Research Article Open Access
New Frontiers of People-Centered Integrated Care for Complex Chronic Disease
Stellato K1*, Radini D1, Pellizzari M2, Pordenon M2, Pletti L2, Humar F1, Apuzzo M1 and Di Lenarda A11Cardiovascular Center, Healthcare Authority AAS no. 1, Triestina and University of Trieste, Italy
2Cardiovascular Center, Healthcare Authority AAS no. 2, Bassa Friulana-Isontina, Italy
- *Corresponding Author:
- Kira Stellato
MS. Psy, LP, Cardiovascular Center
Healthcare Authority AAS
no. 1 – Triestina and University of Trieste, Italy
Tel: +39-3392472453
Fax: 040-3992935
E-mail: kira.stellato@phd.units.it
Received date: August 25, 2015 Accepted date: September 22, 2015 Published date: September 25, 2015
Citation: Stellato K, Radini D, Pellizzari M, Pordenon M, Pletti L, et al. (2015) New Frontiers of People-Centered Integrated Care for Complex Chronic Disease. J Palliat Care Med 5:234. doi:10.4172/2165-7386.1000234
Copyright: © 2015 Stellato K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: Heart failure is a chronic, progressive clinical syndrome with an unpredictable trajectory and difficult prognosis. In 2012, the Italian region of Friuli-Venezia Giulia was appointed pilot leader of a European-funded project for ICT-supported integrated care addressed to European frail citizens, to test the viability and evaluate the impact of health and social care integrated services through an extensive deployment program involving 23 European regions. Methods: Cohort, prospective, randomized study with 1:1 intervention vs. usual care ratio (200 total users) Medical sensor devices and environmental sensors all contribute to keeping end-users safely at home. Integrated, real-time access to the platform allows for integration of clinical and social data. Help-desk and Contact Centre staff, provide 24/7 monitoring of alarms, as well as support to adherence and social inclusion. Results: The European project is planned to end as of December 31st, 2015. While final results are pending, focus groups, case studies and qualitative interviews show that Smart Care integrated platform is being perceived as possibly facilitating person-centred supportive care by streamlining services, allowing for updated information sharing, and providing empowerment to patients, families and professionals alike. Comments and conclusion: Integrated ICT-supported care may successfully complement chronic care pathways for complex cardiac patients. However, in-depth quanti/qualitative data analysis will have to be carried out to understand whether the benefits in terms of work overload and economic costs are such as to allow for costly technical and organizational choices. Supportive pathways need to build on actual integrated team work experience and leadership. GPs’ roles, responsibilities and economic incentives need to be clearly defined in order to make integration viable and sustainable in the long run. Nurses may play an important role in the coordination and monitoring of services but workloads and responsibilities require clear definition and assessment. Training and education need to be carefully planned and steadily monitored to maintain retention and support stakeholders’ empowerment. Integrated ICT-supported care should always be utilized within a beehive-integrated person-centred model to enhance the quality of IT-supported health and social care interventions which cannot and should not replace personal and social interactions.
Keywords
Heart failure; End users; Supportive and palliative care; ICT-integrated care; Beehive person-centered model; Stakeholders
Introduction
The burden of complex cardiac care
The future of health and social care sustainability and quality of services has recently become a priority topic on the agenda of many European countries whose national and private systems have to face increasing challenges posed by the steady ageing of their population and the associated burden of complex chronic disease [1]. Heart failure (HF) is a chronic, progressive clinical syndrome characterized by a number of signs and symptoms secondary to abnormal cardiac function [2,3], and it often proves to be challenging to both formal and informal stakeholders, given its unpredictable trajectory and difficult prognosis [4]. More than 26 million people suffer from heart failure throughout the world and over 3.5 million people are newly diagnosed every year in Europe alone [5]. Clinical and social complexity coupled with issues due to frequent associated co-morbidities (COPD, diabetes, renal failure, cognitive impairment, etc.) [6] and prognostic uncertainty [7] make it challenging to attend to patients’ multiple needs and to efficiently plan for support and end-of-life care [8]. As a result, HF patients are less likely to have access to supportive/ palliative care services as compared to those with neoplastic diseases, and are at a higher risk of being hospitalized due to non-cardiac comorbidities [9]. This, notwithstanding the fact that HF is considered to be equivalent to malignant disease both in terms of symptoms and mortality rates [10].
Literature has established that complex chronic healthcare conditions do affect the whole individual and his/her environment to encompass a multifaceted range of physical, psychological, spiritual [11], and social domains [12]. Patients with HF are often acutely aware of their declining status but feel uncomfortable approaching issues concerning their mortality [13]. Clinical professionals rarely delve into the end-of-life aspects of the disease during clinical encounters [14]. This fragmented communication approach often makes it difficult to integrate motivation to enhance self-management with awareness of disease progression and final acceptance of its terminal nature [15]. Moreover, the complexity of the disease and the presence of comorbidities make adherence to therapy a pivotal aspect of self-management behaviours. However, research has shown that therapeutic adherence is a multidimensional concept [16] mediated by several multi-factorial determinants [17] which include physical [18], psychological [19] and social factors [20] connected with the individual, the therapy, and the healthcare organization supporting the patient [21]. Supportive care in HF may benefit from innovative approaches and integration of services and roles. In fact, it may provide patients and formal/informal carers with the opportunity to benefit from steady monitoring of clinical status. This may, in turn, reduce hospitalizations, promote self-management and empowerment while at the same time familiarizes patients and caregivers with the disease and its evolution.
Taking integrated care one step forward
Demographic change, the rising incidence of chronic disease and the still largely unmet needs for more personalized interventions demand a new, integrated approach to health and social care [22]. Over the past few years, a number of national governments, the European Commission and WHO Europe have been striving to promote the implementation of integrated models of health and wellbeing. Integrated care has been defined as “a coherent set of methods and models on the funding, administrative, organizational, service delivery and clinical levels designed to create connectivity, alignment and collaboration within and between the cure and care sectors” [23]. However, even though there is a common understanding that integrated care is about closing gaps between health and social care, it may be necessary to expand both its concept and scope so as to promote an active/interactive role by patients, caregivers and third sector members, too. This exhaustive, synergic approach would make illness (and hence health) everybody’s business, a shared responsibility with no bystanders. Within this beehive person-centred model, interdependence would become the goal and technology the tool to ensure integration and foster self-care, individual well-being and empowerment [24].
