Short Communication Open Access
New Scoring System Available at Home Health Care for Prediction of 14 Days Survival in Lung Cancer Complicated with Lymphangitic Carcinomatosis
Satomi Konno1, Takuya Kishi2*, Hideyuki Kashiwagi3, Takehiko Makino3 and Takeyuki Matsuguchi1
2Department of Advanced Therapeutics for Cardiovascular Diseases, Kyushu University Graduate School of Medical Sciences, Japan
3Department of Palliative Care, Aso-Iizuka Hospital, Japan
- *Corresponding Author:
- Takuya Kishi
Department of Advanced Therapeutics for Cardiovascular Diseases
Kyushu University Graduate School of Medical Sciences
3-1-1 maidashi, higashi-ku, Fukuoka 812-8582, Japan
Tel: 81-92-642-5360
E-mail: tkishi@cardiol.med.kyushu-u.ac.jp
Received date: September 23, 2014; Accepted date: November 13, 2014; Published date: November 22, 2014
Citation: Konno S, Kishi T, Kashiwagi H, Makino T, Matsuguchi T (2014) New Scoring System Available at Home Health Care for Prediction of 14 Days Survival in Lung Cancer Complicated with Lymphangitic Carcinomatosis. J Palliat Care Med 4:200. doi:10.4172/2165-7386.1000200
Copyright: © 2014 Konno S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: Patients with lung cancer often greeted their terminal phase in the treatment at home, and many
cases complicated with lymphangitic carcinomatosis took a sudden turn. The aim of the present study was to
determine a scoring system available at home health care for prediction of short-term survival of lung cancer
complicated with lymphangitic carcinomatosis.
Methods: In 14 lung cancer patients with lymphangitic carcinomatosis in our medical care at home, we
determined significant close correlated and independent factors for assuming death during 14 days by logisticregression
analysis, and made out new scoring system. Moreover, we determined cut-off value on receiveroperating
characteristics analysis.
Results: In our scoring system calculated as the summation points awarded for the presence of 5 parameters
(i.e., systolic blood pressure<90 mmHg, 2 point; pulse rate>100 beats/minute, 3 point; blood oxygen
saturation<90%, 3 point; oxygen dose>2 L/minute, 2 point; respiratory frequency>20 times/minute, 3 point), cut-off
value was 8 (sensitivity 90%, specificity 68%).
Conclusions: We made a new a scoring system available at home health care for prediction of 14 days survival
of lung cancer complicated with lymphangitic carcinomatosis assumed systolic blood pressure, pulse rate,
respiratory frequency, blood oxygen saturation, and oxygen dose.
Keywords
Lung cancer; Lymphangitic carcinomatosis; Home health care; Survival
Introduction
Background
In our Iizuka city at Japan, aging has suddenly advances, because of lacking alternate industries for traditional coal industry. Moreover, we have so many households including only elderly people, as symbolizing the Japanese community, and it is necessary to do the home health care for end-stage illness, especially malignant cancer. In the aspect of home health care for end-stage, the remained survival would provide important and indispensability information to patients, patients’ family, and physicians. Lynn et al. showed that the end-of-life course varied according to disease (senility, heart failure, respiratory failure, and cancer) [1]. Among the diseases, in cancer, survival would be suddenly deteriorated by the decompensated general body function, although body function is relatively maintained until several months before death. Considering these backgrounds, prediction of survival in short term is necessary as clinical commitment for clinicians of oncology and palliative care to produce the meaningful remained days without excess anxiety for patients and to avoid inappropriate treatments [2].
Previous studies have already established the objective prediction for survival in patients with end-stage malignant cancer [3-8]. Maltoni et al. indicated that clinical survival prediction (clinical prediction of survival (CPS)) and prognostic scores are recommended (level A) based on evidence in the prognostic correlation within 90 days [3]. Stone et al. discussed Palliative Prognostic Score (PaP), Palliative Prognostic Index (PPI), terminal cancer prognostic (TCP) score, Bruera poor prognostic indicator, and Chuang prognositic score (CPS), and concluded that the prognostic scales offer an improvement on unadjusted clinician estimates of survival, in spite of several limitations [3-8]. The PPI established as an objective 3 weeks prognosis estimated evaluation of the cancer in terminal phase is available at home health care without drawing blood. Interestingly, recent paper suggested that Prognosis in Palliative care Study without blood results could be performed as well as clinician’ estimates of survival [9].
Lung cancer is most common in patients with cancer in our country. Therefore, patients with lung cancer often greeted their terminal phase in the treatment at home health care. At the start of the present study, we consecutively experienced the sudden and not anticipated death of lymphangitic carcinomatosis in such a period. However, we have no methods available at home health care to predict short-term survival of such patients. Therefore, the aim of the present study was to determine a scoring system available at home health care for prediction of short-term survival of lung cancer complicated with lymphangitic carcinomatosis.
Methods
Among the patients who took home health care of Matsuguchi Clinic between January 2010 and December 2012, 14 consecutive lung cancer patients with lymphangitic carcinomatosis were retrospectively enrolled. We defined 15 days survival as the primary outcome. Clinical parameters at the first visit to patient’s home after the initiation of home health care by out clinic were assessed, because out motivation was to determine the predictive tool of short-term survival at the first visit to patient’s home. Continuous variables were compared by unpaired t-test. Categorical variables were compared by Fischer’s exact test. Univariate and multivariate analysis with a logistic regression model were done to calculate adjusted odds ratio (OR) and 95% confidence interval (CI) to assess the influence of each variable to 15 days survival. Significant variables in the univariate analysis were assessed in the multivariable analysis. Weighed scores were allocated to each selected variable on the basis of each OR, and we made a new scoring system. Moreover, a cut-off point was obtained by receiver-operating characteristic (ROC) analysis with SPSS(SPSS Inc., Chicago, IL, U.S.A.). A ROC curve was made by which the area under the curve (AUC) for the score was calculated. All data are expressed as mean ± standard deviation. Significance was regarded as P<0.05. The present study complied with the Declaration of Helsinki. Informed consent was obtained from all patients before enrollment.
Results
Among the enrolled 14 patients (10 males and 4 females, mean age was 67 ± 3 years), 6 patients (5 males and 1 female, mean age was 69 ± 5 years) died within 15 days at home. Table 1 showed the clinical parameters at the first visit to patient’s home after the initiation of home health care by out clinic.
| Deathwithin 15 days(n=6) | Survivalover 15 days(n=8) | Total(n=14) | |
|---|---|---|---|
| Age (years old) | 69 ± 5 | 66 ± 3 | 67 ± 3 |
| SBP (mmHg) | 92 ± 18* | 112 ± 19 | 105 ± 24 |
| DBP (mmHg) | 61 ± 6 | 64 ± 11 | 63 ± 9 |
| Heart rate (bpm) | 98 ± 21* | 84 ± 19 | 89 ± 20 |
| SpO2 (%) | 90 ± 3* | 94 ± 4 | 92 ± 5 |
| O2 (L/min) | 4 ± 2* | 2 ± 1 | 2 ± 1 |
| RF (times/min) | 24 ± 3* | 19 ± 4 | 21 ± 6 |
| Body temperature | 37 ± 2 | 37 ± 1 | 37 ± 1 |
| Body weights (kg) | 54 ± 9 | 57 ± 6 | 58 ± 8 |
Table 1: *P<0.05 vs. patients with survival over 15 days (SBP: systolic blood pressure; DBP: diastolic blood pressure; bpm: beats per minute; RF: respiratory frequency).
In the univariable analysis, a significant difference was found in systolic blood pressure<90 mmHg, pulse rate>100 beats/minute, blood oxygen saturation<90%, oxygen dose>2 L/minute, respiratory frequency>20 times/minute (Table 2). According to the multivariable analysis, systolic blood pressure<90 mmHg, pulse rate>100 beats/minute, blood oxygen saturation<90%, oxygen dose>2 L/minute, respiratory frequency>20 times/minute were independent factors for 14 days survival (Table 2).
