Research Article Open Access
Neurosensorimotor Reflex Integration for Autism: a New TherapyModality Paradigm
Masgutova SK1*, Akhmatova NK2 Sadowska L3, Shackleford P4 and Akhmatov EA2
1Svetlana Masgutova Educational Institute, LLC, Orlando, FL, USA
2I.I. Mechnikov Scientific Research Institute for Vaccines and Serums, Moscow, Russia
3Medical University by Piastow Slaskich, Wroclaw, Poland
4PK Concepts, Melrose, FL, USA
- *Corresponding Author:
- Masgutova SK
Svetlana Masgutova Educational Institute
LLC, Orlando, USA
Tel: +1 (720)544-1166
E-mail: saverkamp@sbcglobal.net
Received Date: July 13, 2016; Accepted Date: September 30, 2016; Published Date: October 07, 2016
Citation: Masgutova SK, Akhmatova NK, Sadowska L, Shackleford P, Akhmatov EA (2016) Neurosensorimotor Reflex Integration for Autism: a New Therapy Modality Paradigm. J Pediatr Neurol Disord 2: 107. doi: 10.4172/2572-5203.1000107
Copyright: © 2016 Masgutova SK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pediatric Neurological Disorders
Abstract
The goal of this research was to evaluate the effect of the Masgutova Neurosensorimotor Reflex Integration (MNRI) therapy modality in improving the behavioral, cognitive, and physical functioning of individuals diagnosed with Autism Spectrum Disorder (ASD). Our research group utilized the MNRI therapy modality based on knowledge of the neurophysiology of reflexes, clinical observations, and studies of reflex pathologies which can be key to improving neurodevelopment in children diagnosed with ASD. The MNRI program uses specific strategies and techniques which access innate natural resources – reflex circuit pathways of the nervous system aimed at supporting maturation within their neuro-sensorymotor patterns. Symptoms of children with ASD are reflected in their lack of sensory-motor integration, poor social interaction and language development, repetitive behaviors and actions, and hyperactive and anxiety disorders. The current study involved three groups: the Study Group of children (n=524) diagnosed with ASD that received the MNRI program, and two control groups that did not receive the MNRI treatment program – Control Group 1: 94 children diagnosed with ASD (total n=618) and Control Group 2: 683 children with neurotypical development. A Reflex Assessment was given to all children before and after the study period. Statistical analysis revealed that a large spectrum of reflex patterns (86.67% or 26 of 30 patterns) were dysfunctional or pathological in children diagnosed with ASD compared to those with neurotypical development [5]. Based on this specific data, the MNRI program utilized techniques and exercises that targeted the restoration of reflex circuit components and protection functions of the children with ASD. A Reflex Assessment completed prior to and after the MNRI intervention (duration – 6 hours daily, 48 hours total) demonstrated a statistically significant (p<0.05) improvement in 83.3% of the reflex patterns of children with ASD in the Study Group. Further qualitative analysis confirms that children in the Study Group also showed improvement in the level of sensory-motor integration, communication, physical and cognitive functioning, particularly, in such areas such as: postural control, motor coordination, balance, tactile sensitivity, behavioral control, state of “presence” and self-awareness, and other abilities and skills, observed by their therapists, parents, and sometimes even themselves. Based on the data from the current study, MNRI intervention appears to have a beneficial effect on children with autism with 80% of the study participants demonstrating improved sensory-motor integration as well as physical, behavioral, emotional, and cognitive development.
Keywords
Hypersensitivity; MNRI; Masgutova; Neurosensorimotor Reflex Integration; Autism; Reflexes
Introduction
Autism Spectrum Disorder (ASD) develops in early childhood. Recent population analysis indicates that the number of cases of ASD is increasing in many countries, particularly in technologically developed countries [1-5]. The U.S. Center for Disease Control research claims that, in some states, one of every 68 children (one of 42 boys) has a diagnosis of the ASD, a 30% increase from 2012 (IACC Strategic Plan for Autism Spectrum Disorder Research, 2013) [6-11].
Some typical characteristics of children diagnosed with ASD are well documented including [1-3,6,9-12]:
• Tactile hypo or hypersensitivity and/or auditory hyper-sensitivity
• Lack of or poor eye contact
• Poor social interaction and language development
• Repetitive behavior
• Alimentary behavior disorders such as a preference for a limited number of foods
• Poorly developed self-defense reactions
• Lack of curiosity about the world around them
• Poor muscle tone
• Gaps in the development of kinesthetic memory and selfconsciousness
• Inability to imitate and follow instructions
• Anxiety disorder.
MNRI research, however, offers a key addition to this list:
• Dysfunctional and pathological reflex system development [13,14].
Reflexes are our genetically determined motor-behavioral patterns that are normally integrated by every child into consciously controlled sensory-motor abilities and skills during early childhood [15-18]. These integrated reflexes then support the neurodevelopment of a child assuring an increase in processing sensory input, programming, and control of motor and behavioral actions, and enhanced learning and memory, language and communication skills.
The basis of MNRI is the utilization of information and clinical experience from neurodevelopment by using reflex patterns to develop sensory-motor integration, cognitive skills, and behavioral and emotional regulation. Multiple dysfunctional reflex patterns are characteristic in two separate groups of children diagnosed with autism: 1) those whose patterns were immature or pathological and severely dysfunctional from birth, and 2) those that developed normally but regressed into autism at age 2 or 3 unexpectedly. Reflexes of these children may have been delayed and immature, but not noted by specialists or parents. Their nerve system, possibly, was not resilient enough to cope with the stress that they experienced. Alternatively, their reflexes might not have matured and have caused the asynchronicity in their brain function development on both cortical and extrapyramidal levels resulting in neurodevelopmental disorders beginning around 2 years of age. An initially mild unrecognized problem can lead to more complicated deficits with age.
Individuals diagnosed with ASD show a chronic lack of sensorymotor integration and delay of skills concerning the early motor milestones [7]. They show a wide range of immature reflex patterns such as Hands Pulling, Hands Supporting, Hands Grasp, Crawling, Asymmetrical Tonic Neck Reflex, Symmetrical Tonic Neck Reflex, Babkin Palmomental, Ocular-Vestibular, and other patterns. The MNRI program utilizes non-invasive intervention to support the development of the neuro-sensory-motor aspects of those reflex patterns through specific techniques and procedures that allow restoration of links between reflex circuit components and the protection function of a reflex [15,16,19-21] to normalize their over-freezing and fight or flight reactions [17,22] seen, for example, in tactile defensiveness or deprivation. Thus, the MNRI program works particularly with the autonomic nervous system – its sympathetic and parasympathetic processes governing the alarm system of the organism described by Selye (1974) in terms of the HPA-stress-axis (hypothalamus, pituitary, adrenal glands).