Friuli Venezia Giulia (FVG): An Italian Regional Model of Integrated Care
FVG is one of the 20 regions of Italy, and one of five autonomous regions with special statute. It has an area of 7,858 km² and about 1.2 million inhabitants. A natural opening to the sea for many Central European countries, the region is crossed by major transport routes connecting the east and west of southern Europe. As far as healthcare is concerned, FVG has one of the leading cardiac centers in Italy and it has a long-standing experience in outpatient integrated care with state-of-the-art programs to diagnose and treat the full spectrum of heart conditions for all patients, from infants to adults with advanced disease. Hospital and outpatient care is integrated with an active national and international research network, providing patients with access to innovative treatments. Close cross-departmental synergies are also in place (e.g. with diabetology, geriatrics, etc.) to ensure comprehensive efficient care for complex patients and their families. Third-sector is increasingly acquiring specificity of role within a well-rounded holistic people-centered approach [25]. Hospital-to-Community networks are in place allowing for integrated pathways to create synergies among hospital, intermediate facilities, social/healthcare Districts, and outpatient cardiology clinics to provide effective holistic care for elderly and frail patients [26].
Outpatient Usual Care in Friuli Venezia Giulia
Outpatient care in FVG, either upon hospital discharge, or in existing domiciliary setting, is organized within 20 regional Districts. Under our existing system, a chronic patient (e.g. with HF, COPD, diabetes) may be admitted to hospital for worsening of his/her existing condition. The hospital alerts the District through a “home care activation” paper form sent by fax, to plan a “protected discharge”. A district nurse is sent to the hospital within 72 hrs to meet the patient and his/her family and to obtain from hospital staff all the relevant information which will be needed on discharge.
At present, only a partially integrated data collection network system does exist. Patient’s data are being kept on a regional repository (G2 Clinico, Cardionet) which can be accessed both by the hospital and by the District. At the hospital, the district nurse assesses the patient’s clinical and psycho-social needs which will be subsequently shared with the District Case Coordinator (mainly a district nurse, or a SW) and the District’s Elderly Patients’ Assessment Unit – made up of GP, Social Worker (SW), district physician, specialist, psychologist, district nurses, etc.- to activate the relevant healthcare services upon patient’s discharge.
The District Case Coordinator draws up a discharge plan and fills out the ValGraf form - a preliminary multidisciplinary, longitudinal assessment and evaluation form [27]. This paper document is subsequently recorded on the regional electronic recording system.
Third Sector is usually not part of the team at the moment of hospital discharge. It may be activated at a later time by means of phone calls to fulfil those patient’s needs that cannot be met by caregivers.
After discharge and upon arrival at home, follow-up and continuous home care plans are also being activated and scheduled (on nurse’s paper chart). If deemed necessary by the GP/case manager. Contacts will continue to be kept with SWs, family and volunteers. In accordance with GP care plan, the case manager will activate different care providers should unmet or urgent needs arise. Every update to the care plan is recorded on paper only. Readmission to Hospital may be activated on an emergency-basis or upon GP decision.
As defined by the Italian law [28], this integrated care approach is free of charge for the end user, as is hospital care. Given the elevated costs of such interventions, service efficiency and effectiveness needs to be closely monitored. Occasional low complexity interventions (i.e. assessments, counselling, tests, sutures, medications and injections) may take place without the presence of a specific care plan because of user’s inability to autonomously reach care structures. The goal is to activate a relation-based as well as a health- and social-based network of care and support. The interventions to promote self-management and empowerment aim to enhance individual autonomy and self-efficacy and prevent any inappropriate hospitalization and subsequent loss of autonomy and personal well-being [29]. However, heavy reliance on paper-based and on face-to-face or telephone communication, coupled with the presence of different registries, partially blind to each other, makes the whole process heavily fragmented notwithstanding its exhaustiveness and holistic organization. Also, the patient, though being at the center of the care process, does not play an active, empowering role; in fact, integrated interventions largely focus on the illness rather than on the person suffering from such an illness.
SmartCare: European Union ICT-supported Integrated Care for European Citizens
The European Union technology-supported health and social care infrastructures may be powerful tools for promoting change and improving the quality and efficiency of care provided to patients and to their caregivers. In 2012, the Italian region of FVG became pilot leader of Smart Care, a European-funded project for ICT-supported integrated care addressed to European frail citizens, to test the viability and evaluate the impact of health and social care integrated services through an extensive deployment program involving 23 European regions. The goal of the project is multifaceted and involves assessing impact of services, optimizing service provision, generating empirical and practical evidence to enhance integration of health, social and third-sector people-centred care, with a strong focus on independent living and domiciliary care.
In Italy, the Smart Care pilot project involves all Local Health Authorities within FVG and it includes 20 Healthcare Districts. It is a cohort, prospective, randomized study with 1:1 intervention vs usual care ratio (200 total users). Within each group, stratification is being carried out according to short-term (3 months) or long-term (9 months) pathways. FVG’s outpatient usual care will serve as a comparison group for the study’s intervention group. Both organizational and information are identical to the ones currently utilized. However, in order to allow for comparison between the intervention and control arms of the study, a minimum dataset of information is being collected in the control group (user‘s personal database, vital parameters, multidimensional clinical and social history (ValGraf) [27], therapy, questionnaires on QoL (WHOQOL-Bref) [30], empowerment (PAM) [31], difference in organizational aspects and subjective perception of quality of service as a consequence of ICT-based Integrated care (eCCIS) [32].
ValGraf is a validated tool for multidimensional and multidisciplinary geriatric assessment utilized to provide an interdisciplinary evaluation of frail patient’s global status covering all relevant aspects of disability, including psychological status, social functioning and external resources [27].
The WHOQOL-BREF quality of life assessment [30] provides a cross-cultural quality of life assessment on a four domain structure (Physical Health, Psychological, Social Relationships, and Environment). In FVG, it is being interviewer-assisted given the frailty of our patients.
PAM questionnaire [31] was designed to assess the individual’s knowledge, skills and confidence for self-management. The validated tool measures the level of patient engagement in their own healthcare. It is composed by a 13-item scale of questions about personal beliefs, knowledge and confidence for engaging in health-related behaviours. It finally assigns an activation score based on the user’s responses.
eCCIS [32] is a tool developed and utilized assess the impact of European telecare interventions on stakeholders’ population (Common Well [33] and Independent [34] European Projects). The instrument covers ten domains: self-assessed impacts (positive and negative); impacts on the carer (burden, anxiety, ability to care, reassurance, time and resources spent caring); usefulness of the system; management of health status and care; usability of the system; fit with everyday life; satisfaction with telehealthcare staff; service evaluation, willingness-to-pay; overall satisfaction.
Questionnaires are to be collected upon enrolment and at exit time.
Project outcome will be assessed according to difference in number and length of hospitalizations, or admissions to intermediate care or nursing care facilities; difference in planned vs unplanned contacts with healthcare, social care staff, as well as any other informal carers (family members, third sector, etc.); difference in end users’ empowerment; difference in costs according to cost-benefit analysis; difference in organizational aspects relevant to ICT-integrated care interventions.
Statistical analysis of outcomes will be carried out by intention to treat (ITT) methodology (i.e. analysis of the results of an experiment is based on the initial treatment assignment and not on the treatment eventually received).
Inclusion criteria for SmartCare Project participants are as follows: age >50; at least one moderate-to-severe chronic condition (HF, diabetes mellitus, COPD); end users with social needs (social isolation, insufficient or inadequate social, or family support, need for environmental monitoring); signed informed consent. Exclusion criteria will be: inability to take active part in the project due to dementia/mild to severe cognitive impairment as per MMSE<24, mental illness e.g. major depression, legal incapacity; presence of a terminal disease bearing ≤3 months life expectancy; lack/inadequacy of technical/communication support for ICT-platform utilization.
SmartCare New Outpatient Care: ICT-based Short and Long-term Pathways
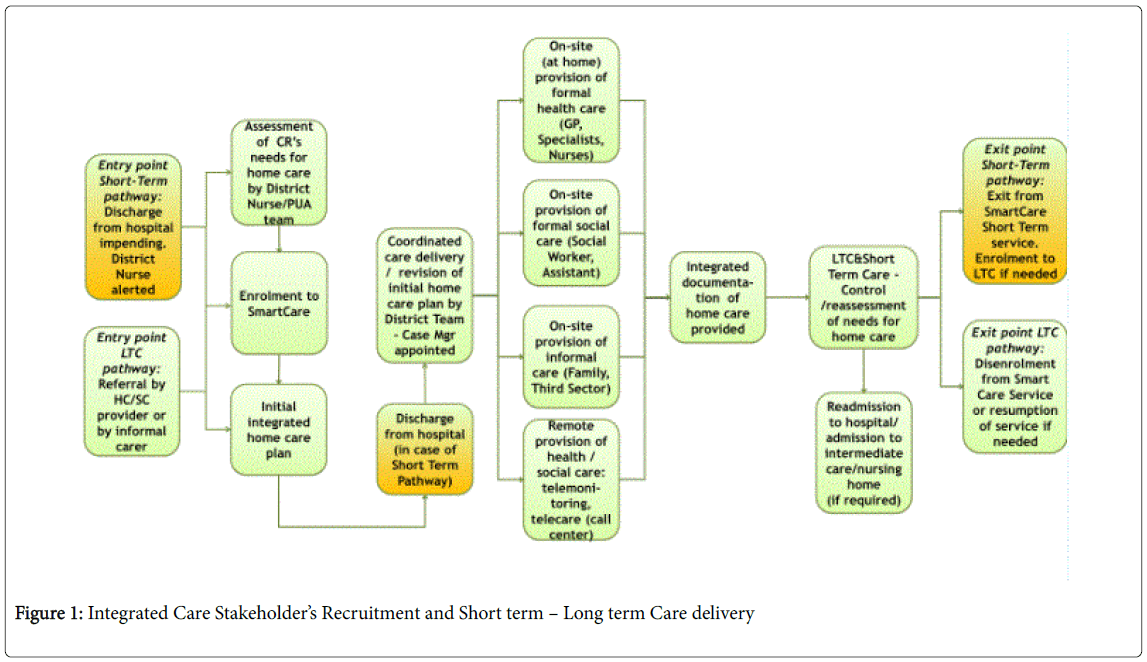
In FVG, two distinct entry points have been identified: the former relates to the Short-Term Pathway (3 months’ activation upon Hospital discharge); the latter is the Long-Term Pathway for frail patients already living at home (9 months). Only entry and exit points differ in either pathway (Figure 1). At present, on hospital entry point for short-term pathways, district nurse will perform a pre-assessment of the hospitalized patient. If the candidate is identified as suitable for SmartCare integrated support, the patient will be asked to sign an enrolment consent form (to be uploaded on the Smartcare platform). At this point, patient’s relevant health and social information will be added to the platform and case manager will provide both patient and caregiver/s with all the basic information about SmartCare and the opportunity to access relevant information directly from home. After randomization, if end user is assigned to intervention arm, the ICT staff will be summoned directly through the platform to set up the devices at the patient’s home (within 7 days from enrolment) while simultaneously training relatives to the use of the platform.
The District nurse will be in charge of completing the assessment by contacting all parties involved within the multidisciplinary team. Subsequently, a Case Coordinator will be appointed among the members of the multidisciplinary team, who will act as the reference person for the home care integrated plan and the ValGraf multidimensional assessment will be uploaded on the SmartCare platform and shared in real time with all the participating actors. This will initiate a tailor-made healthcare integrated plan to be periodically reassessed, adjusted, and shared among the multidisciplinary team members (GPs, nurses, Specialists, Psychologists, SWs, etc.) either via a web-based connection or through portable tablets. The HC recipient and his/her informal care network will also be able to play an active and interactive role with the HC and SC team members by writing journal entries, sending messages, keeping and updated schedule of appointments, etc. Depending on specific clinical and social needs, specific targets and priority care objectives will be defined for every patient (i.e. hemodynamic stability for HF as a clinical target; food delivery, home sensors, etc. as a social target). All integrated Health and Social Care plan are written directly on the platform and made available in real time to all care team members according to pre-defined privileges.
Once a patient has been enrolled, remote monitoring of vital parameters (blood pressure, heart rate, weight, SO2, all defined by standard or individualized thresholds) and of environmental data starts being carried out and made available on a daily basis through external devices sent to the integrated platform. Alarms will be dealt with by the dedicated Call Center and instantly shared on the platform with HC/SC team members. If needed, home visits by health and social carers will be arranged to complete evaluation, or in case of alarms. Should a patient need further hospitalization, a decision will be made by the multidisciplinary team as to temporarily suspend or definitively discontinue SmartCare plan.
Video-conference may be made available if needed. Questionnaires and notes entered by patients, as well as by other formal/informal carers (including Third Sector representatives), have been chosen to enrich the clinical information by providing objective and subjective information as well as a thorough set of outcome measures.
The Help Desk/Call Center is part of the care team activities, and provides a supportive role to the end user’s home care plan providing continuous training and feedback, handling technical problems, adjusting the system to the end users’ changing needs and providing social support, when requested, with scheduled phone calls to check on patient’s adherence and wellbeing.
The Call Center is not responsible for the immediate activation of Healthcare Emergency Number. Should such a need arise, the end user or his/her caregiver will have to promptly and autonomously call an emergency system number. However, after having received a high-emergency alert, the Call Center will nevertheless check the severity of the urgency and activate relevant emergency services, should they not have been already activated.
In the latter case, Call Center staff will access the platform and draw up a summary report of collected data, including alerts, interventions and intervention outcome, and will supply such a report to the hospital team within 48 working hours.
Status of alerts will continue to be updated until return to normalcy status. This continuous monitoring has been designed to gather qualitative/quantitative alert statistics, including mean resolution time or number of successful interventions on alerts.
Alerts automatically produce tickets which allow to measure every step of the alert handling process (Table 1).
| Users / Stakeholders | Role |
|---|---|
| End users (>50, min. 1 moderate-to-severe chronic condition (HF, diabetes mellitus, COPD) | End users (patients) are the main focus and the beneficiaries of the service. At home, they are provided with medical and environmental devices which automatically transmit data to the call center and care team. They can also autonomously communicate through the platform by means of journal entries, or directly to the Help Desk/Call Center staff through a 24/7 active 800 number. |
| End users‘ family members | They play an essential supporting role by monitoring patients’ parameters and meeting their healthcare and social care needs in real time within a predefined scope and to the full extent of their abilities. They have to be allowed to communicate at any given time with the patient’s case manager, or appointed person. They act as end users‘ caregivers. |
| Caregivers (cg) | They play an essential role by helping elderly users to measure those parameters which need to be monitored. If given right of access, they can communicate with healthcare/social care professionals. Oftentimes, such a role is played by the end user’s family members. |
| Third Sector | Volunteers who may either sistematically or from time to time play a supportive role in the end user’s care process. They may be neighbours or members of non-profit organizations, active citizenship’s organizations, etc. |
| Case Manager | The case manager plays an active monitoring and coordination role of the whole end user’s cure and care process. Oftentimes, such a role is being played by a district nurse, but it may be played by a physician (District/GP), or by a social worker. The functions related to such a role may be carried out either within the District or at the end user‘home. |
| Physicians (GPs and specialists)) | They may access the system to provide decision-making support during the course of the disease. They may signal through the system any change in conditions that require intervention. GPs play a pivotal role in the end user’s clinical management and they may act as case managers. District physicians may play a clinical support and coordination role. One or more specialists (cardiologist, diabetologist, pneumologist) may be called to be part of the care team in complex cases. |
| Nurses | They are at the forefront of healthcare interventions. Their goal is to meet end users ‘care needs through domiciliary interventions. A nurse may be appointed as end user’s case manager and become the ‘family’ nurse, acting as a link between the end user, his/her family and the rest of the team. |
| Social workers (SW) | They work for the Municipality and have to provide real time response to the needs signalled by end users. A social worker may be appointed as the end user’s case manager. |
| Staff from the Help Desk/Call Center: | They are in close constant contact with all the stakeholders and play a role in the randomization process, setting up of devices at end user’s home, alarm protocols, providing training and remote support to all the stakeholders involved in the integrated care process. |
Table 1: Project stakeholders.
SmartCare Platform in FVG
The software platform provides an interface between the end user’s home devices and the central database. Its software program sends all data to the central database through standard Web-Services based on secure HTTPS protocols, and its configuration allows tailored setting of the different medical devices according to end user’s specific needs.
A computerized data concentrator allows bidirectional interaction with end user through visual and acoustic signals, messages, memos, reminders and personalised questionnaires [27,30-32]; it also collects and records end user’s clinical and environmental data from various measurement instruments and allows automatic transmission of data to the central healthcare system. In particular, the Hub transmits data received from a number of medical or environmental devices to the central database (eg blood pressure, pulse oximeter, 1-lead ECG, tablet, weight scale, blood glucose monitoring, waist-band for fall detection, Help ME button to request assistance, Z-Wave protocol environmental sensors for motion, temperature, humidity, light, smoke as well as electronic pill box for monitoring patient’s adherence. Fall detection (SmartWalk) is provided by a certified mobility assistive device which measures the end user’s quantity of body motion through 6-minute testing or across the day, as well as his/her accelerations and potential risk for falling. It works as a three-dimensional accelerometer, particularly suited to elderly people and/or people with problems related to balance, or bradykinesia.
The Hub’s purpose is to provide patients with a Home Health station allowing different medical and non-medical devices to provide bidirectional communication by means of Wired or Wireless networks and to connect to the outside world. The integration of home devices with Bluetooth wireless technology allows users to perform monitoring operations unimpeded by wires. Moreover, HC operators may record vital parameters also when patients are physically active.
The platform has been tailor-made according to the needs and requirements which emerged during multidisciplinary meetings and focus groups. The main goal was to make an easy-to-use, readily accessible and scalable integrated platform where every formal/informal stakeholder may play an active role and share real-time information to be recorded and subsequently analysed.
Progress Report
The European project is planned to end as of December 31st, 2015. Final outcome evaluations will focus on the following selected quantitative and qualitative criteria: difference in number and length of hospitalizations; difference in number and length of admissions in intermediate care or nursing care facilities; difference in planned vs. unplanned contacts with healthcare, social care staff; cost-benefit analysis; changes in organizational aspects relevant to ICT-integrated care interventions; end users’ empowerment. FVG is also collecting a number of disease specific health status measures ( i.e. blood pressure, blood glucose, saturation 02, weight, ECG tracing, severity of primary condition) and environmental parameters (e.g. motion in the room, temperature, humidity, light, smoke) together with a large number of clinical and socio-demographic variables including end users’ QoL [30]. While final results are pending, focus groups, case studies and qualitative face-to-face interviews with care recipients, caregivers, as well as health and social care representatives indicate that Smart Care integrated platform is being perceived as possibly facilitating person-centred supportive care by streamlining services, allowing for updated information sharing, and providing empowerment to patients as well as to formal/informal stakeholders. Caregiver’s burden also seems to benefit from added sense of security and perceived closer connection with team members.
In FVG, the eCare project had to be subject to a public tender. Hence, with a view of defining a co-constructed integrated platform, a series of informal meetings was activated to collect stakeholders’ views, needs, and suggestions. Multidisciplinary expert meetings both with potential carers and end-users took place at the outpatient Cardiovascular Center, in Trieste, before arranging focus group activation: the goal was to draw up a grid of specific topics to be addressed in order to identify needs/requirements/critical issues to be met by the Smart Care integrated platform. Questions were asked on previous knowledge of eCare, computer literacy, foreseen barriers, and benefits for the individual and for the care team. Main themes focused on platform accessibility and usability; identification of end-users; data protection; costs and benefits; legal framework; informed consent/privacy; formal and informal stakeholders’ roles and responsibilities; specific needs to be met; training issues; ICT-based requirements and critical issues.
Subsequently, four focus groups were held at local district facilities over a 6-week period to pursue grid saturation. Each group was made up of 10 participants each, representing HC and SC providers (district physicians, district nurses, domiciliary nurses, and municipality social workers) as well as family members and Third Sector representatives. Patients’ views were collected through face-to-face semi-structured interviews carried out either at their domicile since their frail conditions would not allow direct participation in group meetings. Each focus group lasted 1.5 hours and it was led by a trained focus group leader and an observer. The grid of needs/requirements/critical issues was drawn up prior to, and redefined after each focus group so as to allow tailoring the service needs to the healthcare, social and cultural targets.
A shared concern emerging from the meetings was related to platform usability. Being computer literacy low both among professionals and end users, the concerns mainly focused on features to simplify both access and daily usage, to enhance the quality of integrated care and to reduce the risk of drop offs, drop outs and stakeholders’ disempowerment. Formal stakeholders expressed the need for joint training in order to build team connectedness and shared knowledge and to allow each stakeholder to better understand the “big picture” of chronic supportive care so as to provide better overall management. Nurses expressed specific concern about work overload, since the fragmentation of data storage systems in the Region, especially regarding hospital-territory communication, would likely require some double recordings of evaluations. Patients and caregivers both expressed concerns about invasivity of devices, given the fact that elderly people usually live in small apartments. Professionals voiced several specific concerns about privacy issues and data security. On the contrary, despite a few exceptions, most of patients and caregivers expressed relief at knowing that their health information could be finally shared among formal and informal stakeholders. Three multidisciplinary meetings took place at the end point of focus group implementation to summarize and draw up a final list of needs/requirements/critical issues. The platform was subsequently built trying to incorporate the emerging requirements and concerns.
Narrative face-to-face or phone interviews have been carried out throughout the project by a trained interviewer, on a sample of patients, caregivers and HC/SC professionals to explore how technology can support patient care, treatment and rehabilitation and to investigate subjective experience of illness and perception of ICT-based integrated care. Here below, an excerpt from such interviews and case description is provided.
ICT-Integrated Person-Centered Approach: Paul’s Story
Paul is a 63 year old male, living with his wife and two children (10, 17). He has been working for several years as an electronic engineer but had to take early retirement from work due to severe worsening of his health conditions He suffers from Heart Failure (functional class NYHA IV), severe COPD (requiring oxygen-therapy), diabetes and anxiety disorder, besides being severely allergic to a number of medications and environmental factors. He is mostly home-bound because of his illness. He suffers from panic attacks, feels hopeless, and has very low self-confidence and self-esteem. His adherence is very poor. Following upon an episode of acute decompensated HF, Paul is admitted to the local Hospital. After stabilization, discharge procedures start with notification to the District and subsequent visit from a District Nurse who carries out a global pre-assessment (gathering clinical and social information and talking to Paul and his wife). If Paul is deemed eligible for telecare/tele-monitoring services, and he provides his consent, randomization can start. Paul asks questions and is reassured by data security and confidentiality of the platform. After agreeing to being randomized, Paul is eventually assigned to the intervention group A multidisciplinary team assessment is carried out at District level and a case manager is appointed. Paul’s initial home care plan is agreed upon by the District multi-disciplinary team (GP, specialists, healthcare/social care staff, caregiver/s). Assessment information is categorized to give the different members of Paul’s care team their role-based access view. Paul also asks to be given his access key together with his wife, his primary caregiver. Paul does decline volunteer help, but he knows that it may be available, if later needed. Initial home care plan starts and subsequent follow ups will be scheduled according to alerts and Paul’s clinical stability. Paul’s physicians set up individualized alarm thresholds. Data are analysed by the system and progress of Paul’s goal achievement is displayed in the multi parametric diagram. 24/7 Contact Center service starts handling tele-health and telecare alarms. All alerts are being visualized on the same screen page simultaneously.