| UnivariateP | Multivariate odds ratio (95% CI) | P | |
|---|---|---|---|
| Age | 0.88 | ||
| Sex | 0.19 | ||
| Metastasis | 0.13 | ||
| SBP<90 mmHg | 0.01 | 1.69 (1.32-2.04) | 0.01 |
| DBP<60 mmHg | 0.19 | ||
| HR>100 bpm | 0.02 | 2.57 (2.11-2.98) | 0.03 |
| SpO2<90% | 0.05 | 2.88 (2.45-3.27) | 0.03 |
| O2>2 L/min | 0.01 | 1.82 (1.27-2.39) | 0.04 |
| Body temperature | 0.17 | ||
| Respiratory frequency>20/min | 0.04 | 2.52 (1.99-3.10) | 0.03 |
Table 2: Univariate and Multivariate analysis (SBP: systolic blood pressure; DBP: diastolic blood pressure; HR: heart rate; bpm: beats per minute).
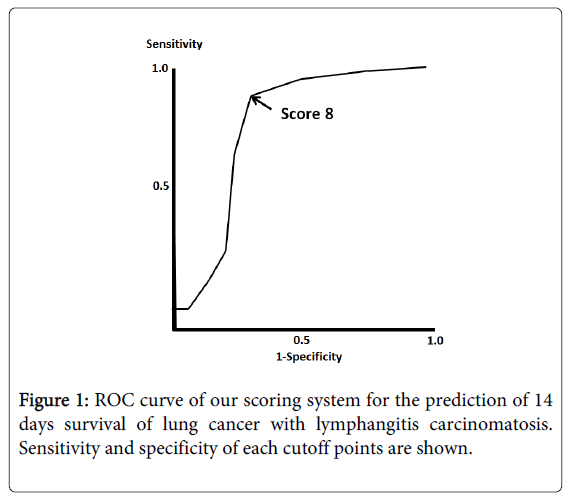
Considering the results of multivariate logistic analysis, systolic blood pressure<90 mmHg, pulse rate>100 beats/minute, blood oxygen saturation<90%, oxygen dose>2 L/minute, respiratory frequency>20 times/minute were selected to our new scoring system, calculated as the summation points awarded for the presence of 5 parameters (ie, systolic blood pressure<90 mmHg (OR 1.69), 2 point; pulse rate>100 beats/minute (OR 2.57), 3 point; blood oxygen saturation<90% (OR 2.88), 3 point; oxygen dose>2 L/minute (OR 1.82), 2 point; respiratory frequency>20 times/minute (OR 2.52), 3 point). ROC analysis revealed that cutoff value was 8 (90% of sensitivity, specificity 68%) (Figure 1).
Discussion
In the present study, we made a new a scoring system for prediction of 14 days survival of lung cancer complicated with lymphangitic carcinomatosis assumed systolic blood pressure, pulse rate, respiratory frequency, blood oxygen saturation, and oxygen dose. Cut-off value of summation points awarded for the presence of 5 parameters (systolic blood pressure<90 mmHg, 2 point; pulse rate>100 beats/minute, 3 point; blood oxygen saturation<90%, 3 point; oxygen dose>2 L/minute, 2 point; respiratory frequency>20 times/minute, 3 point) was 8 (90% of sensitivity, specificity 68%) by ROC analysis.
Previous many studies have demonstrated that the survival of malignant cancer can be predicted significantly by decrease in false cholinesterase [3,10], increase in vitamin B12 [3,11], increase in serum bilirubin [3,12] with multivariate analysis and increase in C-reactive protein [3,11,13], decrease in lymphocytes [3,5,10], and increase in leukocytosis [5,10] statistically. However, these parameters are assessed by blood sample, and are not easily used in home health care. In these aspects, our present results and scoring system have clinical implications. Furthermore, it will be certain that wearing devices of body monitoring would spread by medical innovation in future, and the present scoring system could be calculated automatically at home health care by the future wearing medical devices without the visiting of medical staff.
Limitation and Strengths
The present study is just only a biased retrospective assessment at a single center, and the statistic power is not so high. Moreover, the sample size per 3 years was small, because we focused only lymphangitic carcinomatosis, which is not major in lung cancer overall. Not only lymphangitic carcinomatosis, the patients who had advanced stages of lung cancer could have suffered from many kinds of symptoms and conditions. Moreover, we used the parameters only assessed at the first visit to patient’s home after the initiation of home health care by out clinic, because out motivation was to determine the predictive tool of short-term survival at the first visit to patient’s home. We did not assess the time course of clinical parameters as predictive value. Considering these limitations, we could not provide our scoring system as a useful definitive predictive tool in clinical practice for lung cancer from only the present results.
The study’s greatest strength is that we tried to make a new and potentiated scoring system available at home health care for prediction of 14 days survival of lung cancer complicated with lymphangitic carcinomatosis assumed systolic blood pressure, pulse rate, respiratory frequency, blood oxygen saturation, and oxygen dose. Next future prospective large and multi-center studies are necessary to determine whether our concept would be really useful in clinical practice for lung cancer.
Acknowledgement
The Department of Advanced Therapeutics for Cardiovascular Diseases, Kyushu University Graduate School of Medical Sciences, is supported by Otsuka Pharma and Nippon Boehringer Ingelheim (to Dr. Kishi). We would like to make special thanks to all the medical staff of Matsuguchi Clinic.
References
- Lynn J (2001) Perspectives on care at the close of life. Serving patients who may die soon and their families: the role of hospice and other services. JAMA 285: 925-932.
- Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, et al. (2004) Trends in the aggressiveness of cancer care near the end of life. J ClinOncol 22: 315-321.
- Maltoni M, Caraceni A, Brunelli C, Broeckaert B, Christakis N, et al. (2005) Prognostic Factors in Advanced Cancer Patients: Evidence-Based Clinical Recommendations-A Study by the Steering Committee of the European Association for Palliative Care. J ClinOncol 23: 6240-6248.
- Stone PC, Lund S (2007) Predicting prognosis in patients with advanced cancer. Ann Oncol 18: 971-976.
- Pirovano M, Maltoni M, Nanni O, Marinari M, Indelli M, et al. (1999) A new palliative prognostic score: a first step for the staging of terminally ill cancer patients. Italian Multicenter and Study Group on Palliative Care. J Pain Symptom Manage 17: 231-239.
- Doyle D, Hanks G, Cherny N, Calman K (2005) Oxford textbook of palliative medicine, (3rdedn), Oxford University Press.
- Bruera E, Miller MJ, Kuehn N, MacEachern T, Hanson J (1992) Estimate of survival of patients admitted to a palliative care unit: a prospective study. J Pain Symptom Manage 7: 82-86.
- Chuang RB, Hu WY, Chiu TY, Chen CY (2004) Prediction of survival in terminal cancer patients in Taiwan: constructing a prognostic scale. J Pain Symptom Manage 28: 115-122.
- Gwilliam B, Keekey V, Todd C, Glitins M, Roberts C, et al. (2012) Development of Prognosis in Palliative care Study (PiPS) predictor models to improve prognostication in advanced cancer: prospective cohort study. BMJ Support Palliat Care 2: 63-71.
- Maltoni M, Pirovano M, Nanni O, Marinari M, Indelli M, et al. (1997) Biological induces predictive of survival in 519 Italian terminally ill cancer patients: Italian terminally ill cancer patients: Italian Multicancer and Study Group on Palliative Care. J Pain Symptom Manage 13: 1-9.
- Geissbühler P, Mermillod B, Rapin CH (2000) Elevated serum vitamin B12 levels associated with CRP as a predictive factor of mortality in palliative care cancer patients: a prospective study over five years. J Pain Symptom Manage 20: 93-103.
- Rosenthal MA, Gebski VJ, Kefford RF, Stuart-Harris RC (1993) Prediction of life-expectancy in hospice patients: identification of novel prognostic factors. Palliat Med 7: 199-204.
- McMillan DC, Elahi MM, Sattar N, Angerson WJ, Johnstone J, et al. (2001) Measurement of the systemic inflammatory response predicts cancer-specific and non-cancer survival in patients with cancer. Nutr Cancer 41: 64-69.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14452
- [From(publication date):
November-2014 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9915
- PDF downloads : 4537