Newborn and Maternal Outcomes in Out-of-Hospital Delivery: A Review
Received: 19-Mar-2018 / Accepted Date: 23-Apr-2018 / Published Date: 30-Apr-2018 DOI: 10.4172/2376-127X.1000371
Abstract
Introduction: As maternity services became available out-of-hospital births diminished in favor of planned hospital deliveries. After an early decline, there is a recent increase of out-of-hospital births in United States, from 0.87% in 2004 to 1.36% in 2012. Reasons why women have an out-of-hospital birth differ between countries. Many women feel that hospital is the safest place to give birth, but others believe that hospital is impersonal and a place that provoke anxiety. Maternal outcomes due to labor include: Obstetric interventions’ and non-related with interventions. Newborn outcomes comprise: 5 min Apgar <7, prematurity, low birth-weight (<10% for gestational age or <2500 g), macrosomia (>90% for gestational age or ≥ 4000 g), postdatism (≥ 42 weeks’ gestation), assisted ventilation requirement and neonatal/perinatal death. The aim of this review was to understand the real impact of out-of-hospital births in newborn and maternal outcomes. Methods: The search was performed on PubMed, from which 45 articles met all inclusion criteria. Results: In developed countries, home birth rate is very low (1-2% in UK, 1% in New Zealand, 0.6% in USA, 0.5% in France and 0.4% in Australia), the exception is Netherland (30%). In developing countries, the situation is quite different: Home birth rate is 95% in Bangladesh, 41% in Mozambique and 90% in Nepal. Unplanned out-of-hospital births had higher incidence of maternal and newborn complications. Planned out-of-hospital deliveries also showed higher incidence of newborn complications, especially when transferred babies were considered also out-of-hospital births. Discussion: Although some studies showed that maternal-fetal outcomes occur in the same proportion in planned low risk out-of-hospital births compared to hospital births, unplanned or high-risk out-of-hospital births show higher incidence of maternal and newborn complications. Conclusion: The safety of out-of-hospital births remains controversial because the benefits may be overcome by the disadvantages, given the maternal and birth risk and the unplanned scenarios.
Keywords: Out of hospital birth; Out of hospital delivery; Home birth; Out of hospital birth outcomes; Out of hospital delivery outcomes; Water birth
Introduction
Labor is a unique experience in which women are confronted with great dualities of feelings, some apprehensions, fears, but also with happiness [1].
There are many options available that the mother can choose for deliver her baby. One of which is an out-of-hospital birth, which is a birth that happens outside a hospital. This includes births occurring at home, birthing center (a freestanding place not attached to a hospital), doctor’s office or clinic or other location [2].
In 1900, almost all United States’ deliveries occurred outside a hospital. Though, as maternity care services became available, the frequency of out-of-hospital births in developed countries diminished in favor of planned hospital deliveries to 44% by 1940 and to 1% by 1969. However, after a gradual decline, the percentage of out-ofhospital births increased from 0.87% in 2004 to 1.36% in 2012 [2,3]. The American College of Obstetricians and Gynecologists estimates that, nowadays, 35000 births per year (0.9%) occur at home in United States of America (USA) [4]. Although home births have increased in the USA in the last decade, in Netherlands, the country with greatest experience in home births, they have decreased [5]. In undeveloped countries, unfortunately, the rates and outcomes of these out-ofhospital births are grossly underreported [6].
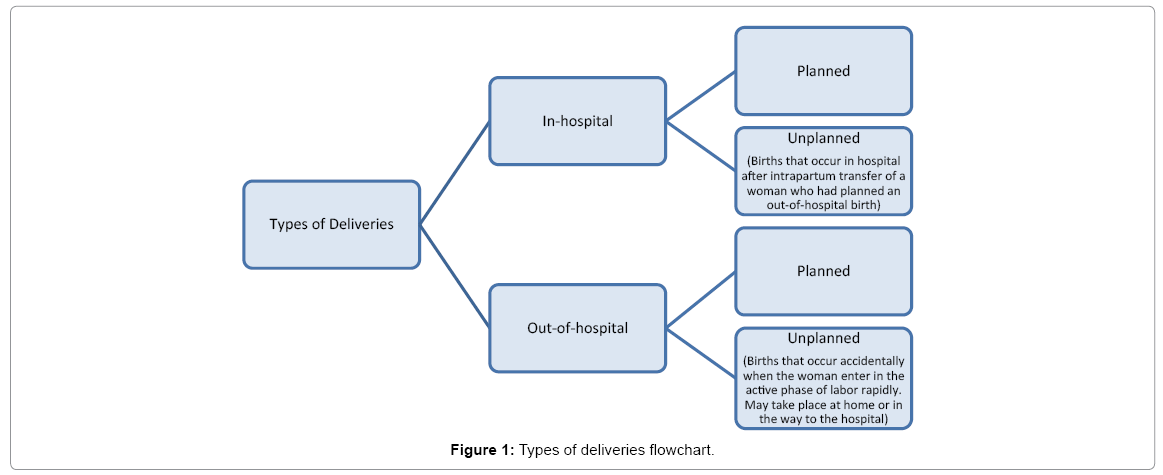
Out-of-hospital delivery can be divided into planned and unplanned. The first one are intended and planned to take place out-ofhospital and generally occur in a prepared setting with or without the attendance of medical staff, the second one usually occur accidentally when the woman enter in the active phase of labor rapidly and may take place at home or in the way to the hospital [6].
Furthermore, it is also important to disaggregate in-hospital births into the categories of planned in-hospital and unplanned (births that occur in hospital after intrapartum transfer of a woman who had planned an out-of-hospital birth) [7]. Actually, in the Centers for Disease Control and Prevention (CDC) dataset, when patient’s care began out-of-hospital but they were transferred to the hospital, their outcomes count as care in the hospital, which results on the underestimation of out-of-hospital outcomes [5]. Figure 1 summarizes these types of births (Figure 1).
It is imperative to know the location of delivery because it is related to important poor neonatal and maternal outcomes, like quality of intrapartum fetal monitoring, expertise of maternity care provider and access to acute care services [8]. In fact, over the past two decades there was a decrease in neonatal and perinatal deaths because of the use of ultrasound, electronic fetal heart rate monitoring, fetal acidbase assessment and labor induction [6,9]. As planned home births are related with lower interventions, some clinical signs of, for example, blood loss, such as decrease in blood pressure and increased heart rate, that tend to appear late are not possible to be detected because women are not well monitored [6,9].