Multi-disciplinary team has access to updated Shared Care Record including Paul’s new lifestyle goals, tele-health physiological measurement parameters and alert generation as well as environmental monitoring and fall prevention alerts. Paul regularly enters his lifestyle behaviour and tele-health clinical parameters (the latter automatically uploaded through Bluetooth connection) and gradually achieves his initial goals including his home-based cardiac rehabilitation activities. Paul and his informal carers, with appropriate permissions, can view records and make entries in the integrated platform. Self-care and self-management support are supplied to Paul through interactive cognitive/behavioural monitoring and lifestyle/social integration web-based interventions. Patient and informal carers with appropriate permissions can view records and make entries in the integrated platform.
Achievement of lifestyle goals is being displayed and available to relevant stakeholders. Paul is followed up by a trained nurse who revises his lifestyle goals and health status. Paul’s social care needs are regularly assessed by Social Workers. Family caregivers are closely involved in the cure/care process. Paul continues to recover well from his acute cardiac event and is more motivated to look after himself. He is eventually discharged from the Short-Term Hospital Discharge Pathway. The multidisciplinary team assesses Paul’s overall clinical and social situation and jointly decides to enrol Paul in the Long-Term Care Integrated Pathway.
Paul’s perspective
Illness: ‘First I was a man, someone who was not afraid of anything. Then, all of a sudden I became a child again… not a happy child; a scared, vulnerable, weak child. It all started many years ago. BPCO, heart failure, diabetes, allergies, you name it. Several hospitalizations I slowly kept fading away. Now, I often see my wife and my children as if I were in a fish tank. I would like to do more, I would… But in some twisted way I cannot make myself do anything. My body has shut down and so has my mind.’
IT-based integrated care: ‘When the nurse suggested I take part in the project, either in the intervention or control group, at first I was reluctant. I was concerned about privacy, data protection, that sort of things. I was soon reassured; both my nurse and my doctor explained it clearly to me, and I started feeling excited about the potential. Now, I really believe that being enrolled was the best day in a long time, for me. I was a little bit afraid this would raise my anxiety and yet, I wanted to know. Now I feel as if I can at least do something, be active in some way. I don’t feel so passive anymore. I asked the smart Care staff to have me signed in on the platform. Training was easy for me, but I’ve always been working with computers. Taking my weight on a regular basis has always been difficult. I’m very lazy… Now, I get on the scale more easily in the morning and I regularly take my BP. Measurements are automatically sent to the platform, I don’t have to do anything. Now I know that everybody knows and it’s a good feeling. I could ask to be sent pill reminders but I have a very attentive wife and I don’t think I need any further help, for the time being. I guess that being able to keep a watch on you makes it easier to actually do the right things for your life and health. I know I’m very sick; I will never be whole again. However, technology has given me back some of the dignity and self-esteem that the disease had stolen away.’
Caregiver’s perspective (wife)
Illness: ‘My husband has been sick for a very long time and.this thing, this illness is like a monster who everyone is afraid of. It’s heavy and scary. It’s a burden for everybody. You always live with an unwanted guest in your home. I, as his wife, feel a lot of responsibility: it’s not just me and him, it’s the children, Paul’s mother, my parents… I have to take care of too many people, too many emotions. It gets lonely, at times. Every day I wake up thinking something terrible might happen. We never talk about it, Paul is a fighter. However, we all know that we live on borrowed time. This has most affected our children. There is no normal day in our lives; we always feel in an emergency mode. It makes you feel isolated, different from others: an Unidentified Flying Object. It’s lonely, out in space…’.
IT-based integrated care: ‘It may sound silly, but at first I was concerned that people would come in my house and drill holes everywhere to set up bulky devices. Luckily, that was not the case at all. The devices are small and non-intrusive; no holes were needed. They installed temperature, humidity and smoke sensors in the house and provided Paul with a fall detection waistband. All these people working together for Paul and for us, monitoring and making sure he’s ok, well, that’s a great feeling. I signed in to have my name recorded on the platform but I am not using it directly, right now. I don’t have the time to do it. However, I asked to be trained together with Paul so that I know how things do work and what happens should an emergency occur. When the doctor or the nurse come, I feel they already know the whole story and neither Paul nor I need to repeat it all over again. I feel less anxious, as if there were more eyes to watch on Paul at any given time. Everyone, in our situation, should have that kind of support.’
Healthcare professional’s perspective (cardiologist)
Illness: ‘I have known Paul for a very long time, 5 or 6 years at least. He suffers from post-infarction cardiopathy, NYHA-IV heart failure, severe BPCO requiring oxygen therapy, diabetes and multiple severe allergies. Heart failure is a very complex syndrome with a very unpredictable trajectory. It’s very difficult to make a precise prognosis. It worsens, it stabilizes, it worsens again. It’s very delicate and close monitoring is essential to keep the situation under control in order to prevent frequent instabilizations and hospital admissions. Monitoring of clinical parameters and adherence are important. This is a very delicate patient, both from a clinical and a psychological point of view. In usual care, we cannot set alarm thresholds or have readings available; this makes it challenging to prevent acute episodes of instabilization and it may be very time consuming in terms of domiciliary or outpatient visits.’
IT-based integrated care: ‘Paul’s platform-based integrated care treatment plan focuses on symptoms’ control and close monitoring of weight, heart rate, blood pressure and glucose levels to prevent worsening of conditions and subsequent hospitalization. We set personalized alarm thresholds, which can be easily modified, and we, as a care team, are able to share information in real time and to keep a close eye on him. Nurses play an important role in the care of such frail patients and the platform hopefully can help them better organize their work and focus their attention on daily domiciliary interventions to the end users who really need them. It certainly does help physicians like me to provide more effective interventions without waste of precious time. I think the system may be helping all of us in keeping all the variables in check. I don’t know whether this kind of technology can be sustainable for patients as severe as Paul is; however, I do feel that chronic supportive care may benefit from the introduction of technology-based communication and interventions’.
Healthcare professional’s perspective (nurse)
Illness: ‘Paul’s illness and the various comorbidities he suffers from have and still are challenging for us nurses. He is a high risk patient and the responsibility for close monitoring mainly lies on us. We are at the forefront of care for these frail patients, a bridge between patients, physicians, and families as well. Such a high-stress job may lead to burn out. You may feel lonely, at times overwhelmed both with practical tasks and with the emotional toll’.
IT-based integrated care: ‘Thus far, my experience with the platform has been quite satisfactory. There has been the need for double registration of general assessment (Valgraf) given the existence of two separate registries and this has meant extra work for all of us. However, aside from this hurdle, which we all hope can be overcome in the future, the benefits have been plenty. It’s good to know that everybody can check Paul’s status at a glance. Storing data also makes it easier to monitor his conditions and trace back his clinical history. For a nurse, having a tablet to take to the patient’s home is very useful and makes your job easier once you go back to your workplace. There is a schedule for appointments on the platform which I feel can be very useful for everybody. When you are so sick there are many people you need to see; it’s a good thing to have a shared schedule so as not to overlap interventions. I feel that the system can help all of us to work more efficiently and to feel more like a real integrated team. And it’s very good to have active patients and caregivers. It makes work in such a delicate field even more enriching, both as professionals and as human beings’.
Social care professional’s perspective
Illness: ‘Paul’s history dates back to several years ago, unfortunately. He has a severe, terminal illness which has disrupted the whole family, taking a heavy toll on his wife and their children. In fact, we, as a Municipality, have been providing support for his children with after school care and activities’.
ICT-based integrated care: ‘Social care is an integral part of District care interventions. However, communication is not always easy and updated. There are many phone calls, and plenty of paper that can be lost or simply skip somebody’s attention. ICT-based integrated care is providing a common ground where updates to the initial care plan can be shared quickly and with no glitches or risks of misinterpretation. In Paul’s case, after overall assessment, it was decided to set up environmental sensors in his home (temperature, water leaks and smoke detection); a fall sensor was also provided to detect sudden changes in movement and automatically send an alarm to the Call Centre. Video-monitoring was ruled out, since Paul lives in an accessible area of town and does not feel comfortable sharing too much of his private life with carers. Should the situation suddenly change, social services would be immediately alerted and could intervene within a very short period of time to maximize benefits of intervention and minimize burden on end user and his family’.
Comments and Conclusion
While it is too early to draw final conclusions, the initial evidence shows that integrated ICT-supported care may successfully complement complex chronic care pathways by providing tailor-made eCare multidisciplinary home-based interventions for complex cardiac patients. However, an in-depth quanti/qualitative data analysis will have to be carried out to understand whether the benefits in terms of work overload and economic costs are such as to allow for costly technical and organizational choices. Structuring of supportive pathways and tailor-made interventions needs to build on actual integrated team work experience and requires time and leadership: a common vision needs to be shared by physicians (notably GPs), nurses and social care professionals alike. GPs’ roles, responsibilities and economic incentives need to be clearly defined in order to make integration viable and sustainable in the long run. In fact, while participation of nurses and physicians has been satisfactory, many GPs have chosen to play a standby role which would have to turn into more active participation in case of actual large scale implementation of the platform. Nurses may play an important role in the coordination and monitoring of services, but workloads and responsibilities require clear definition and assessment. Training and education of formal and informal stakeholders need to be carefully planned and steadily monitored to maintain retention and support empowerment. Also, while training within the Smart Care Project has been co-led by nurses (together with the technical staff), the question arises whether in the future nurses will be able to bear the burden of patient’s training.
The platform’s flexibility bids well for the future; however, it still remains to be seen whether there will be the willingness and capability to interface it with other systems, devices, and registries to make regional integration complete. Cost-benefit analysis of telecare/telemedicine programs need to be implemented and results shared, because no structural and/or organizational restructuring may be long-lived without economic sustainability. If successful, the project may reconcile the cure and care aspects of clinical and social domains, fostering inter and intra team communication while tightening and strengthening social networks and support. Also, it may further validate and strengthen nurses’ roles in bridging the gap among formal and informal stakeholders through their front line interventions both at clinical and educational level. Given the complicated treatment regimens of HF patients, integrated teams of health and social care professionals should be engaged in collaborative programs, as already happens in oncology [35]. However, technology alone cannot meet the complex, multidimensional needs of frail patients [36]. Hence, integrated ICT-supported care should enhance the subjective and individual quality of IT-supported health and social care interventions which cannot and should not replace personal and social interactions. Persons with long-term conditions, complex clinical and social needs, and terminal illness require simultaneous access to different services. Intra-organisational integration is of paramount importance and each and every stakeholder’s efficiency and effectiveness of service needs to be matched with individual empowerment and wellbeing [24]. Future research needs to focus on training and education of formal and informal stakeholders, within a social learning framework; on-line educational interventions may also prove beneficial and their cost-effectiveness needs to be further investigated. Greater involvement of active citizenship and volunteer mentors should be fostered to disseminate education and knowledge, and to provide economic sustainability with a view to allowing frail citizens with a chronic, terminal condition to live as independently as possible through the provision of sustainable people-centred care. Medical academic institutions are called to provide education on integrated care to prepare future physicians for the rising challenges which require, both ethically and economically, to place the whole person at the centre of medicine and health [37,38].
References
- Wilkinson G, Marmot MG (2003) Social Determinants of Health: The Solid Facts. WHO, Geneva.
- Jessup M, Abraham WT, Casey DE, Feldman AM, Francis GS, et al. (2009) 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation 119: 1977-2016.
- WHO, World Health Organization (2011) Global atlas on cardiovascular disease prevention and control. WHO, Geneva.
- McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, et al. (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33: 1787-1847.
- Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL (2014) Heart failure - Preventing disease and death worldwide. European Society of Cardiology.
- Braunstein JB, Anderson GF, Gerstenblith G, Weller W, Niefeld M (2003) Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure 42: 1226-1233.
- Zapka JG, Moran WP, Goodlin SJ, Knott K (2007) Advanced heart failure: prognosis, uncertainty, and decision making. Congest Heart Fail 13: 268-274.
- Denvir MA, Highet G, Robertson S, Cudmore S, Reid J, et al. (2014) Future Care Planning for patients approaching end-of-life with advanced heart disease: an interview study with patients, carers and healthcare professionals exploring the content, rationale and design of a randomised clinical trial.
- Fradgley EA, Paul CL, Bryant J (2015) A systematic review of barriers to optimal outpatient specialist services for individuals with prevalent chronic diseases: what are the unique and common barriers experienced by patients in high income countries? Int J Equity Health 14: 52.
- Goodlin SJ, Hauptman PJ, Arnold R, Grady K, Hershberger RE, et al. (2004) Consensus statement: Palliative and supportive care in advanced heart failure. J Card Fail 10: 200-209.
- Willems DL, Hak A, Visser F, Van der Wal G (2004) Thoughts of patients with advanced heart failure on dying. Palliat Med 18: 564-572.
- Bunevicius A, Staniute M, Brozaitiene J, Pop VJ, Neverauskas J, et al. (2013) Screening for anxiety disorders in patients with coronary artery disease. Health Qual Life Outcomes 11: 37.
- Quill TE (2000) Perspectives on care at the close of life. Initiating end-of-life discussions with seriously ill patients: addressing the "elephant in the room". JAMA 284: 2502-2507.
- Boyd KJ, Murray SA, Kendall M, Worth A, Frederick Benton T, et al. (2004) Living with advanced heart failure: a prospective, community based study of patients and their carers. Eur J Heart Fail 6: 585-591.
- Fried TR, Bradley EH, O'Leary J (2003) Prognosis communication in serious illness: perceptions of older patients, caregivers, and clinicians. J Am Geriatr Soc 51: 1398-1403.
- Jin J, Sklar GE, Min Sen Oh V, Chuen Li S (2008) Factors affecting therapeutic compliance: A review from the patient's perspective. Ther Clin Risk Manag 4: 269-286.
- (2006) Consensus conference on the management of heart failure. G Ital Cardiol 7: 383-432.
- Gallagher R, Sullivan A, Burke R, Hales S, Gillies G, et al. (2013) Mild cognitive impairment, screening, and patient perceptions in heart failure patients. J Card Fail 19: 641-646.
- Chauvet-Gélinier JC, Trojak B, Vergès-Patois B, Cottin Y, Bonin B (2013) Review on depression and coronary heart disease. Arch Cardiovasc Dis 106: 103-110.
- Compare A, Zarbo C, Manzoni GM, Castelnuovo G, Baldassari E, et al. (2013) Social support, depression, and heart disease: a ten year literature review. Front Psychol 4: 384.
- Sabate E. WHO (2003) Adherence to long term therapies. Evidence for action. Geneva : World Health Organization.
- Meyer I, Muller S, Kubitschke L (2014) Achieving Effective Integrated E-Care Beyond the Silos. Advances in healthcare information systems and administration. Meyer, Mueller, Kubitschke Editors.
- Kodner DL, Spreeuwenberg C (2002) Integrated care: meaning, logic, applications, and implications--a discussion paper. Int J Integr Care 2: e12.
- Stellato K, Humar F, Montesi C, Radini D, Antonione R, Sinagra G, Di Lenarda A (2015) Integrated Outpatient Care in Advanced Heart Failure: the Beehive Person-Centered Model. Int J of Person Centered Med 4: 23-30.
- Theou O, Rockwood K (2015) Frailty in Aging: Biological, Clinical and Social Implications. Karger Publishers.
- Di Lenarda A, Radini D, Stellato K, Humar F, Cherubini A et al. (2014) Hospital-to-Community Integrated Pathways for Heart Failure: Critical aspects and future prospectives. Cardiol Croatica 9: 222.
- Pascazio L, Morosini P, Bembich S, Nardone I, Claricic A et al (2009) Description and validation of a geriatric multidimensional graphical instrument for promoting longitudinal evaluation. Arch of Gerontol and Ger 48: 317-324.
- http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=1300&area=programmazioneSanitariaLea&menu=lea.
- Jerant AF, Azari R, Martinez C, Nesbitt TS (2003) A randomized trial of telenursing to reduce hospitalization for heart failure: patient-centered outcomes and nursing indicators. Home Health Care Serv Q 22: 1-20.
- (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med 28: 551-558.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M (2004) Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 39: 1005-1026.
- Delaney ST, Meyer I, Mueller S (2013) The eCare Client Impact Survey (eCCIS) - Developing a new Tool for assessing Client Impacts of Telehealthcare. Int J of Integr Care 13: 1.
- http://commonwell.eu/commonwell-home/.
- http://www.independent-project.eu/home/.
- Berger A, Shuster J, Von Roenn JH (2007) Principles and Practice of Palliative Care and Supportive Oncology. Lippincott-Raven Publishers.
- Pulignano G, Del Sindaco D, Di Lenarda A, Sinagra G (2006) The evolving care of the elderly with heart failure: from the 'high-tech' to the 'high-touch' approach. J Cardiovasc Med (Hagerstown) 7: 841-846.
- Mezzich JE, Bras M, Dordevic V, Appleyard J (2014) Professional health education and person centered medicine.Int J of Person Centered Med 4: 1-5.
- Goodwin N (2012) Where next for telehealth? Reflections from the 2nd International Congress on Telehealth and Telecare. Int J Integr Care 12: e104.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 17686
- [From(publication date):
September-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 13131
- PDF downloads : 4555