Over the past 20 years, we have compiled statistical analysis of reflex evaluation results for 3,700 children diagnosed with ASD, which has resulted in the creation of a Reflex Profile for children diagnosed with ASD [5]. This profile has shown that 86.7% of their reflex patterns (26 out of 30 patterns) were dysfunctional/pathological compared to those in children with neurotypical development, and 13.3% (4 out of 30 patterns) were functional, but at a low level -far from the normal range . Previous research has demonstrated that 35% of dysfunctional reflexes cause reflex integration disorder (RID) [5,13,19]. The Reflex Profile for individuals with ASD has shown that RID is characteristic of children diagnosed with autism as a majority of their reflex patterns according the assessment were immature and dysfunctional. Knowledge of the level of an individual’s reflex development and functioning can be an important point in finding an effective strategy of intervention.
The severity of dysfunctions of reflex patterns in children diagnosed with ASD, according to our research, correlates with the level of severity of their ASD symptoms. It also reflects the onset of various challenges such as sensory-motor interaction language skills and intellectual abilities. The manifestations of ASD expressed in reflex patterns immaturity have strong and consistent commonalities but they differ considerably across individuals.
Study Participants
This research project specifically studied 618 children diagnosed with ASD who received an MNRI Reflex Assessment of their 30 reflex patterns. This study focuses on 524 of those, who benefited from MNRI therapy training during the years of 2011-2014. The children who participated all showed symptoms in several important areas: 1) social development delays (poor understanding of family and surrounding social structure, lack of social “presence”, tendency for hyperactive self-protection and aggression), 2) speech and communication deficits (non-verbal, poor expressive and conversational language), and 3) behavioral rituals (repetitive movements and actions, hyperactive jumping/running; being stuck in certain postures), and abnormal habits (injurious behavior to self and others, poor toilette control; inability to adapt to changes in daily routine); 4) poor integration of sensorymotor and reflex patterns (disharmonious work of the tactile system – hyper and hyposensitivity, tactile defensiveness, seeking specific overstimulation; dysfunctional or delayed reflex patterns); 5) lack of motor and postural programming, planning and control; 6) intellectual processing delay (poor prioritizing and selective perception, delay in focusing and widening the attention span, poor mental recall and understanding of cause-result).
Reflex Characteristics of Individuals Diagnosed with ASD
As mentioned, previous research data regarding MNRI Reflex Assessments collected with 3,700 children diagnosed with ASD on 30 separate reflex patterns resulted in showing that all their reflex patterns were globally dysfunctional. According to this data, the average percentage of dysfunctional reflex patterns in the children were: 86.7% (26 out of 30 patterns) in those with severe autism, 73.3% (22 out of 30 patterns) with moderate autism, and 56.7% (17 out of 30 patterns) in those with mild (high functioning) autism. These results indicate an evident correlation with the severity of ASD, presence of the RID in children with ASD, and the declining effect of reflex functioning in their sensorimotor integration and neurodevelopment
Research Groups
This research focused on 618 children with ASD and details the comparative analysis of their improvement in reflex pattern development along with those whose development was neurotypical.
Study Group: The Study Group documented the effect of MNRI training with 524 children with ASD (4 to 19 years old) including 193 females (67 girls of 4-6 years, 71 girls of 7-12 years, and 55 girls of 13-19-year-old age) and 331 males (116 boys of 4-6 years, 103 boys of 7-12 years, and 112 boys aged 13-19). All of these children were grouped according to the level of severity of their disorder based on the main criteria given in their official medical and psychiatric evaluations (ASD Diagnosis DSM-5 DSM-V Social Communication Disorder): ASD Level 1 - Requiring support (mild disorder or high functioning); Level 2 – Requiring substantial support (moderate disorder), Level 3 – Requiring very substantial support (severe disorder) (). Forty-two children were not evaluated for severity of the disorder due to being tested at a young age and other issues (no medical description, no clear test results, or parents did not know this information). Based on observations, specialists working with these children determined their level to be approximately 10 – mild ASD, 19 – moderate ASD, and 13 children – with severe ASD. Thus, the 524 children diagnosed with ASD in total were described as follows: 148 (28.24%) children – mild disorder; 203 (38.74%) – moderate disorder, and 173 (33.02%) children – severe disorder.
In this Study Group of 524 children, each underwent at least one MNRI Conference held during the 2011 and 2014 calendar years. The Family Conferences were organized in Poland in Warsaw; in the USA in San Francisco (CA), Minneapolis (MN), West Palm Beach, St. Petersburg, Fort Lauderdale (FL), and in Canada at Vancouver, B.C. The number of participants in the multiple day conferences was 20-36 individuals. Each participant was given a pre-test Reflex Assessment followed by the MNRI corrective sessions and post-test Reflex Assessment at the conference. Reflex integration sessions were conducted by Core Specialists who have completed professional continuing education courses and clinical hours in MNRI. The sessions included 8 days of treatment: 4 days of intense training on reflex integration, one-day of rest, followed by 4 days of treatment. The sessions included MNRI sub-programs given to the child on an individual one-to-one basis: Dynamic and Postural Reflex Re-patterning, Neurostructural Reflex Integration, NeuroTactile Integration, Oral-Facial Reflex Integration, Visual and Auditory Reflex Integration, Lifelong Reflex Integration, Archetype Movement Integration, and Proprioceptive/Vestibular and Cognitive Skills Development. Caregivers were also given evening group lectures and training workshops.
Control Group 1: Control Group 1 was composed of 94 individuals diagnosed with ASD that did not participate in the MNRI program. Each participant was given a Reflex Assessment pre-test and post-test within the same amount of days as the Family Training Conferences of 9 days. This group (ASD, n=94) was the same age range of 4 to 19 years; 34 females and 60 males and had severity levels as follows: 27 children (28.72%) – mild ASD, 29 (30.85%) children – moderate ASD, 38 (40.43%) children – severe ASD.
Control Group 2: Control Group 2 was composed of 683 individuals having neurotypical development that did not participate in the MNRI therapy training. Each participant was given a Reflex Assessment pretest and post-test within the same time span as the Family Training Conferences of 9 days. Control Group 2 were neurotypical children (aged 4 years to 19 years; 376 females and 307 males without MNRI training).
Institutional Review Board (IRB) research approval was given by the New England IRB (85 Wells Avenue, Suite 107, Newton, MA 02459) (IRB ll-173). :”Ethical approval for this research was also granted by the Health Sciences and Developmental Rehabilitation Department of Medical Academy by Piastow Slaskich (Wroclaw, Poland) and the Mechnikov Scientific Research Institute for Vaccines and Serums (Moscow, Russia). All participants were given alpha numeric digits to protect their anonymity. Consent forms were received from every parent or legal guardian of the children. MNRI Assessments and therapy sessions were conducted by designated MNRI Core Specialists successfully completed the Continuing Professional Education requirements and clinical hours.
Method of Measurement
MNRI Reflex Assessment: Our primary interest was the outcome seen at post-Reflex Assessments which showed improvement in patterns of the children with autism that participated in our study. The results of Reflex Pattern Assessments conducted before (pre-test) and after conferences (post-test) were inspected through comparative analysis. Evaluations of sensory-motor patterns were oriented toward the child’s age and neurologic abnormalities with regard to the normal status of reflexes. Briefly, this entailed grading 30 reflexes (diagnostic qualities/realms coded X1-X30) using five parameters: reflex schema or pattern (or sensorimotor circuit), direction of a motor/postural response, strength or intensity of reaction (or muscle tone regulation), time and dynamic of reaction (latency, length, finishing), and symmetry (of all parameters above) with four features for each. [23] Thus scores were based on a continuous scale of 0-4, with the score ‘4’ indicating a fully functional parameter, and ‘0’ indicating the absence of the parameter (for all five parameters) with a maximum 20 points for each reflex (Table 1). A summary of the varying scores are in Table 1. Reflex patterns were grouped relative to the three planes of the body with ten reflex patterns in each: the sagittal, horizontal, and dorsal planes [5].
| Normal Function | Dysfunction/Pathology | |||||
|---|---|---|---|---|---|---|
| Points | Level of reflex integration | Points | Level of reflex dysfunction | |||
| 20 | Full / Complete integration | 10-11.75 | Marginal pathology and dysfunction | |||
| 18 – 19.75 | Mature and integrated | 8 – 9.75 | Incorrect, light dysfunction | |||
| 16 – 17.75 | Correctly developed – normal | 6 – 7.75 | Dysfunction | |||
| 14 – 15.75 | Functional, but low level of development | 4 – 5.75 | Severe dysfunction | |||
| 12-13.75 | Functional, but very low level of development | 2 – 3.75 | Pathology | |||
| 10-11.75 | Marginal pathology and dysfunction | 0 – 1.75 | Severe pathology | |||
Table 1: Clinical evaluation: criteria for Reflex Assessment scores.
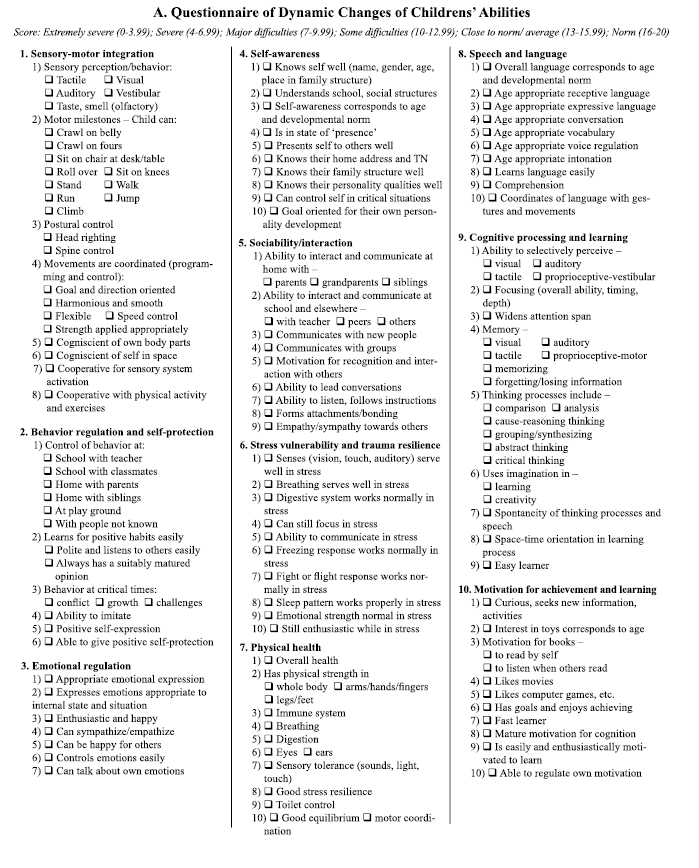
Questionnaire of Dynamic Changes in Children’s Abilities: The evaluation of changes in children’s sensory-motor integration, behavior, communication, personality and cognitive areas completed by parents and specialists before and after the MNRI therapy training was based on analysis of results of the Questionnaire of Dynamic Changes in Children’s Abilities (MNRI QDC; Masgutova, Conference materials, 2010) [See Appendix A]. Its scoring system in points ranged from 0 to 20, in which 0 and 1 was lowest developed features and 20 – normal and very well developed (Table 2). This questionnaire contains 10 clusters of statements reflecting different areas of functioning and life activities of children – among them concerning the features from the criteria for autism spectrum (Diagnostic and Statistical Manual of Mental Disorders; 5th ed.; DSM-5). The areas proposed for evaluation were: 1) sensory-motor coordination and integration; 2) behavior regulation and self-protection, 3) emotional regulation, 4) self-awareness, 5) sociability and interaction, 6) stress vulnerability/resilience, 7) physical health, 8) speech and language, 9) cognitive processes and learning, and 10) motivation for achievement and learning. Parents and specialists working with each child provided daily reports during all eight days of the MNRI training program and one additional summary report as a conclusion of the therapy intervention period. Results of the first and last summarizing reports for each parent and per-four professionals/ child were given (a total 5 reports per child).
| A child’s activity area: Clusters |
Scoring of levels of changes in different activity areas for a child Levels in points 0-12 |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pathological responses (hyper- hypo-sensitive, deprived) | Major difficulties (7-9.99) |
Some difficulties (10-12.99) |
Close to norm/ average (13-15.99) |
Norm (16-20) |
|||||||||||||||||
| Extremely severe(0-3.99) | Severe (4-6.99) |
||||||||||||||||||||
| Points (0-20) | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
| 1. Sensory-motor integration | ---- | ---- | ---- | ---- | ---- | ------ | ---à | 7.2 | |||||||||||||
| ---- | ---- | ---- | ---- | ---- | ------ | ----- | ----- | ----- | ------ | ---à | 11.2 | ||||||||||
Table 2: The example of scoring of children’s abilities for the ‘Sensory-motor integration’ cluster before (pink color scale) and after the MNRI® program (green scale).
Every statement was rated as either: “neurotypical/normal response”, “close to norm/average”, “some difficulties”, “major difficulties”, “pathological response”.
An example of scoring of children’s abilities in different areas by parents and specialists presented below shows the criteria for rating of the ‘Sensory-motor integration’ cluster prior to and after the MNRI program (Table 2).
Statistical Methods
MNRI Reflex Assessment: Results of (total 2602 of assessments examined) Reflex Assessments in children diagnosed with ASD were analyzed based on the multivariable function z = f(x) of non-observable phenomena [24]. This function evaluates the level of the reflex pattern development/integration Z as a function of the reflex patterns X1,X2, ..., X30. Consequently, variable ZS (reflex patterns serving mainly for the sagittal body plane) presents summary information from the first ten reflex patterns X1, X2,…., X10. Variable ZH (horizontal body plane) summarizes the information from the second group of ten reflex patterns X11, X12,.., X20. Variable ZD (dorsal) summarizes the last ten reflex patterns X21, X22,.., X30. The level of the reflex pattern development/integration (ZC) is evaluated by all measured patterns (X1, X2,..., X30). In this study, we determined values of reflex pattern integration by the three body planes and/or one value of the reflex pattern integration level Z for values between 0 and 1 based on a summary of 30 values scored from 0 to 20 for each individual. Mean values of ZC, ZS ZH, and ZD were compared prior to and after 9 days of going through the MNRI program using an ANOVA test created for this type of statistical analysis (IBM SPSS Statistics Grad Pack 22.0). Results were approached as statistically significant at p<0.001 and not significant at p>0.05. The statistical evaluations were also performed by the Mann-Whitney U-test and additionally by statistical (version 6.0; Stat Soft Inc, Tulsa, OK, USA). P values (M ± SD) less than 0.001 in the same way were evaluated as significant at p<0.001 and not significant at p>0.05.
Questionnaire of Dynamic Changes in Children’s Abilities: Statistical analysis of the data of the Questionnaire of Dynamic Changes in Children’s Abilities (MNRI QDC [See Appendix A]) was calculated using the ANOVA test (IBM SPSS Statistics Grad Pack 22.0) in which results were evaluated as statistically significant at p<0.05, and not significant at p>0.05 (Table 3). Also the Mann-Whitney U-test, using Statistica (version 6.0; Stat Soft Inc, Tulsa, OK, USA) was applied, which was interpreting the values (M ± SD) less than p<0.05 as significant and not significant at p>0.05.
| Diagnostic Quality/ Feature | Body Movement Plane | Reflex | Individuals with ASD (n=556) Results before and after the MNRI® Program (in 9 days) |
Individuals with neurotypical development | ||||
|---|---|---|---|---|---|---|---|---|
| Study Group (n=524) |
Control Group 1 (n=94) |
Control Group 2 (n=683) | ||||||
| Pre-test: | Post-test: | Pre-test | Post-Test | Pre-test | Post-test | |||
| X1 | S | Core Tendon Guard | 12.57±0.6 | 13.32±0.8* | 13.27±0.8 | 13.19±0.5 | 15±0.7 | 15±0.9 |
| X2 | S | Robinson Hands Grasp | 9.58±0.5 | 11.21±0.7* | 9.68±0.9 | 9.75±0.7 | 17±0.7 | 17±0.7 |
| X3 | S | Hands Pulling | 8.76±0.5 | 11.26±0.8* | 9.15±0.6 | 8.87±0.7 | 16±0.5 | 16.1±0.8 |
| X4 | S | BabkinPalmomental | 7.97±0.9 | 8.76±0.7 | 8.46±0.7 | 8.55±0.3 | 16±0.8 | 15,8±0.9 |
| X5 | S | Babinski | 7.89±0.6 | 10.12±0.6* | 9.34±0.5 | 9.55±0.9 | 16.±0.8 | 16.5±1.2 |
| X6 | S | Foot Grasp | 8.46±0.4 | 9.83±0.6* | 7.78±0.9 | 8.25±1.2 | 15±0.6 | 15±0.8 |
| X7 | S | Leg Cross Flexion-Extension | 11.87±0.6 | 12.74±0.8 | 12.82±0.5 | 12.67±1.4 | 17±0.9 | 17.1±0.7 |
| X8 | S | Asymmetrical Tonic Neck | 9.19±0.7 | 10.75±0.9 | 9.45±0.4 | 9.38±0.4 | 15±0.7 | 15±0.9 |
| X9 | S | Abdominal Sleep Posture | 7.13±0.4 | 8.84±0.5* | 7.46±0.3 | 7.35±0.5 | 16±1.0 | 16.1±0.9 |
| X10 | S | Bonding | 9.36±0.8 | 10.74±0.4* | 10.22±0.6 | 9.97±0.7 | 15.5±0.7 | 15.5±0.8 |
| X11 | H | Thomas Automatic Gait | 12.23±0.9 | 13.85±0.7* | 12.45±0.5 | 11.98±0.5 | 17,5±0.9 | 17,4±1.3 |
| X12 | H | Bauer Crawling | 8.73±0.7 | 10.87±0.6* | 8.87±0.8 | 9.15±0.7 | 15,5±0.6 | 15,5±0.8 |
| X13 | H | Moro Embrace | 8.78±0.6 | 11.42±0.5* | 9.32±0.7 | 9.25±0.6 | 15,5±0.6 | 15,5±0.8 |
| X14 | H | Fear Paralysis | 8.88±0.4 | 10.65±0.8* | 9.93±0.9 | 9.78±0.4 | 14,5±0.5 | 14,6±0.7 |
| X15 | H | Hands Supporting | 7.87±0.5 | 10.86±0.6* | 8.13±0.4 | 8.31±0.6 | 15,5±0.7 | 15,5±0.9 |
| X16 | H | Segmental Rolling | 7.58±0.7 | 9.42±0.7* | 7.32±0.3 | 7.23±0.9 | 15±0.8 | 15,4±1.2 |
| X17 | H | Landau | 8.64±0.7 | 9.83±0.6 | 6.16±0.6 | 6.27±0.7 | 15±0.8 | 15,1±1.1 |
| X18 | H | Flying and Landing | 9.01±0.5 | 10.66±0.8* | 9.78±0.7 | 9.84±0.5 | 14,5±0.7 | 14,5±0.9 |
| X19 | H | Grounding | 8.94±0.4 | 11.42±0.5* | 9.64±0.6 | 9.81±0.9 | 15,5±0.6 | 15,5±0.8 |
| X20 | H | Head Righting | 9.14±0.5 | 10.92±0.7* | 9.87±0.8 | 10.23±0.4 | 16,5±0.7 | 16,5±1.3 |
| X21 | D | Trunk Extension | 12.46±0.6 | 13.93±0.7* | 12.39±0.6 | 11.96±0.5 | 16±0.7 | 16,2±0.8 |
| X22 | D | Symmetrical Tonic Neck | 8.87±0.5 | 11.14±0.4* | 9.43±0.6 | 9.56±0.7 | 16±0.6 | 15,8±0.9 |
| X23 | D | Spinal Galant | 7.36±0.4 | 9.34±0.6* | 8.34±0.8 | 9.16±0.7 | 15±0.9 | 15±1.2 |
| X24 | D | Spinal Perez | 7.87±0.6 | 10.45±0.7* | 8.76±0.5 | 9.22±0.3 | 16±0.7 | 16,1±1.2 |
| X25 | D | Tonic Labyrinthine | 8.47±0.7 | 10.45±0.4* | 9.22±0.4 | 8.96±0.4 | 16±0.9 | 16,1±1.1 |
| X26 | D | Foot Tendon Guard | 7.46±0.4 | 9.87±0.8* | 8.2±0.7 | 8.4±0.5 | 15,5±0.8 | 15,3±1.2 |
| X27 | D | Spinning | 8.78±0.4 | 10.34±0.9* | 8.23±0.8 | 8.37±0.7 | 15±0.9 | 15,1±1.7 |
| X28 | D | Locomotion | 7.48±0.6 | 8.35±0.8 | 7.63±0.7 | 7.35±0.4 | 14,4±0.4 | 14,5±0.8 |
| X29 | D | Balancing | 8.56±0.8 | 10.89±0.7* | 8.34±0.4 | 8.47±0.4 | 15,7±0.6 | 15,6±1.1 |
| X30 | D | Pavlov Orientation | 9.87±0.7 | 11.78±0.6* | 8.74±0.6 | 8.56±0.8 | 18,5±0.7 | 18,5±0.9 |
| %/patterns | Dysfunctional reflexes (6-9.99 points) | 86.7%/26 | 23.3%/7 | 83.3%/25 | 80%/24 | 0 | 0 | |
| %/patterns | Marginal between dysfunctional & functional state (10-11.99) | 0 | 66.7%/20 | 3.3%/1 | 13.3%/4 | |||
| %/patterns | Functional; very low level of development (12-13.99) | 13.3%/4 | 10%/3 | 13.3%/4 | 6.6%/2 | |||
| %/patterns | Functional but low level of development (14-15.99) | 0 | 0 | 56,6%/17 | 63.3%/19 | |||
| %/patterns | In norm (16-17.99) | 0 | 0 | 43.3%/13 | 36.6%/11 | |||
Table 3: Reflex Profile of Individuals with ASD. Results of Reflex Assessment in Study Group (n=484) compared to individuals with ASD in Control Group 1 (n=72) and with neurotypical development in Control Group 2 (n=683).
Data Analysis
MNRI Reflex Assessment data: The MNRI Reflex Assessment of individuals diagnosed with ASD (n=618) in two groups-Study Group (n=524) and Control Group 1 (n=94), and of Control Group 2 of individuals with neurotypical development (n=683) are presented below (Table 2) showing that dysfunctional reflexes in children diagnosed with ASD were characteristic for both groups: the Study Group demonstrated dysfunctional reflex patterns for 86.67%/26 of assessed reflex patterns and Control Group 1 showed 83.3% of reflexes were dysfunctional, while results in Control Group 2 (children with neurotypical development) show that 100% of their reflex patterns are functional.
Results prior to and after the MNRI program (in 9 days) for the Study Group showed high dynamic changes occurred in the levels of reflex patterns in a rather short period of time-only 26.67% of them were still on a dysfunctional level (vs. 86.67%) and 60 % of the patterns moved to the next higher level to “Marginal, between dysfunctional and functional”, and 13.33% moved to an even higher level of “Functional, very low level of development”. In conclusion, this data shows an improvement of 63.33% reflex patterns of individuals in the Study Group.
Control Groups 1 and 2 that did not participate in MNRI therapy training show no such improvement in reflex patterns, which affirms the positive influence of the MNRI intervention therapy in children of the Study Group showing the need of specialized training for improvement of reflex patterns in cases of the ASD (Table 3).
Table 3 shows the Diagnostic Quality Features (X1-X30) within body and movement planes (S = sagittal; H = horizontal; D = dorsal), levels of reflex development and assessment results before and after participation in MNRI therapy intervention in the Study Group. It also presents the reflex test results of the control groups that did not go through MNRI intervention and were tested a second time, after 9 days. Note: *statistical significance p<0.05.
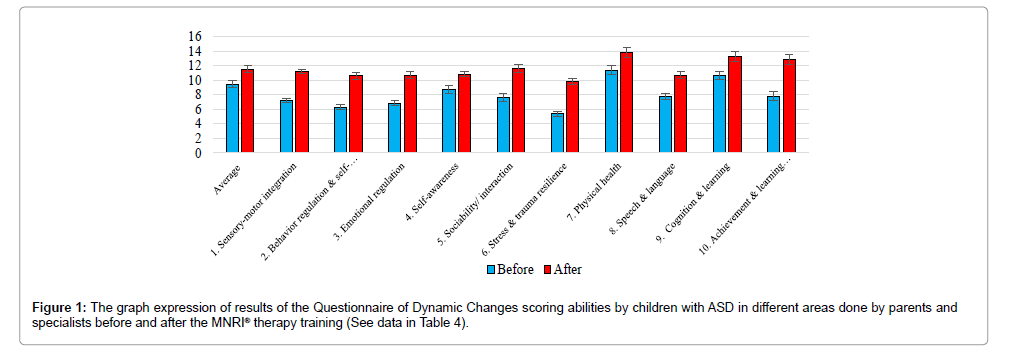
Questionnaire of Dynamic Changes in Children’s Abilities: The data on the Questionnaire of Dynamic Changes [See Appendix A] in children’s sensory-motor integration, behavior, communication, personality, and cognitive areas done before and after the MNRI therapy training also shows corresponding positive changes in all 10 clusters of the Study Group (Table 4). Average score for different areas of activity in the children before the MNRI intervention grew from 7.96 points to 11.52 points after the program (statistical significance p<0.05).
| A child’s activity area: Clusters |
Scoring of levels of changes in different activity areas for children with ASD in Study Group (n=484) before and after the MNRI® intervention. Levels in points 0-12 |
||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pathological responses (hyper- hypo-sensitive, deprived) | Major difficulties (7-9.99) |
Some difficulties (10-12.99) |
Close to norm/ average (13-15.99) |
Norm (16-20) |
|||||||||||||||||
| Extremely severe(0-3.99) | Severe (4-6.99) |
||||||||||||||||||||
| Points (0-20) | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
| 1. Sensory-motor integration | 7.2 | ||||||||||||||||||||
| 11.2 | |||||||||||||||||||||
| 2. Behavior regulation and self-protection | 6.3 | ||||||||||||||||||||
| 10.6 | |||||||||||||||||||||
| 3. Emotional regulation | 6.8 | ||||||||||||||||||||
| 10.7 | |||||||||||||||||||||
| 4. Self-awareness | 8.7 | ||||||||||||||||||||
| 10.8 | |||||||||||||||||||||
| 5. Sociability/ interaction | 7.6 | ||||||||||||||||||||
| 11.6 | |||||||||||||||||||||
| 6. Stress vulnerability and trauma resilience | 5.4 | ||||||||||||||||||||
| 9.8 | |||||||||||||||||||||
| 7. Physical health | 11.4 | ||||||||||||||||||||
| 13.8 | |||||||||||||||||||||
| 8. Speech and language | 7.8 | ||||||||||||||||||||
| 10.7 | |||||||||||||||||||||
| 9. Cognition and learning | 10.6 | ||||||||||||||||||||
| 13.2 | |||||||||||||||||||||
| 10. Achievement and learning motivation | 7.8 | ||||||||||||||||||||
| 12.8 | |||||||||||||||||||||
| Average before MNRI | 7.96 | ||||||||||||||||||||
| Average after MNRI | 11.52 | ||||||||||||||||||||
| Statistical significance | P<0.05 | ||||||||||||||||||||
Table 4: The results of the Questionnaire of Dynamic Changes scoring in children’s sensory-motor integration, behavior, communication, personality, and cognitive areas done by parents and specialists before and after the MNRI® therapy training (in 9 days).
Results
MNRI Reflex Assessment results in Study Group: Initial scores for reflex patterns of children in the Study Group ranged from Dysfunctional (7.13 ± 0.4 points) to Low levels of development (13.93±0.7 points) (Table 2). A significant range of their reflexes - 63.33% or 19 patterns out of 30-showed substantial positive results after completion of MNRI intervention, though not to the level of development of those children with neurotypical development. Five of 30 or 23.33% of reflex patterns of children of this Study Group (the Babkin Palmomental, Leg Cross Flexion-Extension, ATNR, Landau, and Locomotion) did not show statistical significance (Table 3) although positive dynamic and changes were observed specifically in such patterns as: Leg Cross Flexion-Extension, which became more differentiated, better controlled for balancing on one leg and resulted in improvement in the reciprocal manner and regulated speed of walking and running, and Landau and Locomotion which became less rigid for the movement of up and down and towards the horizontal body planes, and improved orientation to sides and overall in space and flexibility.
Control Group 1: Analysis of reflex patterns of children in the Control Group 1 (with a diagnosis of ASD that did not participate in the MNRI training) shows that there was no positive dynamic in their reflex patterns; there was no statistical significance - p>0.05 (Table 4).
Control Group 2: Analysis of reflex patterns of children in Control Group 2 (children with neurotypical development that did not go through MNRI training) reveals that there was no positive dynamics in their reflex pattern; there was no statistical significance -p>0.05 (Table 4).
Questionnaire of Dynamic Changes in Children’s Abilities in the Study Group: Comparative analysis of results of responses by parents and specialists on the Questionnaire of Dynamic Changes in the children’s sensory-motor integration, behavior, communication, and other abilities before and after the MNRI therapy intervention showing overall positive changes in all the areas grouped into 10 clusters still has some significant differences. The progress in some areas was evaluated as much higher after the MNRI intervention, specifically in such areas as: sensory-motor integration (7.2 points grew to 11.2 points), behavior regulation and self-protection (6.3->10.6), emotional regulation (6.8- >10.7), stress resilience (5.4->9.8), achievement and motivation to learn (7.8->12.8). Changes in other areas - physical health (11.4->13.8 points), cognition and learning (10.6->13.2 points), motivation for achievement and learning (7.8->12.8), social interaction (7.6->11.6) performed at the next level. The area of self-awareness (8.7->10.8) was lower/slower, however still statistically significant. Positive changes in children’s abilities in the Study Group (Table 4 and Figure 1) with an average score of 7.96 points before the MNRI intervention and 11.52 points after (statistical significance at P<0.05) validate a strong correlation between positive changes in reflex patterns and improved abilities of children which was observed by parents and professionals and showed on the questionnaires.
Discussion
Children with ASD have a range of accompanying of developmental deficits and disorders such as sensorimotor, emotional-behavioral, language, speech, and communication, so there is an urgency to identify maximally beneficial strategies for supporting development of their functional capabilities [1-5]. MNRI has been developed as a means for assessing and facilitating the neurological function of children with developmental deficits and disorders. [5,13] The MNRI therapeutic facilitation program is oriented toward improving reflex pattern functioning in children with disorders in neurodevelopment which will also be beneficial to their sensorimotor integration, cognitive planning, behavioral regulation and self-control, and emotional growth. This concept has evolved based on clinical results of improved function in children participating at MNRI Family Conferences [5,13]. Further evidence of this concept were positive changes in reflex functioning and its beneficial impact upon fine and gross motor coordination, motor planning, and postural development [25]. Improvement in behavioral regulation also was observed with MNRI training because, with more proper functioning reflexes, children became capable of regulating unconscious, involuntary spontaneous responses, sensorimotor activity, and emotions [26]. Therefore, also cognition can concurrently improve as reported by other authors [27,28].
The Effects of Dysfunctional Reflex Patterns on Children Diagnosed with ASD
Disharmony in muscular system development and lack of regulation for muscle tone beginning in children with ASD in their infancy results in impulsive reactions that often turns into permanent physical characteristics and behaviors as they grow older. For example, impulsivity may lead to poor ability for goal setting, poor focus and following instructions, deficient inner control, hyperactivity, disorganized and chaotic behavior, and irritability and impatience. Lack of muscle tone regulation may later result in challenges in motor programming and control, planning, and thus lead to poor motorcognitive- behavior coordination [19]. This poor regulation is caused by a lack of balance in the excitation and inhibition processes in the reflex circuits, including improper connectivity between alpha and gamma motor neurons. Clinical observations show that the disharmony and lack of proper regulation in muscle tone in children with ASD are seen mainly in:
• Hypertonic muscles in the posterior dorsal plane of the body (along the spinal column - sacrospinalisis, thoracic longus, trapezius) and with the opposite hypotonic abdominal muscles and diaphragm negatively affects development of postural control. The child with ASD, in an attempt to release tension caused by this disproportion of muscle tone in the back and front of their body, may often display reactivity in behavior and impulsive movements triggering balance/equilibrium mechanisms (balancing reflex pattern), resulting in a state of being overstimulated.
• Hypotonic extensors in the back of the neck and upper limbs (bracioradialis, biceps) and muscle tone disharmony in their palms and fingers causing a tendency to keep their arms flexed (a negative effect to the Hands Pulling Reflex). This results in poor dexterity (based on Hands Grasp, Sequential Fingers Opening and Closing, and other patterns).
• Hypertonic muscles in lower limbs (gastrocnemius, soleus, Achilles tendon, quadriceps, hamstrings) resulting in children with ASD often toe walking and incessantly jumping and running.
• Low tonicity of oral-facial muscles which cause a tight jaw and encouraging a lack of jaw mobility. Tight tendons and muscles around the jaw joints inhibit development of chewing, swallowing, and articulation.
• Poor muscle tone regulation in children with ASD also results in a tendency for hyperventilation and shallow breathing, especially at times of stress.
Lack in development of postural control is also a challenge caused by insufficient muscle tone regulation which may be a result of a lack of dopamine and GABA neurotransmitters in the basal ganglia and interneurons of the reflex circuits [29,30]. Children with ASD may have under developed mobility and body structure, causing reduced overall growth (height and weight) due to deficits in growth factor hormone regulation [31]. Poor muscle tone regulation can indirectly cause challenges in information processing on a cognitive level often seen as a tendency to ignore important external stimuli, escaping into their internal world, involving themselves in repetitive interactions with the same stimuli (via over-excitation in basal ganglia centers and sympathetic system) [29]. Lack in muscle tone regulation, slowed physical growth, hyperventilation and shallow breathing, and poor sleep patterns may be some of the reasons for delays in their physical, intellectual, and emotional development.
Postural control problems: Children with ASD habitually lean their torso and head forward. This postural habit shows at over-tight spinal and calf muscles and hypotonia in abdominal and neck muscles. Their gravity center shifts to the front (from the back) disproportionately, causing difficulties in maintaining normal standing equilibrium. The brain, in an attempt to resolve these difficulties, sends an order to tighten and lock the tendons to maintain an upright position. Too much effort to control this posture over-excites the defensive responses of fight or flight, which in turn leads to more impulsive reactions and movements [19].
Motor coordination deficits: A lack of stability in the standing position and in walking patterns is characteristic for children with ASD. Lack of motor coordination within the sagittal (right-left, righting movements), horizontal (rotational, lateral extension-flexion), and dorsal planes (flexion-extension, postural control) cause impulsive or slowed motor activity and awkward movements. Head righting is usually sufficiently developed in children with ASD, still they have challenges with head movements that their repetitive patterns may cause. Rotational movements of their neck are too frequent, rigid, and, in some, the neck muscles are hypotonic with the corresponding motor abilities rather poorly formed. Independently of the challenges of posture and head righting, this dynamic leads to toe walking, running around, and reactive jumping in the same spot. This type of hyperactivity generates other repetitious behaviorisms that additionally increases their tendencies to be either hyperactive or freeze. This disharmony in a child’s excitation and inhibition processes, along with disorganized motor reactivity, must be the focus for specific therapy by professionals and parents. Re-patterning techniques proposed in MNRI programs utilize methodology to help regulate these responses. Participation in such activities as walking, swimming, running, biking, skiing, and weight training are encouraged to also help them gain proper use of their primary motor patterns and reflexes [19]. MNRI specialists observe that fine motor coordination is also affected by poor gross motor coordination. Incorrect regulation of tone in these large muscles means that improved manual dexterity and perception is challenging when working only on the finer muscles of the hands, eyes, and hearing.
Problems in visual and auditory perception systems: The eyes of children diagnosed with ASD show a restless state or lack of mobility and dilated pupils. They usually have a limited, narrow visual span, poor visual attention and focus, and hyperactive peripheral vision. Their eye movements appear to freeze or jump rapidly in saccades. Many children with ASD demonstrate an addictive tendency for computers and cell phones with compulsive repetition of the same image, object, or program, often watching it at a very close range. The child with ASD becomes over-focused, which over-stimulates their vestibular system and static balance. The Pupillary Reflex in these children may become hypersensitive, over-stimulating the sympathetic system, with either over-reactive or hypoactive motor activity. The visual system of children diagnosed with ASD cope poorly with this visual chaos which leads to a visual processing disorder.
Auditory processing and the affected reflexes are usually problematic for children with ASD [32]. The majority have incorrect sound orientation to auditory stimulus, focusing and binaural perception, and sound prioritizing along with an undeveloped ATNR, Stapedius Acoustic, and Auditory Fear Paralysis Reflex patterns. This is why so many children with ASD are hypersensitive to surrounding sounds though many times their objective audiology evaluation shows normal functioning of the auditory nerve [32]. Their auditory system demonstrates the inability to prioritize outstanding and important sound, therefore they simultaneously hear all incoming sound input, which causes an over-excitation of the auditory system and results in associated reactive behaviors. This is why they tend to protect their auditory system by covering their ears to try to reduce troubling external sounds. Other behaviors often observed relating to a hypersensitive auditory response are hitting their own ears, rapidly shaking their head, vocalizing, and head banging. Delays in auditory reflex patterns result in poor auditory processing: sound differentiation, coding/decoding, prioritizing, and auditory analysis. Dysfunctional auditory reflexes are the main reason for delays in articulation, speech, and expressive language often seen in children with ASD.
Delays in reflex development: Over the last 25 years, data collected from research and direct observation of children diagnosed with ASD [5,19] suggests that they have a wide range of non-integrated reflexes presented in every child with ASD in unique specific arrangements of dysfunction or immaturity. Some examples are:
• Tonic Labyrinthine Reflex is usually significantly delayed in children with ASD. This reflex matures in infants normally between 4-5 months of life [5,30]. The delay of this tonic reflex inhibits the formation of other postural (static) and dynamic reflexes such as Symmetrical and Asymmetrical Tonic Neck and Head Righting.
• Head Righting Reflex on an unconditioned level in a typical infant matures between 1½-2 months of life [30]. The delay of this reflex in children with ASD causes dysfunction in the Trunk Extension and ‘head-core-trunk’ coordination.
• Hands Grasp Reflex matures normally by the end of the fourth month in an infant’s life [5,30]. Children with ASD usually demonstrate a noticeable delay shown by their inability to fully close their palm and fingers into a fist and in an incorrect fist position in phase 2 (a complete closing of the palm and fingers) and phase 4 (grasp with a half open palm and fingers called ‘a hanging grasp’) patterns. This type of delay affects negatively their ability to use their hands for survival and protection needed at times of stress. The Hands Grasp Reflex later affects higher levels of manual skills – pincer and tripod grips, which support many fine motor and manual skills. Proficiency in techniques such as handwriting, playing piano, and using tools such as silverware are delayed in these children.
• Hands Pulling Reflex in most infants mature at the end of their second month of life [5,30]. A delay of formation of this reflex leads to confusion in the sequence of ‘elbows-head-core’ flexion, which is the basis for correct development of the biomechanics of future coordination of core flexion and visual convergence, trunk extensionvisual divergence, close-far vision, and also hand-eye coordination. Thus a delay of this pattern negatively affects their ability to focus, divergent and distance vision, and 3-D vision which specifically influences their writing and drawing abilities.
• Asymmetric Tonic Neck Reflex typically integrates at between 6-7 months in an infant’s life [5]. Lack of maturation of this reflex is frequent in children diagnosed with ASD which leads to poor special orientation and later poor development of monaural and binaural auditory perception and processing, leading to overall speech delays.
• Trunk Extension Reflex matures normally between 7-8 months in an infant’s life [5,28,30]. This reflex is usually immature and hyperactive in children with ASD causing a conflict between the hypotonia of their peripheral muscles and hypertonia of their trunk often leading to toe walking. This also negatively affects their cognitive skills, leading to over-focusing on details, limited imagination, and a lack of curiosity. Hyperactive Trunk Extension is expressed in children with ASD by an excessive running behavior, impulsive movements of their head forward or to the sides, and jumping.
• The Crawling Reflex which matures normally at the end of the fourth month in an infant’s life is not integrated in 83% of the children with ASD according to our research [5,30]. Many of these children were early walkers who did not crawl in infancy. Poor development of this reflex pattern in children with ASD leads to a lack of integration in their cross-lateral (reciprocal) gross motor abilities, motor programming, control, and planning, and in their multitasking abilities.
• The Automatic Gait Reflex is seen early prenatally and must mature by the end of the second month of an infant’s life [5,28,29]. In children diagnosed with ASD it is either hyperactive (in most) or hypoactive-hypotonic and leads to a tendency for a passive state (freezing) or constant running.
• The Hands Supporting Reflex that must mature normally by 6 months in an infant’s life is usually poorly developed in children with ASD and then can be corrected only with specific techniques. Underdeveloped Hands Supporting limits the potential for protection of the body on a biomechanical level, specifically, when using their arms to support their body against falling on the ground after losing a stable body position. [5].
• A Bonding response in infants is seen from their first months after birth. Bonding as a behavior trait matures during their first years of life. Almost every child with ASD that we assessed presented signs of inadequate bonding – lack of attachment, tactile and interactivity defensiveness, a tendency for self-isolation, poor imitation, and poor learning of verbal communication. When bonding is immature, there are problems with visual contact, focusing on the face/eyes of their mother and other adults and poor emotional communication, inability to adequately smile, and poor labeling of the objects in their environment [5].
• Moro and Fear Paralysis Reflexes are patterns responsible to provide a protective strategy for the brain. Specifically, the freeze response is activated by too intense sensory stimulation (Fear Paralysis), and the fight or flight response is based on proprioceptive-vestibular stimulation (Moro) when a stable body position is challenged by shaking or falling down. Clinical observations show that in children with ASD these two reflex responses are usually confused (overlapped). This confusion in brain processing leads to lack of differentiation in the functions of sympathetic (excitation) and parasympathetic (inhibition) nervous system resulting in extreme hyperactivity or freezing, an ‘absent’ mental state or indifference, panic attacks, often a tendency for over-protective or aggressive behaviors. When the Moro Reflex is immature it affects their ability to withdraw their core and offers the body insufficient self-protection [5].
• Spinning and Segmental Rolling are reflex patterns that mature by 4 months of life and allow a child to roll over and move across space, rolling by way of crossing the body midline. These patterns train the child’s body to do rotational movements which bring freedom to the horizontal planes of their body via links with the body plane. When these rotational reflex patterns are rigid and delayed in development as often seen in children with ASD they cause a tendency for limited flexibility in gross movements. This happens when the body plane axis affecting movement and posture is utilized more habitually than horizontal rotational moves. This lack of freedom in movements in the horizontal plane results in constant running around, toe walking, excessive jumping, and excitation [5].
• Vestibular-Ocular Reflexes (horizontal and vertical) is responsible for supporting the adjustment of visual images and the resulting vestibular responses and creating stability for the proprioceptive system. This is usually dysfunctional or very poorly developed in many children with ASD. A child with immature visual reflexes presents with a lack of control of their equilibrium, rigidity, poor vestibular-visual coordination, hyper or hypoactive physiological nystagmus, and poor visual-proprioceptive orientation [5].
• Visual Convergence/Divergence Reflexes allow us to bring our eyes together for focusing near and distance. These reflex patterns, often delayed in children with ASD, influence negatively our selective perception, visual focusing, decoding and coding, analysis and, all together, the whole the visual cognition process. A delay of these patterns also results in dysfunction in peripheral vision, gaze, and tracking which in turn leads to a lack of voluntary control in eye mobility, poor ability for structural perception and visual analysis, reading, and visual comprehension [5].
• The Stapedial/Acoustic Reflex and sound prioritizing. The Stapedial Acoustic Reflex is triggered when the eardrum is stimulated by a sharp high frequency sound causing the contraction of the stapedius muscle in the middle ear. Children diagnosed with ASD frequently show a hyperactive Stapedial Reflex resulting in a hypersensitive auditory system which inhibits their ability to decode and prioritize sounds. This inability can cause confusion via their perception of overlapping of sounds causing processing disorders [13,18]. The immaturity of this reflex can lead to protective behaviors such as attempts to ignore or inhibit auditory stimuli to relax the auditory system. Such compensatory behaviors may include covering or hitting the ears, head banging, pushing on their jaw or chin, vocalizing a constant sound, self-stimulation, and talking to themselves [5,7].
• Swallowing and Chewing Reflex patterns in a child with ASD are usually either hypo or hyperactive. Typical hyperventilating and shallow breathing accompanies these patterns. Poorly developed Swallowing and Chewing Reflexes cause difficulties in eating, holding saliva and food in the mouth, eating too much or refusal to eat, digestion, and articulation and speech [7,19]. The Sucking Reflex is not integrated in many children with ASD and this can suppress the integration of the Swallowing and Chewing Reflexes, which may be additionally hindered by low muscle tone in the oral cavity and in tongue muscles.
The MNRI program targets sensory-motor and muscle systems coherence through re-routing, re-education and training of immature reflexes, which helps a child to re-connect with their natural senses, movements, and responses. This kind of training also allows for the correction of any inhibited and hyper- or hypo-active patterns of the child with ASD. Correction or resolving the impulsive and defensive responses, in turn, will positively affect the growth of kinesthetic consciousness, improvement in postural control, and motor programming (Table 5).
| Parameteres of Reflex Patterns-total in % | Parameters of Reflex Patterns – total in % | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensory -Motor Circuit | Direction of Movement |
Intensity | Latency | