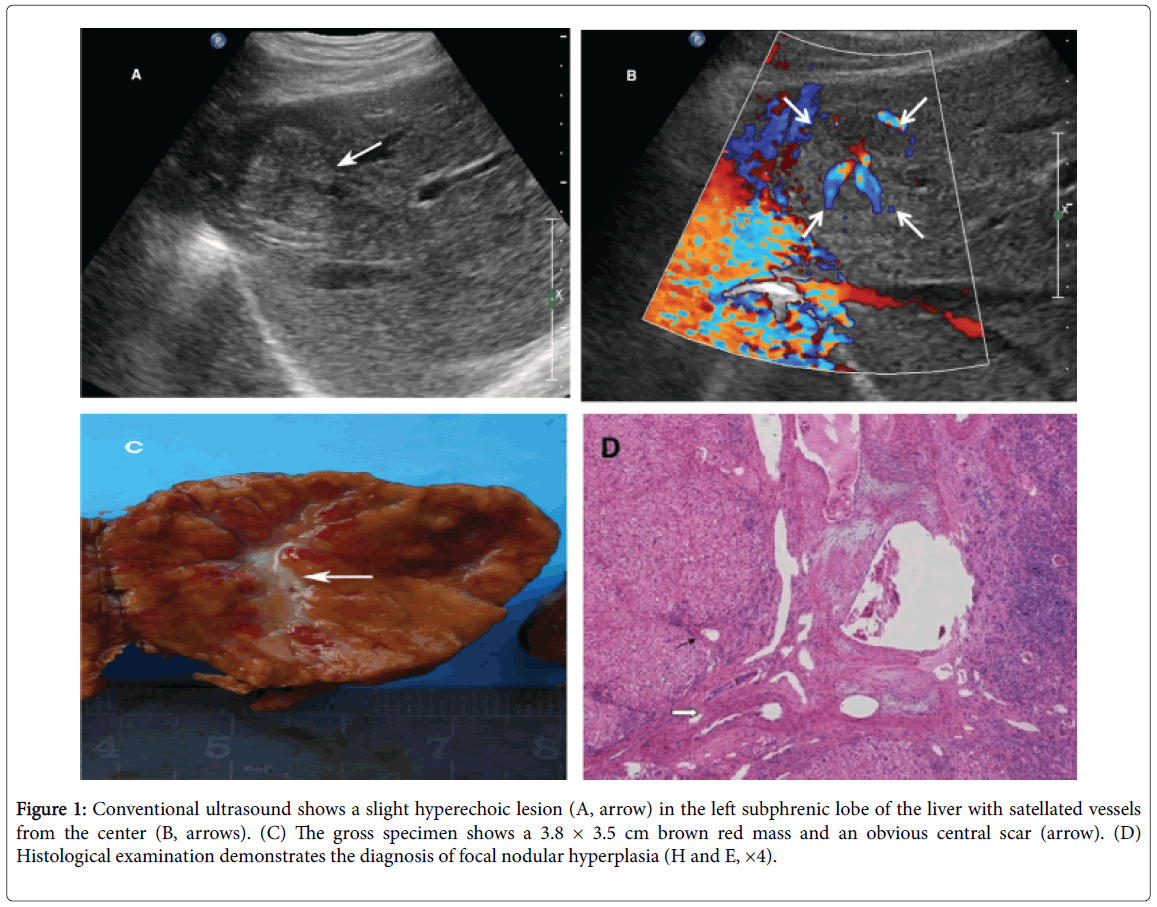
A 25-year-old Chinese female presented with a solid nodule in the left lobe of her liver near the diaphragmatic dome in 2012. The laboratory tests: Hepatitis B surface antigen (HBsAg) (-), hepatitis B surface antibody (HBsAb) (>1000, +), hepatitis B e antigen (HBeAg) (-), hepatitis B e antibody (HBeAb) (+), hepatitis B core antibody (HBcAb) (+), hepatitis B virus DNA (-). The lesion was heterogeneous and slight hyperechoic with a size of 38 × 35 mm on conventional ultrasound. The shape of the tumor was irregular and there seemed to be a low echo dark ring around the lesion. Color Doppler Ultrasound showed abundant intratumoral flow signals with a spoke-wheel pattern in the center of the lesion. The resistance index of the detected arteries was approximately 0.60. Although asymptomatic, that lesion was completely resected. The surgical removal of the lesion showed the gross specimen a 3.8 × 3.5 cm brown red mass and an obvious central scar (Figure 1). Final histopathological examination indicated features consistent with FNH.
Figure 1: Conventional ultrasound shows a slight hyperechoic lesion (A, arrow) in the left subphrenic lobe of the liver with satellated vessels from the center (B, arrows). (C) The gross specimen shows a 3.8 × 3.5 cm brown red mass and an obvious central scar (arrow). (D) Histological examination demonstrates the diagnosis of focal nodular hyperplasia (H and E, ×4).
In 2015, routine ultrasound examination indicated nothing abnormal in her liver for three years before the patient got pregnant. At 28 weeks gestation, routine gynecological ultrasound in local hospital revealed a solid focal lesion in the right lobe of the liver with a size of 26 × 23 mm. Subsequent Magnetic Resonance Imaging (MRI) demonstrated the hepatic nodule being suspicious of malignancy. Abdominal examination was notable for a gravid uterus consistent with a third trimester of pregnancy but wasn't palpable for the liver.
The laboratory tests: Alpha-fetoprotein (AFP) 137 ng/mL (abnormal, >20 ng/mL), Carbohydrate antigen 19-9 (CA19-9) and Carcinoembryonic Antigen (CEA) were within normal limits. Viral serological tests for hepatitis B were positive. She was arranged for an induction of labor at 34 weeks’ gestation and delivered a healthy baby at term via normal vaginal delivery.
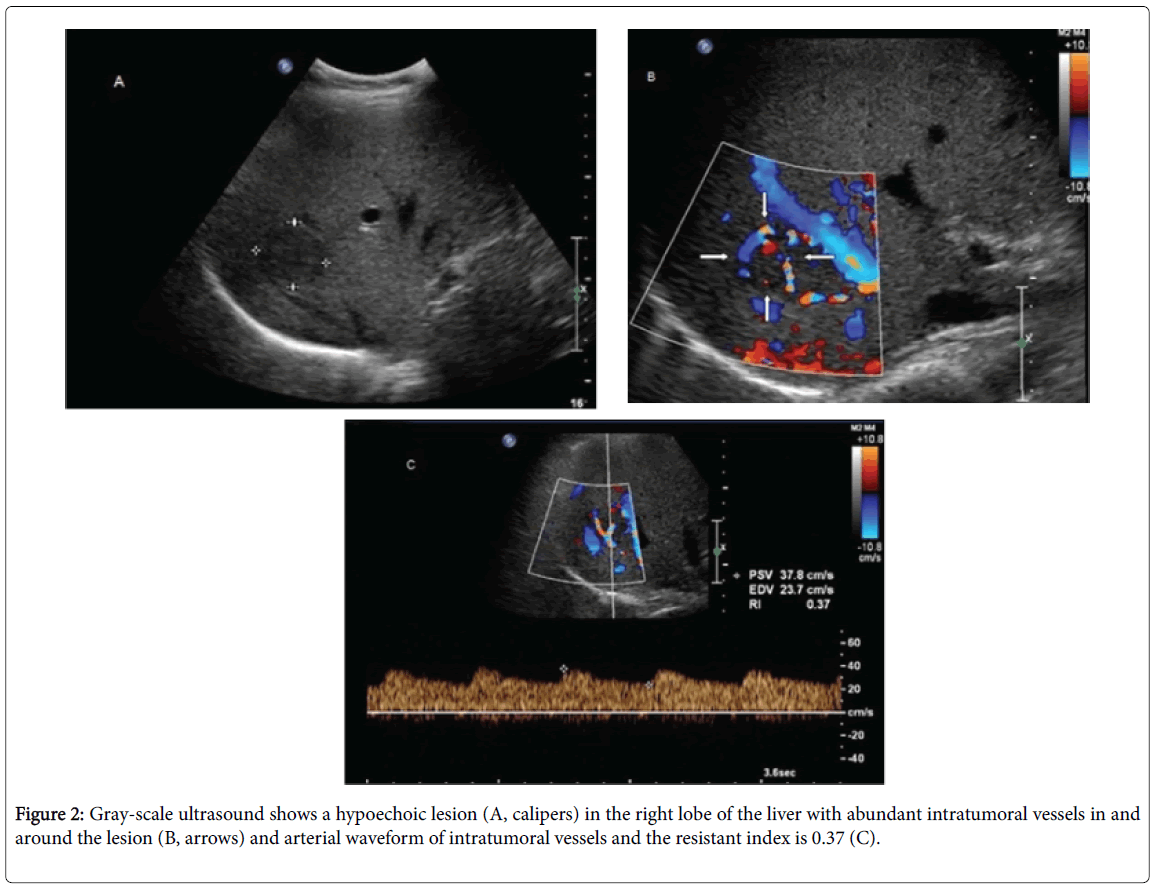
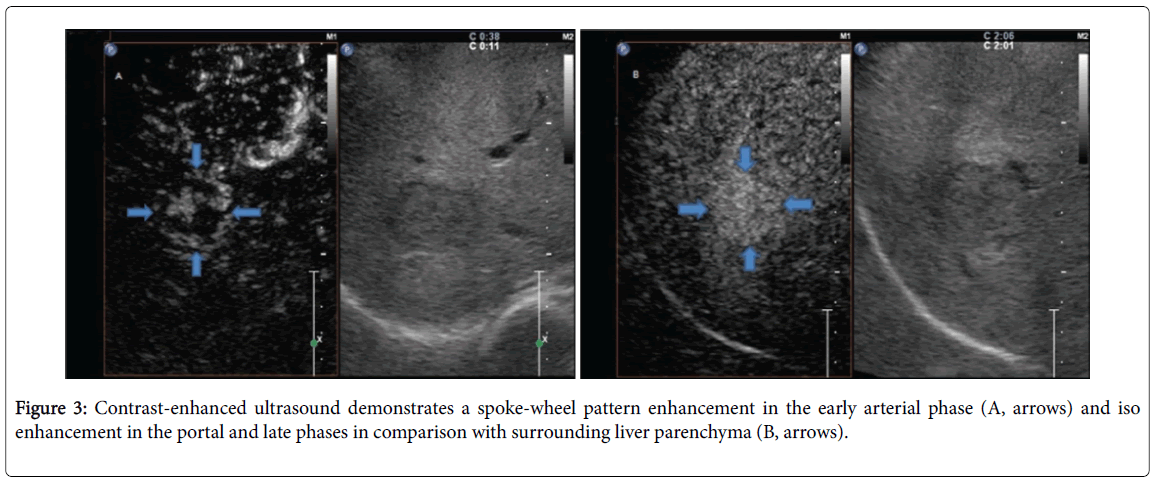
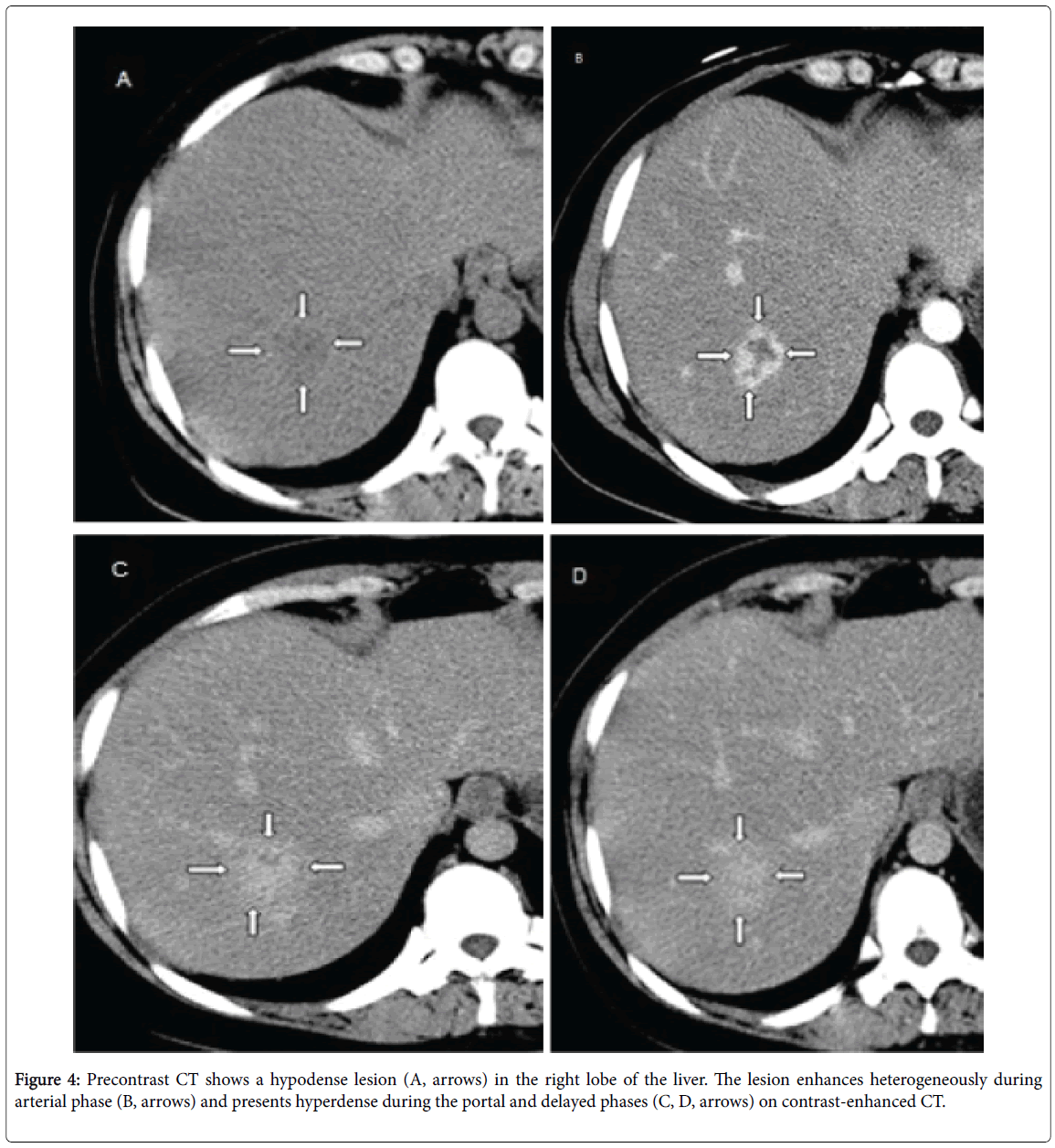
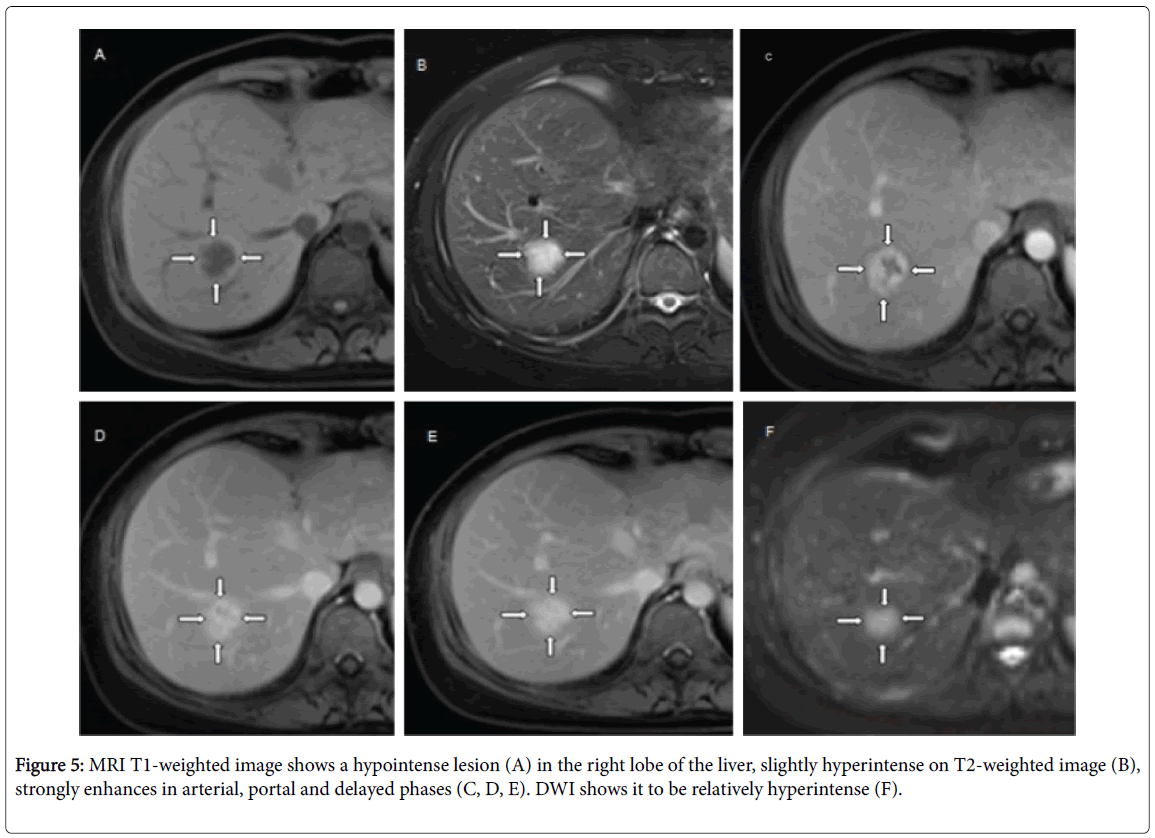
Then she was referred to our hospital for further management. Physical examination showed nothing abnormal of her liver. Imaging studies with and without contrast agent, including abdominal ultrasound, Computed Tomography (CT), and MRI were performed. Gray-scale ultrasound showed a hypoechoic well-defined lesion in the right lobe of the liver and the size of the lesion increased to 35 × 30 mm. Color Doppler Ultrasound disclosed abundant peri-and intratumoral vessels, whose resistance index was approximately 0.37 (Figure 2). Contrast-Enhanced Ultrasound (CEUS) with SonoVue® (BR1; Bracco, Milan, Italy) showed a centrifugal filling preceded by a spoke-wheel pattern enhancement in the early arterial phase and it appeared hyperechoic in comparison with the surrounding liver parenchyma during the portal venous and delayed phases (Figure 3). On precontrast CT scans, the lesion was seen as a focal hypodense nodule, which enhanced rapidly during arterial phase and still enhanced during portal phase. A relatively hypodense central scar was observed during arterial phase with delayed enhancement during later phases (Figure 4). On MRI scans, this lesion was slightly hypointense on T1-weighted images, hyperintense on T2-weighted images and had a similar enhancement pattern after injection of gadolinium (Figure 5). Laboratory data revealed both normal liver biochemistries and normal hepatic synthetic function. AFP level was 30.51 ng/mL, a little exceeding normal limit (20 ng/mL).
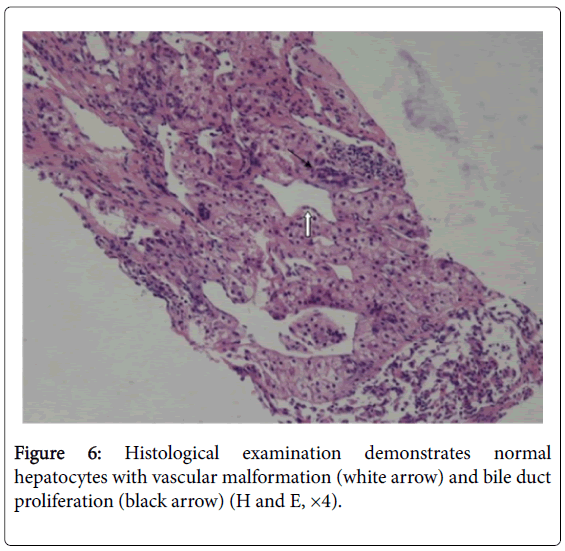
The imaging findings of CEUS, CT and MRI confirmed the diagnosis of FNH. To exclude the smaller possibility of malignancy, however, a core needle biopsy of the lesion was performed under the guidance of ultrasound. Microscopically, we observed a proliferation of hepatocytes, bile ducts, lymph-vessels and blood vessels. The hepatocytes were cytologically normal. Enzyme Marked Assays authenticated it further. Eventually a final diagnosis of FNH was confirmed (Figure 6).
The patient was discharged without complications on post-operative day 7. She was doing well during four years of follow-up in ultrasound and MRI.
Discussion
FNH is the second most common benign liver tumor after hemangioma. It is found in all ages of groups in both males and females, however, more frequent in females, especially among reproductive age young women. FNH is a nodule composed of normal hepatocytes occurring in a liver otherwise histologically normal [2]. Its pathogenesis remains unknown although the most accepted theory suggests that it is a result of congenital or acquired vascular abnormalities, responding to hyperperfusion by the characteristic anomalous arteries found in the center of the nodules [3]. In typical case, a central stellate scar can be found in it, which is seen as a relatively characteristic imaging finding in FNH. The central scar contains malformed vascular structures and fibrous connective tissue [4]. FNH is usually asymptomatic which is largely responsible for the difficulty in diagnosis, nevertheless, in reported symptomatic cases the symptoms are largely variable-abdominal pain the most frequent. Khan et al. [5], reported an unusual case with a progressively increasing mass in the right upper quadrant which was associated with pain and emesis. Trucut biopsy of the hepatic mass was equivocal and angiography showed a tumor vascular that was supplied by a tortuous branch of the proper hepatic artery. However, the final histopathological examination ascertained it to be FNH.
Navarro et al. [1], believed that there are two key issues influencing clinical decision making (conservative observation versus surgical resection) of FNH: Diagnostic certainty and symptomatic assessment. The indications for surgical management of suspected FNH has not been amply and explicitly clarified until now. Nowadays, most publications are in favor of the conservative management by for FNH when the diagnosis is certain in imaging or after biopsy. Routine physical examination is suggested to keep the suspected lesion under surveillance. Diagnosis remains the subject of concern for FNH management.
With increasing use of modern imaging modalities, FNH is becoming clinically more relevant [6]. Diagnostic modalities used in the majority of FNH studies involve ultrasound, CT and MRI, among which MRI has the highest sensitivity and specificity in the diagnosis of FNH. Typical imaging features could help radiologists to diagnose FNH more confidently.
On ultrasound, FNH appears as variable degrees of echogenicity, usually slightly hypoechoic or isoechoic, with lobulated contours or a hypoechoic halo. Although a characteristic finding is the slightly hyperechoic central stellate scar, it is often difficult to visualize on grayscale ultrasound. However, it has earned widespread acceptance that CEUS is highly specific for the diagnosis of FNH and the combination of color Doppler ultrasound with CEUS can increase the diagnostic rate of FNH. The typical CEUS features of FNH contain centrifugal or global filling with sustained enhancement [7]. On precontrast CT scans, FNH is seen as a focal hypodense or isodense mass. A central hypodense scar can be observed in only one-third of cases. In most cases (89-100%), the lesion enhances rapidly during the arterial phase on contrast-enhanced CT and its parenchymal enhancement is sustained in the portal venous and delayed phases. Patients who had undergone MRI had typical findings including slightly hyperintense on T2-weighted images, slightly hypointense on T1-weighted images, a hyperintense central scar on T2-weighted images and arterial enhancement without delayed washout. Current studies consistently show that MRI using hepatobiliary-specificity contrast agents such as gadoxetic acid (Gd-EOB-DTPA) allows for higher diagnostic accuracy of FNH, due to the mechanism that uptake of Gd-EOB-DTPA is only achieved by functional hepatocytes and FNH is considered as a nonneoplastic lesion [8]. In general, typical imaging features could help radiologists to diagnose FNH more confidently. In our case, in spite of the typical findings of the central scar on CT and MRI, the pathological findings from liver biopsy (cytologically normal hepatocytes) also supported the final diagnosis of FNH, in addition to not only reach a more accurate diagnostic rate but also avoid unnecessary surgical intervention.
However, imaging cannot firmly establish the diagnosis of FNH sometimes, for the typical signs maybe absent or weak in atypical cases. A special immunostaining of Glutamine Synthetase (GS) has attracted attention in recent years. Some studies have confirmed that GS can help identify FNH from other hepatocellular nodules [9,10]. The wild clinical application of the immunohistochemistry method to determine the certainty of diagnosis of FNH also needs further validation and development.
The potential malignancy of FNH remains indeterminate, but there have been no reports of definitely histologically proven malignant transformation of FNH into hepatocellular carcinoma (HCC). In spite of that, association between FNH and HCC do exist. Petsas et al. [11], reported a case of HCC arising within a large FNH. The lesion underwent preoperative CT-guided core needle biopsy that revealed FNH but the final histological diagnosis resulted FNH and HCC. This suggests that: patients should be made fully aware of the potential for malignancy in addition to a benign diagnosis more likely; repeat imaging examination should be adopted to observe the change of suspected lesions.
Based on the current research, the case we presented above-FNH occurred in patients with HBV infection-is likely to be fortuitous. However, it has been wildly recognized that the chronic HBV infection is the most significant etiologic risk factor of HCC. Therefore, like our case, typical imaging findings put a more important role on diagnostic certainty in those occasional but crucial cases, so as to avoid unnecessary surgeries.
Although the influence of pregnancy on the occurrence and enlargement of FNH remains controversial, the latest studies tend to consider that FNH may be responsive to female hormones such as estrogen or progesterone. Enlargement of FNH during pregnancy have been reported [12,13]. Furthermore, one recent study demonstrated that the majority of FNH lesions and surrounding liver parenchyma express estrogen receptors [14]. In our case, we speculate that there might be a vascular abnormality in the right lobe of the liver and the new-onset nodule was growing up around that abnormal vascularity. However, it wasn’t big enough to be found by imaging before until her pregnancy when her inner estrogen stimulated its growth further more. Another point to be noted is that the AFP-serum tumor markers are abnormal (137 ng/mL) in this patient. This can also be one contributing factor to a wrong judgement to malignant. While AFP is not only an oncoembryonal protein which is highly expressed in hepatocellular carcinomas, it also can be elevated physiologically in pregnant women, for the reason that AFP is fetal glycoprotein which is derived from fetal liver cells. This also should be paid attention in clinical diagnosis.
Conclusion
Diagnosis accuracy remains the subject of the concern for FNH detection and management. Regenerate of FNH may also occur in viral hepatitis infected patients, which deserves our attention in terms of diagnosis and differential diagnosis. A series of typical imagistic features found through modern imaging modalities can not only significantly increases the diagnostic accuracy of FNH but also avoid unnecessary surgical intervention.
Conflicts of Interest Disclosure
There are no conflicts of interest among the authors or with other people/organizations.
Acknowledgement
This work was supported by National Natural Science Foundation of China (No. 81571675).
References
- Navarro AP, Gomez D, Lamb CM, Brooks A, Cameron IC (2014) Focal nodular hyperplasia: a review of current indications for and outcomes of hepatic resection. HPB 16: 503-511.
- Lecler A, Arrive L (2011) Focal nodular hyperplasia. Clin Res Hepatol Gastroenterol 35: 159-160.
- Byrnes V, Cardenas A, Afdhal N, Hanto D (2004) Symptomatic focal nodular hyperplasia during pregnancy: a case report. Ann Hepatol 3: 35-37.
- Chen WH, Peng CM, Chou CM, Chen HC, Jan YJ (2010) Focal nodular hyperplasia of the liver in a 5-year-old girl. J Chin Med Assoc 73: 611-614.
- Khan MR, Saleem T, Haq TU, Aftab K (2011) Atypical focal nodular hyperplasia of the liver. Hepatobiliary Pancreat Dis Int 10: 104-106.
- Wasif N, Sasu S, Conway WC, Bilchik A (2008) Focal nodular hyperplasia: report of an unusual case and review of the literature. Am Surg 74: 1100-1103.
- Kong WT, Wang WP, Huang BJ, Ding H, Mao F, Si Q (2015) Contrast-enhanced ultrasound in combination with color doppler ultrasound can improve the diagnostic performance of focal nodular hyperplasia and hepatocellular adenoma. Ultrasound Med Biol 41: 944-951.
- Palmucci S (2014) Focal liver lesions detection and characterization: the advantages of gadoxetic acid-enhanced liver MRI. World J Hepatol 6: 477-485.
- Bioulac-Sage P, Laumonier H, Rullier A, Cubel G, Laurent C, et al. (2009) Over-expression of glutamine synthetase in focal nodular hyperplasia: a novel easy diagnostic tool in surgical pathology. Liver Int 29:459-465.
- Bioulac-Sage P, Cubel G, Taouji S, Scoazec JY, Leteurtre E, et al. (2012) Immunohistochemical markers on needle biopsies are helpful for the diagnosis of focal nodular hyperplasia and hepatocellular adenoma subtypes. Am J Surg Pathol 36: 1691-1699.
- Petsas T, Tsamandas A, Tsota I, Karavias D, Karatza C, et al. (2006) A case of hepatocellular carcinoma arising within large focal nodular hyperplasia with review of the literature. World J Gastroenterol 12: 6567-6571.
- Shortell CK, Schwartz SI (1991) Hepatic adenoma and focal nodular hyperplasia. Surg Gynecol Obstet 173: 426-431.
- Kim MJ, Han SY, Baek YH, Lee SW, Kwon HJ (2014) A case of focal nodular hyperplasia with growth progression during pregnancy. Clin Mol Hepatol 20: 392-397.
- Chandrasegaram MD, Shah A, Chen JW, Ruszkiewicz A, Astill DS, et al. (2015) Oestrogen hormone receptors in focal nodular hyperplasia. HPB 17: 502-507.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 14440
- [From(publication date):
December-2016 - Mar 30, 2025] - Breakdown by view type
- HTML page views : 13441
- PDF downloads : 999