In addition, it is also important to note whether or not the place of birth was planned because unplanned out-of-hospital deliveries carry a larger risk of adverse maternal, neonatal and perinatal outcomes, specifically maternal hemorrhage and neonatal and perinatal mortality [6].
Despite some studies have demonstrated that planned home birth is safe, mainly in countries where most of deliveries are attended by certified nurse-midwives, other studies revealed worse neonatal outcomes in planned home births, such as seizures or neurologic dysfunctions, an increased risk of 5 min Apgar score less than 7 and hypoxic ischemic encephalopathy [5,8,10-12].
The reasons why women have an out-of-hospital birth are totally different between countries. In some developed countries, women choose this kind of birth because they feel more safe and comfortable at home, want family involved, are afraid of hospitals or many other reasons [13]. The condition is quite different in developing countries, where out-of-hospital delivery is not exactly an option but occurs mainly due to limited access to health services and births with unskilled attendants are common, which are associated with high rates of neonatal mortality and morbidity [6].
Besides typical out-of-hospital deliveries, as the delivery process has many physiological challenges, science has improved to find different delivery methods with minimal medical intervention and minor negative results for mother and baby [14]. Among alternatives, water birth is, nowadays, a birth choice that some mothers prefer because they feel that it is a more natural process, similar to the environment in the uterus [15]. Although water birth has become a popular method, it remains controversial because of neonatal risk of aspiration, hypoxemia and infection [16].
Faced with controversial facts, the aim of this literature review is to understand the real impact of out-of-hospital births in newborn and maternal outcomes.
Methods
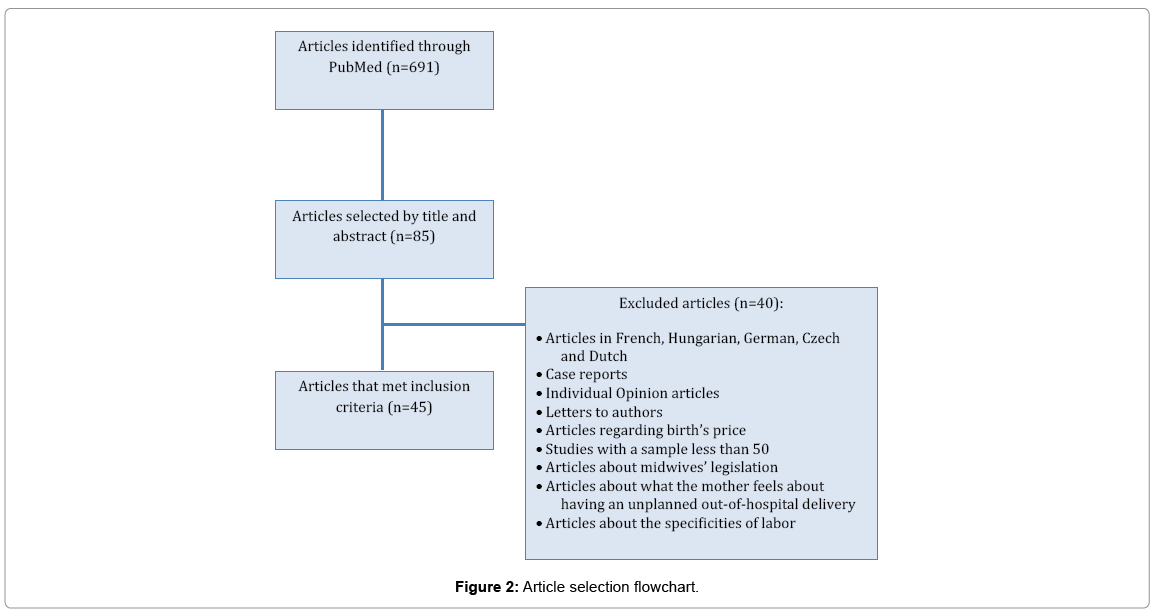
A search was performed on PubMed during the months of September, October and November of 2017, using the following formula of words: “out of hospital birth”, “out of hospital delivery”, “home birth”, “home birth outcome”, “out of hospital birth outcomes”, “out of hospital delivery outcomes” and “water Birth”. The filters “human” and “publication date from 31/08/2007 to 31/08/2017” were used.
Inclusion criteria included studies and review articles about outof- hospital deliveries, planned or not, about their outcomes and about what influences mother to want this type of delivery, written in English, Portuguese and Spanish. Were excluded articles in other languages, case reports, individual opinion articles, letters to authors, articles regarding the birth’s price, studies with a sample less than 50, articles about midwives’ legislation, about what the mother feels about having an unplanned out-of-hospital delivery and about the specificities of labor.
A total of 85 articles were selected by title and abstract, from which 45 articles met all inclusion criteria. Figure 2 represents the article selection flowchart. Based on the selected articles, the relevant information was collected for the review (Figure 2).
Results
Global rates of out-of-hospital deliveries
Developed countries: In most developed countries, home birth rate is very low (1-2% in UK, 1% in New Zealand, 0.6% in USA, 0.5% in France, 0.4% in Australia and 1.1% in Japan), the big exception is Netherlands that has 30% of home births [13,17-19].
Netherlands: Kooy et al. [20] found that, of women who deliver at home, 50% give birth attended by midwives [20].
As Netherlands’ home birth rate is the largest in Europe, perinatal mortality rate is also higher compared to other European countries, one of the causes may be the average age of mothers, that is the third highest in Europe (after Ireland and Spain), but more research is needed to understand the causes of this perinatal mortality [10].
USA: Pan American Health Organization estimates that 79% of deliveries in the region of the America take place in institutional settings [6]. Unfortunately, this trend was not accompanied by a corresponding decrease in maternal and perinatal mortality, which may be due to unnecessary interventions, such as cesarean section and episiotomy, which may lead to increased morbidity and even mortality [6].
If we consider out-of-hospital births in USA, in 2012, 66% occurred at home and 29% in a freestanding birthing center [2]. Despite the low rate of out-of-hospital deliveries in USA, the percentage has increased from 2004-2012 for all racial and ethnic groups, more for non-Hispanic white women [2].
Turkey: In some developed countries, like Turkey, there are no conditions for all births to take place in hospital, because population do not have a good access to medical services and only 83% of births are assisted by a doctor, nurse or midwife, the others occur without assistance or just assisted by neighbors [13].
Developing countries: In developing countries we can see a different context. In a multi-country analysis survey for developing countries, more than half of the deliveries were reported to be at home in 23 of 48 countries [21]. Home birth rate is around 95% in Bangladesh, 41% in Mozambique, 90% in Nepal, 43% in Ghana, 90% in Ethiopia and 62% in Nigeria [13,21].
Evidence has shown that 40% of all pregnancies will have complications and those, 15% are life threatening that require emergency obstetric care [21]. Therefore, a skilled attendant available at birth is crucial to recognize these complications, manage them and provide appropriate referral, in order to protect the mother from life threatening complications (like post-partum hemorrhage) and the newborn, that may need immediate resuscitation [21,22]. However, unfortunately, in all these countries, births with unskilled attendants are common (65% of all deliveries in 2005), because the majority of home deliveries are accidental or unprepared, which are associated with high rates of neonatal mortality and morbidity [6,22].
In fact, in Ethiopia, for example, over 90% of births take place at home in the presence of unskilled attendants and in Nepal, 55% of the deliveries that occur at home, are conducted by untrained friends or relatives [6,22]. This fact implies that neonatal morbimortality continue to be a large component of the burden of disease in sub-Saharan Africa, which constitutes a continuing obstacle to socio-economic development [23].
So, although infant mortality has fallen during the past 20 years, it is not enough, since the fall is being very slow and still significantly higher than in the hospital births [23]. Besides that, it is important to know that 56% of the global maternal deaths occurred in Sub-Saharan African (Nigeria alone accounted for 14% of these deaths) [21]. Nigeria also contributes to 60% to 70% of all childhood mortality [23]. These high rates are due to no supervision by skilled attendants, unplanned birth and, mainly, because of the poor access to emergency obstetric care services [21]. Table 1 summarizes global home birth rates and other specificities (Table 1).
| Country | Home Birth Rate | Assistance | Childhood Mortality |
|---|---|---|---|
| Bangladesh | 95% [13] | ||
| Nepal | 90% [13] | ||
| Ethiopia | 90% [14] | ||
| Nigeria | 62% [14] | 60% to 70% of all childhood mortality [16] | |
| Ghana | 43% [14] | ||
| Mozambique | 41% [13] | ||
| Netherlands | 30% [13] | Of women who deliver at home, 50% give birth attended by midwives [23] | Higher compared to other European countries [8] |
| UK | 1-2% [13] | ||
| Japan | 1.1% [22] | ||
| New Zealand | 1% [13] | ||
| USA | 0.6% [13] | ||
| France | 0.5% [20] | ||
| Australia | 0.4% [21] | ||
| Turkey | Only 83% of births are assisted by a doctor, nurse or midwife [13] |
Table 1: Global home birth specificities.
Factors influencing birthplace choices
Coxon et al. in 2017 [24] concluded that most of women do not feel they have a choice of place of birth or believe that their choice is very limited. In fact, planning birth in hospital was considered, for a long time, straightforward and irrefutable, as if it was not a choice at all.
In addition to the choice of location, in some countries it is still possible to choose who attends the delivery (midwife or obstetrician). Obstetricians are often chosen because they are associated with expertise and safety [18]. On the other hand, women who choose midwives tend to believe that birth is a natural process and should happen without interventions and technology [18].
The reasons why women have an out-of-hospital birth are totally different between countries. Social-cultural context and level of education is very important because it advises women’s insights and it is related to the use of health institutions [13,24,25]. Although many women feel that hospital is the safest place for birth (due to medical staff, pain relief available and not needing to transfer), many believe that hospital is impersonal and a place that provoke anxiety [24]. In fact, some developed countries, women choose to give birth at home mainly because they feel more safe and comfortable at home, want family involved, do not want interventions, want to control their birth experience or are afraid of hospitals [13,26].
Specificities by country: In Australia, 49.6% of the students prefer to give birth at the hospital with a doctor, 36.4% with a midwife and only 1,8% prefer to give birth at home with a midwife, most of them women [18].
In Netherlands, a study concluded that 60.7% of the women in midwife-led care at the onset of labor, planned to delivery at home [10].
Boucher et al. in 2009 [26], analyzed 160 women in USA and realized that 24% mentioned the concern of safety as being the main reason to choose a home birth. The fact that in USA, hospitals usually do not allow vaginal birth after a woman that had undergone cesarean section may be related with home births increment [7].
In the same way, a questionnaire distributed to 3283 Swedish women showed that they choose home birth because they want the presence of siblings or a female friend and they want to avoid pharmacologic pain relief [27].
Despite being a developed country, in Turkey, the main reason to choose home birth are economic difficulties, which mean that home birth is an indicator of low economic status, which is likely to have higher risks associated as these women are frequently untrained [13]. Besides, about 50% of Turkish women say that they feel more comfortable at home and also refer that they have difficulties to going to the hospital, are afraid of unfriendly behavior of hospital assistants and trust the person who would assist the home birth [13,26].
In undeveloped countries, the condition is quite different, where out-of-hospital deliveries are not exactly an option. Out-of-hospital delivery occurs at home, religious houses, birth attendants’ homes or on the way to hospital [23]. These births occur mainly due to limited access to health services, but also due to high cost of the delivery, unfriendly attitude of health care workers, lack of options of birthing positions, fear of surgery or other interventions (such as episiotomy, forceps, intravenous oxytocin), lack of privacy, cultural practices and desire to seek spiritual protections from prayer houses [6,21,23].
Groups of women that have out-of-hospital deliveries
There are specific groups more likely to experience out-of-hospital deliveries, like non-Hispanic white women (two to four times higher than any other racial or ethnic group), married women, older (≥ 25 or ≥ 35), multiparous, women who live in a longer distance from an obstetric unit, women that live in rural countries of less than 100,000 population, have a post-graduation or a master’s degree education (and less likely to have not completed high school)29 and women that had started prenatal care later (≥ 4 months) [2,6,11,17,19,28,29].
Specificities by country: Specifically in Canada, women interested in an alternative birth place (birthing room, home birth or birth center) were more likely to be older, married, cultured, interested in midwifery services and to have had a low-intervention vaginal birth [13].
In Turkey, births that take place in a health facility rise from 48% among women with no education to 97% among women with higher level of education [13].
In Netherlands, women that planned a home birth are more likely to be older, medium or high socio-economic status, multiparous and to give birth at 41 weeks gestation [10].
In France, Blondel et al. in 2011 [30], realized that out-of-hospital births occur more often in rural areas and the rate is higher the greater the distance to the maternity. In this country, unplanned out-of-hospital deliveries are more common among women of lower social class, which may be due to inaccessible healthcare services during pregnancy.
Differently of developed countries, in undeveloped, women who most deliver at home have lower level of education and lower wealth, but in the same way they are more frequently multiparous, resident in rural areas and had received little or none prenatal care [21,23,24]. Table 2 summarizes most common groups of women that have an outof- hospital birth (Table 2).
| Most common groups of women that have an out-of-hospital birth |
|---|
| Older than 25 [6,10,11,27,31] |
| Older than 35 [32] |
| Multiparous [6,10,11,19,27,31,32] |
| Rural areas [6,11,27,30,31] |
| Employed in fields where an educational qualification is needed [32] |
| Largest distance to hospital [30] |
| Non-Hispanic white women [6,11] |
| Master’s degree education [29] |
| Women that had started prenatal care later (≥ 4 months) [11] |
| Medium or high socio-economic status [10] |
Table 2: Most common group of women that have an out-of-hospital birth.
Maternal and clinical characteristics of higher risk women: Some facts about women who deliver at home:
• A home birth after cesarean delivery is associated with a higher fetal death rate than an in-hospital birth after cesarean delivery [4].
• Neonatal mortality rates for pregnancies with ≥ 41 weeks is the double than with <41 weeks if we consider uncertified midwives, but not with certified [12].
• Neonatal mortality rate in nulliparous women is more than double than in multiparous and the risk of 5 min Apgar score of 0 and the risk of seizures and neurologic dysfunction is also higher in nulliparas [5,12]. Multiparous are also, in general, less likely to have neonatal morbidity, labor dystocia, medical interventions and to require transfer to hospital when they have home deliveries. However, if we consider home births, multiparous have the same risk of perinatal morbidity than nulliparous [11].
• The risk of 5 min Apgar score of 0 is also higher in women >35 years old and the risk of a 5 min Apgar less than 4 and less than 7 are higher in women that had planned a home birth [11].
Considering that facts, it’s very important to select women who are not at high risk of complications, in order to reduce perinatal mortality at planned home births [13,31]. It’s possible to do that based in some criteria, such as the absence of any maternal disease (pre-existing or during pregnancy), a singleton fetus, a cephalic presentation, gestational age between 36-37 and 41-42 weeks, spontaneous labor and that the patient has not been transferred from another place to the hospital [4]. If these criteria are not present, planned home birth is associated with a higher risk of perinatal death. Other articles emphasize that women with higher risk of neonatal mortality are those with breech presentation or with a previous cesarean, nulliparous, gestational age ≥ 41 weeks and women ≥ 35 years old [10,31].
The American College of Obstetricians and Gynecologists consider that fetal malpresentation, multiple gestations or a previous cesarean delivery should be absolute contraindications to home birth [4].
Adverse maternal outcomes
Maternal outcomes can be divided in obstetric interventions’ outcomes and outcomes non-related with interventions [9].
Obstetric interventions’ outcomes include electronic fetal heart rate monitoring, labor induction or augmentation, epidural analgesia, episiotomy, instrumental vaginal delivery (forceps or vacuum) and cesarean delivery [9,11,19,27].
These kind of outcomes are less common in planned home births [4,9,11,27,32]. In fact, home births are more attended by midwives than hospital births, which is associated with fewer intrapartum interventions, such as induction, episiotomy, operative vaginal birth and cesarean delivery [4,26,27].
Other maternal outcomes, non-related with interventions, are: Mortality, lacerations (vaginal and perineal), infections, postpartum hemorrhage, retained placenta, umbilical cord prolapse [9]. Despite the fact that home birth is usually a prolonged labor, it has fewer vaginal lacerations and less maternal infection [4,27]. However, although some studies refer that hemorrhage and perineal lacerations occur less often in home births, other studies conclude that the rate is higher in those deliveries or do not conclude any significantly difference [27,32,33]. Kataoka et al. [19] in a retrospective cohort study in Japan concluded that perineal lacerations are less frequent in home births, but hemorrhage rate is higher.
Adverse newborn outcomes
The newborn outcomes most frequently evaluated in the literature about out-of-hospital deliveries are fetal death, neonatal death (death during the first 28 days after delivery), perinatal death (composite of fetal and neonatal deaths), infant death (death during the first year of life), 5 min Apgar score less than 4, 5 min Apgar score less than 7, prematurity, postdatism (≥ 42 weeks’ gestation), low birth-weight (<10% for gestational age or <2500 g), macrosomia (>90% for gestational age or ≥ 4000 g) and assisted ventilation requirement [7,9,11].
The most important risk mediators to perinatal mortality are defined as the “Big 4”: 4 conditions that, the presence of any of them entails a perinatal mortality rate of 85%. These conditions are: Congenital abnormalities, intrauterine growth restriction, preterm birth and low Apgar score (less than 7 at 5 min) [20]. These big 4 conditions are less prevalent in planned home births, which may result in a lower ratio mortality risk [34].
When we just need to compare intervention rates instead of mortality rates, we use the “Big 3 adjustment”, excluding low Apgar score [34]. That Big 3 conditions are related to a higher mortality rate at home, probably due to under-treatment because of delayed timing of intervention [34].
Neonatal and perinatal mortality: Studies from Netherlands, Canada and USA concluded that perinatal and neonatal mortality rates are similar in home and hospital delivery, if we consider women with low-risk pregnancies and expected normal deliveries and women that had received care from well-trained midwives, highly regulated and fully integrated into the health care system [27,34,35]. However, in Netherlands, if just multiparous women were considered, the rate of Apgar scores <7 and admission in intensive care units (ICU) was lower in planned home births [36]. De Jonge et al. [10] again in a Dutch study, of 529,688 low-risk births, also concluded that there was no difference between perinatal mortality rate in in-hospital delivery and out-ofhospital delivery. Nevertheless, in this country particularly, we have to consider that home births are perfectly integrated into the maternity care service system, midwives are well trained, the travel distances are short and only low risk women can choose their birth place (home or hospital) [34,36].
On the other hand, a meta-analysis of six studies comparing the birth outcomes of 24.092 low-risk pregnant women identified the double neonatal mortality rate among home births compared to inhospital births, but the same perinatal mortality [9]. In the same way, Grünebaum et al. [31] in a study from 2017, realized that neonatal mortality is significantly higher in planned home births. The causes of the increased risk of this neonatal mortality include neonatal brain damage and infections.
Planned home births have a greater proportion of deaths attributed to respiratory distress and failed resuscitation, probably due to some contributors that may raise neonatal mortality, such as personnel, training and equipment available for neonatal resuscitation [9].
It is very important to remind that many studies do not disaggregate in-hospital births in planned in-hospital births and unplanned (births that occur in hospital after intrapartum transfer of a woman who had planned an out-of-hospital birth), which results on the underestimation of out-of-hospital outcomes [5]. A study performed in Oregon during 2012 and 2013 disaggregate these births, by asking all women where they had planned to labor, in order to show the effects of this misclassification [7]. This study also excluded home births that were unplanned and births that occurred in other locations (clinic or doctor’s office) [7]. They concluded that before reclassification, fetal, perinatal and neonatal death did not differ significantly between groups, but after reclassification, the rates of fetal, perinatal and neonatal death were higher among planned out-of-hospital births.
Prematurity and postdatism: A meta-analysis of 12 studies performed in 2010, showed that babies that are delivered at home have the same perinatal mortality and are less likely to be born preterm or be of low weight than babies that are delivered in hospital. However, they are more likely to be postdating and the overall neonatal mortality is almost twice in planned home births vs. planned hospital births and almost tripled among non-anomalous neonates [9]. Similarly, in an USA study, only about 4.4% of out-of-hospital births were born preterm (less than 37 weeks), compared to 11.6% of in-hospital birth [2].
Premature birth mortality is more than double in out-of-hospital births than in in-hospital births, most of them because of neurological outcomes and hypothermia [3].
Risk of admission in intensive care units (ICU): The risk of admission in neonatal ICU is higher in in-hospital births, primiparous, 37 or 41 weeks gestation, ≥ 35 years old and low socio-economic status mothers [10].
Other outcomes: The Oregon study mentioned above also concluded after reclassification that depressed 5 min Apgar score, increased risk of 5 min Apgar score <4 and <7, neonatal seizures and maternal blood transfusions were higher among planned out-ofhospital births, however, they did not find no difference in infant death [7,11]. Obstetrical procedures were also more common among women who had planned in-hospital deliveries [7,9,11].
If risks are adjusted, some studies revealed that neonatal outcomes, such as assisted ventilation, prematurity, birth trauma, required resuscitation, meconium staining, low birth-weight, requiring oxygen beyond 24 h and admission in neonatal intensive care units, occur at similar or lower rates in out-of-hospital births than in in-hospital births [10,20,32,37]. However, other studies showed a higher frequency of these outcomes in out-of-hospital births [9,27].
Outcomes in unplanned deliveries: Some studies found that babies born in unplanned emergency settings have higher risk of complications due to hypoxia, infections, respiratory distress, hypothermia (24% of newborns), acidosis and prematurity (22% versus 8% for hospital deliveries) [38]. Intrapartum asphyxia was described as an excessive contributes to perinatal mortality accounting for among 31% to 51% of home deliveries deaths [27]. Hypothermia is also the main complication in accidental out-of-hospital births [17].
Outcomes in developing countries: It was estimated that 25% of home deliveries in undeveloped countries complicate with postpartum hemorrhage (6.6%), retained placenta (3.9%), severe birth asphyxia (3.2%) and early neonatal death (2.7%) [21]. Ashimi and Amole in 2015 [21] and Orimadegun et al. in 2008 [23] found that, in addition to the increased mortality, in the group of newborns delivered outside the hospital, there were also a higher rate of hypothermia, prematurity, perinatal asphyxia, hemorrhage, neonatal tetanus, sepsis, neonatal jaundice, anemia, seizures and fractures, because of poor environmental hygiene. Tables 3 and 4 summarize newborn and maternal outcomes most frequently cited and the reasons for these outcomes.
| Outcomes | Low risk in out-of-hospital delivery | No differences | High risk in out-of-hospital delivery |
|---|---|---|---|
| Fetal Mortality | [20,36] | [7] | |
| Neonatal Mortality | [9,27,32,36] | [7,9,31] | |
| Neonatal Seizures | [33] | [5,7,11] | |
| Perinatal Mortality | [9,10] | [7] | |
| Infant Mortality | [7] | ||
| Admission in Intensive Care Unit | [10] | ||
| Less Apgar index | [32,33] | [5,7,11] | |
| Hypoxic ischemic encephalopathy | [8] | ||
| Asphyxia at birth | [33] | ||
| Premature and low birth weight infant | 9 | [37] | |
| General obstetrical procedures | [7,9,11] | ||
| Episiotomy | [32] | ||
| Cesarean section | [32] | ||
| Vaginal lacerations | [4,27] | ||
| Perineum lacerations | [33] | ||
| Post-Partum Hemorrhage | [33] | 7 | |
| Maternal infections | [4,27] | [33] | |
| Sphincter/Rectal rupture | [32] |
Table 3: Newborn and maternal outcomes most frequently cited (numbers are the references).
| Reasons for the outcomes mentioned above |
|---|
| Causes of the increased risk of this neonatal mortality include neonatal brain damage and infections [31] |
| Higher risk of neonatal mortality: Breech presentation, previous cesarean, nulliparous, gestational age ≥ 41 weeks and women ≥ 35 years old [10,31] |
| The big 4 conditions are less prevalent in planned home births, which may result in a lower ratio mortality risk [35] |
| Unplanned birth outside an institution is associated with higher mortality rates, especially in nulliparous women [39] |
| In developing countries, high rates are due to no supervision by skilled attendants, unplanned birth, poor access to emergency obstetric care services and poor environmental hygiene [21] |
Table 4: Reasons for the outcomes.
The transport problem and unplanned out-of-hospital births
A safe and timely transport of a laboring woman is an important factor that influences the safety of planned home birth [4]. It is possible to define a travel zone as the physical area in which women are estimated to reach the nearest obstetric center within a given time [39].
In Norway, 12.7% of the women that planned a home birth are transfer to hospital (8%-56% of primiparous and 6%-16% of multiparous). These transfers occur whether intrapartum or within the first five days after birth [25]. In France, the transfer rate to the hospital is between 15% and 30% [30].
In part because of this, the risks of planned home birth are usually underestimated, since 0.4% of all low risk pregnancies, 9% of multiparous and 37% of nulliparous women intending to home birth are transferred to hospital, which means that negative outcomes of planned home births are wrongly associated to hospital births [9,40].
Women are most frequent transferred during labor because of an abnormal labor progress (like slow progress in labor), need for pain relief, hypertension, hemorrhage, fetal malpresentation, fetal distress or the presence of a midwife that could not stay longer [25,27]. Blix et al. [25] reported that the main reason is the slow progress in labor, while Dencker et al. [33] concluded that the main reason is meconium- stained liquor and/or fetal heart rate abnormalities.
The main reasons for postpartum transfer are: hemorrhage, retained placenta and neonatal infection and respiratory complications [25].
The risk of unplanned delivery outside an institution is five times higher in the 1-2 h travel zone compared to the <1 hour travel zone [39]. Amelink-Verburg et al. [40] realized that a time of ≥ 20 min by car is associated with an increased risk of mortality and adverse outcomes in term women. Therefore, the risk of unplanned birth outside an institution is strongly related with the largest travel time to the nearest institution [39].
Thus, even for a planned home birth it is essential to ensure the accessibility to maternity care services in order to transfer in case of emergency, since unplanned birth outside an institution is associated with higher mortality rates, especially in nulliparous women [30,39]. In fact, we can observe a higher mortality rate in babies from pregnant women that were transfer to hospital, compared to babies of women who started labor in secondary care [41].
In some reports from developed countries, the incidence of unplanned out-of-hospital deliveries varied from 0.1 to 2%. The incidence is about 0.1% in Finland, 0.31% in UK, 0.6% in Scotland [6,38].
Factors associated with accidental out-of-hospital deliveries include: inappropriate transport, single mothers, low maternal schooling, multiparty and lack of prenatal care, which by themselves might increase the risk for adverse perinatal outcome [6,38].
Factors that could lead to delay the way to the hospital are: The transport time, time until the reference decision, poor accessibility to the hospital, demographic factors (age, education, parity, area of residence, socio-economic status, religion, ethnic), socio-cultural status (women empowerment, engagement in job), economic position, service factors (satisfaction with hospital services, counseling and information during prenatal phase), deprived pre-planning and birth preparedness and obstetric factors (onset of labor-delivery time) [22,41]. In Nepal, for example, although the easy access to hospital, many women (mostly of middle or lower socio-economic class) go to hospital so late that they deliver on the way, due to inadequate counseling [22].
The specific case of water births
This kind of birth was first reported in France in 1803 and become popular through the 1980s and 1990s around Europe, United Kingdom and Canada [42]. Nowadays, almost 1% of births in United Kingdom include one period of immersion or more [43]. On the other hand, the prevalence in USA is unknown, but a survey from 2001 found that 143 USA birthing centers have immersion in water during labor [15].
Giving birth in water involves the complete delivery of the baby under warm water, which activates mother’s peripheral neurological receptors leading to pain relief and promotes increasing venous return and mobilization of extravascular fluid [14,15,42]. When women are immersed in warm water, other benefits besides pain relief were reported, such as decrease rate of cesarean sections, less episiotomies, feeling safer and more relaxed, a reduction in blood loss and perineal trauma, as well as an optimization of the work process, with a shorter active phase of the first and third stages [14-16,42]. In this context, American Academy of Pediatrics concluded that immersion in water during the first stage of labor may be tempting (due to pain relief, shorter duration of labor and less use of anesthesia), but no maternal or fetal benefits were found in immersion during the second stage of labor [15].
Due to the benefits mentioned above, women who underwent water birth receive less anti-spasmodic drugs, opiates, analgesics and oxytocin during labor and, in a study from Chaichian et al. [14] all of those women gave birth naturally (a normal vaginal deliver), instead of a conventional birth, whereas only 79.2% gave birth this way. However, other studies revealed higher rate of perineal lacerations (but less severe than in conventional delivery) and others did not find any difference in duration of first and second stages of labor [14,42].
Some studies actually believe that water birth is not less painful than conventional birth, but in reality, it elevates the pain threshold and pain acceptance by increased comfort [14].
Although water birth has become a popular method, it remains controversial because of neonatal outcomes, such as risk of aspiration, hypoxemia, infection, difficulties in neonatal thermoregulation, umbilical cord rupture, newborn respiratory problems, seizures, perinatal asphyxia and higher rate of low Apgar score ≤ 7 at 1 min [14-16,42]. Anyhow, other studies showed no difference on the risk of infection and no negative impact on newborns between women who had water births and conventional births, if the water is correctly sanitized [16]. Menakaya et al. [42] found that the risk of low Apgar score ≤ 7 at 1 min is higher in multiparous women than primarous and the risk of low Apgar score at 5 min is the same in women that deliver in water or in a conventional way.
A Cochrane review randomized controlled trials, which involved 3243 women, concluded that there was no evidence of increased adverse newborn or maternal outcomes from water birth [44,45].
It’s still necessary to develop rigorous protocols to select women who may safely have a water birth, maintenance and cleaning of the water, infection controls procedures, fetal and mother’s monitoring at suitable intervals while immersed [15].
Review Learning Points
It is very important to understand that the perception of safety depends on the person we are talking about, because while women see safety in giving birth in a familiar environment, at her comfort zone, with her family and friends, obstetricians perceived safety in terms of skills and conditions that may save the newborn in case of complications.
Most important of all is to respect the choice of the woman, namely, where she feels safer, the place that will decrease her stress, in order to better outcomes of pregnancy, labor and births [29]. Obstetricians should inform women with evidence-based recommendations, explaining them the risk of neonatal mortality and showing that home births are strongly associated with worse outcomes [5].
Although many studies showed similar maternal-fetal outcomes for planned out-of-hospital births versus planned hospital births, its safety still remains controversial because the benefits may be overcome by the disadvantages associated with delayed treatment [7,10,34].
The recommendations about planned home birth diverge in different countries and even international Colleges disagree, since the American College of Obstetricians and Gynecologists is against home births and Royal College of Obstetricians and Gynecologists in the United Kingdom believes home births are a good choice for uncomplicated pregnancies [32].
In Netherlands, maternity care is divided into primary (for lowrisk women) and secondary (for high-risk women). Midwives only provide care to a low-risk woman and these women are the only ones that may choose to have a home birth. The secondary care is provided by obstetricians and it is the only care that may use interventions, such as pharmacological pain relief, fetal monitoring and augmentation of labor [10]. Perhaps the implementation of Netherlands’ measures on other countries could reduce the high mortality rates in out-of-hospital deliveries, can correctly separate high-risk pregnancies from low-risk pregnancies, given the same geographical issues.
In low risk pregnant women, midwifery-led units seem to reduce the risk of unnecessary interventions, such as episiotomy and amniotomy and confer a good outcome [33]. However, recent systematics reviews of cohort studies of home birth, reported fewer maternal interventions, but higher neonatal mortality rates than in-hospital births [7,9]. In fact, avoiding medical technology and interventions, considered an advantage of planned home birth, may represent a major contributor to neonatal and perinatal deaths [27].
Several studies documented that home births attended by registered midwives were not associated with an increased risk of adverse neonatal outcomes [10]. On the other hand, some studies recognized that choosing a home birth attendant by a certified or uncertified midwife does not improve neonatal mortality, when compared to planned hospital births, which have significantly lower neonatal mortality rates [12].
Conclusion
1. It is primordial to ensure that women have a good prenatal and labor care in order to achieve a safe maternity. In fact, the maternity care is an important factor to ensure good maternal and fetal morbidities and mortality. Besides, it is also important to inform women of their options to deliver and the benefits of each. They should be informed that the relative risk remains on debate and although there are fewer maternal interventions, some studies revealed a higher risk of neonatal and perinatal morbimortality.
2. Place of birth should be categorized as planned in-hospital, on the way to hospital, planned out-of-hospital and accidental out-of-hospital, by asking women where they plan to deliver, to truly understand the outcomes in each place, since nowadays a substantial number of adverse outcomes attributed to hospital births result from births on the way to hospital or transfers from home births that complicated. Only with this categorization it will be possible to truthfully understand out-of-hospital outcomes.
3. Most of the studies concluded that, although women who choose an out-of-hospital birth have low risk pregnancies and fewer interventions, newborns have a higher risk of poor outcomes, such as seizures, low Apgar score and neonatal and perinatal mortality.
4. Pregnant high-risk women (nulliparous, ≥ 41 weeks gestation, fetal malpresentation, multiple gestations, previous cesarean delivery, congenital abnormalities, intrauterine growth restriction, preterm birth or women with medical or obstetric complications) should be excluded from home births.
5. It would be also important to create medical teams capable of effectively and timely transfer a pregnant woman to the hospital when necessary, because although planned home birth is an established practice in many developed countries, there is no system capable of ensuring a birth as safe as desire.
6. Special attention should be given to avoid unplanned deliveries, which greatly increase the neonatal and perinatal mortality rate.
7. As far as water deliveries are concerned, further studies are needed to confirm their safety, since the studies performed are still few, with small samples, retrospective studies of a single center and many are not intended to find the greatest outcomes as differences in neo and perinatal mortality.
8. Future research should identify specific contributors to reduce neonatal and maternal morbimortality.
9. Further studies, however, should be carefully planned since major ethical issues arise during obstetric scientific investigation.
10. In summary, planned home birth remains a debated choice.
References
- Rocha VAD (2009) A água como meio alternativo para o nascimento natural. Dissertação de Mestrado em Ciências de Enfermagem.
- Macdorman MF, Declercq E, Mathews TJ (2013) Recent trends in out-of-hospital births in the United States. J Midwifery Womens Health 58: 494-501.
- Jones P, Alberti C, Julé L, Chabernaud JL, Lode N, et al. (2010) Mortality in out-of-hospital premature births. Acta Paediatr Int J Paediatr 100: 181-187.
- Cohain JS (2014) Apgar score of 0 at 5 min and neonatal seizures or serious neurologic dysfunction in relation to birth setting. Am J Obstet Gynecol 210: 377.
- Sheiner E, Ohel I, Hadar A (2006) Out-of-hospital deliveries. In: Lynch CB, Keith LG, Karoshi M (Eds), A textbook of postpartum hemorrhage: A comprehensive guide to comprehension, management and surgical intervention. London: Sapiens Publishing, pp: 413-420.
- Snowden JM, Tilden EL, Snyder J, Quigley B, Caughey AB, et al. (2015) Planned out-of-hospital birth and birth outcomes. N Engl J Med 373: 2642-2653.
- Wasden SW, Chasen ST, Perlman JM, Illuzzi JL, Chervenak FA, et al. (2016) Planned home birth and the association with neonatal hypoxic ischemic encephalopathy. J Perinat Med.
- Wax J, Lucas F, Lamont M, Pinette MG, Cartin A, et al. (2010) Maternal and newborn outcomes in planned home birth vs planned hospital births: A meta analysis. Am J Obstet Gynecol 203: 243e1-e8.
- De-Jonge A, Goes BYVD, Ravelli ACJ, Amelinkâ€Verburgm MP, Mol BW, et al. (2009) Perinatal mortality and morbidity in a nationwide cohort of 529 688 low-risk planned home and hospital births. BJOG 116: 1177-1184.
- Cheng YW, Snowden JM, King TL, Caughey AB (2013) Selected perinatal outcomes associated with planned home births in the United States. Am J Obstet Gynecol 209: 325.e1-e8.
- Grünebaum A, McCullough LB, Arabin B, Brent RL, Levene MI, et al. (2016) Neonatal mortality of planned home birth in the United States in relation to professional certification of birth attendants. PLoS One 11: 1-7.
- Kukulu K, Öncel S (2009) Factors influencing women’s decision to have a home birth in rural Turkey. Midwifery 25: 32-38.
- Chaichian S, Akhlaghi A, Rousta F, Safavi M (2009) Experience of water birth delivery in Iran. Arch Iran Med 12: 468-471.
- American Academy of Pediatrics (2014) Immersion in water during labor and delivery. Pediatrics 133: 758-761.
- Demirel G, Moraloglu O, Celik IH, Oguz SS, Nurdan Uras, et al. (2013) The effects of water birth on neonatal outcomes: A-five-year results of a referal tertiary centre in Turkey. Early Hum Dev 17: 1395-1398.
- Renesme L, Garlantézec R, Anouilh F, Bertschy F, Carpentier M, et al. (2013) Accidental out-of-hospital deliveries: A case-control study. Acta Paediatr Int J Paediatr 102: 174-177.
- Stoll KH, Hauck YL, Hall WA (2016) Home or hospital? Midwife or physician? Preferences for maternity care provider and place of birth among Western Australian students. Women Birth 29: e33-e38.
- Kataoka Y, Eto H, Iida M (2013) Outcomes of independent midwifery attended births in birth centres and home births: A retrospective cohort study in Japan. Midwifery 29: 965-972.
- Kooy JVD, Poeran J, De-Graaf JP (2011) Planned home compared with planned hospital births in the Netherlands. Obstet Gynecol 118: 1037-1046.
- Ashimi AO, Amole TG (2015) Prevalence, reasons and predictors for home births among pregnant women attending antenatal care in Birnin Kudu, North-west Nigeria. Sex Reprod Healthc 6: 119-125.
- Chaudhary P (2005) Accidental-out-of-hospital deliveries: Factors influencing delay in arrival to maternity hospital. Kathmandu Univ Med J 3: 115-122.
- Orimadegun AE, Akinbami FO, Tongo OO, Okereke JO (2008) Comparison of neonates born outside and inside hospitals in a children emergency unit, Southwest of Nigeria. Pediatr Emerg Care 24: 354-358.
- Coxon K, Chisholm A, Malouf R, Rowe R, Hollowell J (2017) What influences birth place preferences, choices and decision-making amongst healthy women with straightforward pregnancies in the UK? A qualitative evidence synthesis using a “best fit†framework approach. BMC Pregnancy Childbirth 17: 103.
- Blix E, Huitfeldt AS, Oian P, Straumea B, Kumle M (2012) Outcomes of planned home births and planned hospital births in low-risk women in Norway between 1990 and 2007: A retrospective cohort study. Sex Reprod Healthc 3: 147-153.
- Boucher D, Bennett C, McFarlin B, Freeze R (2009) Staying home to give birth: Why women in the united states choose home birth. J Midwifery Women’s Heal 54: 119-126.
- Wax JR, Pinette MG, Cartin A (2010) Home versus hospital birth-process and outcome. Obstet Gynecol Surv 65: 132-140.
- Ovaskainen K, Ojala R, Gissler M, Luukkaala T, Tammela O (2015) Out-of-hospital deliveries have risen involving greater neonatal morbidity: Risk factors in out-of-hospital deliveries in one University Hospital region in Finland. Acta Paediatr Int J Paediatr 104: 1248-1252.
- Sperlich M, Gabriel C, Seng J (2016) Where do you feel safest? Demographic factors and place of birth. J Midwifery Womens Health.
- Blondel B, Drewniak N, Pilkington H, Zeitlin J (2011) Out-of-hospital births and the supply of maternity units in France. Health Place 17: 1170-1173.
- Grünebaum A, McCullough LB, Sapra KJ, Arabin B, Chervenak FA (2017) Planned home births: The need for additional contraindications. Am J Obstet Gynecol.
- Janssen PA, Saxell L, Page LA, Klein MC, Liston RM, et al. (2009) Outcomes of planned home birth with registered midwife versus planned hospital birth with midwife or physician. Can Med Assoc J 181: 377-383.
- Dencker A, Smith V, McCann C, Begley C (2017) Midwife-led maternity care in Ireland-a retrospective cohort study. BMC Pregnancy Childbirth 17: 101.
- Van-der-Kooy J, Birnie E, Denktas S, Steegers EA, Bonsel GJ (2017) Planned home compared with planned hospital births: Mode of delivery and Perinatal mortality rates, an observational study. BMC Pregnancy Childbirth 17: 177.
- Lindgren HE, RÃ¥destad IJ, Christensson K, Hildingsson IM (2008) Outcome of planned home births compared to hospital births in Sweden between 1992 and 2004. A population-based register study. Acta Obstet Gynecol Scand 87: 751-759.
- De Jonge A, Geerts CC, Goes BYVD, Mol BW, Buitendijk SE, et al. (2014) Perinatal mortality and morbidity up to 28 days after birth among 743 070 low-risk planned home and hospital births: A cohort study based on three merged national perinatal databases. BJOG 122: 720-728.
- Pirneskoski J, Peräjoki K, Nuutila M (2016) Urgent EMS managed out-of-hospital delivery dispatches in Helsinki. Scand J Trauma Resusc Emerg Med 24: 94
- Lazić Z, TakaÄ I (2011) Outcomes and risk factors for unplanned delivery at home and before arrival to the hospital. Wien Klin Wochenschr 123: 11-14.
- Engjom HM, Morken NH, Hoydahl E, Norheim OF, Klungsoyr K (2017) Increased risk of peripartum perinatal mortality in unplanned births outside an institution: A retrospective population-based study. Am J Obstet Gynecol 217: 210.e1-e12.
- Amelink-Verburg MP, Verloove-Vanhorick SP, Hakkenberg RMA, Veldhuijzen IME, Gravenhorst JB, et al. (2008) Evaluation of 280 000 cases in Dutch midwifery practices: A descriptive study. BJOG 115: 570-578.
- Evers ACC, Brouwers HAA, Hukkelhoven CWPM (2010) Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: Prospective cohort study. BMJ 341: 981.
- Menakaya U, Albayati S, Vella E, Fenwick J, Angstetra D (2013) A retrospective comparison of water birth and conventional vaginal birth among women deemed to be low risk in a secondary level hospital in Australia. Women Birth 26: 114-118.
- Davies MW (2010) Water births and the research required to assess the benefits versus the harms. J Paediatr Child Health 48: 726-729.
- Cluett E, Burns E (2007) Immersion in water in pregnancy, labour and birth (Review). Cochrane Libr.
- Gottfredsdottir H, Magnúsdóttir H, Hálfdánsdóttir B (2015) Home birth constructed as a safe choice in Iceland: A content analysis on Icelandic media. Sex Reprod Healthc 6: 138-144.
Citation: Amorim D, Machado HS (2018) Newborn and Maternal Outcomes in Out-of-Hospital Delivery: A Review. J Preg Child Health 5: 371. DOI: 10.4172/2376-127X.1000371
Copyright: © 2018 Amorim D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7458
- [From(publication date): 0-2018 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 6340
- PDF downloads: 1118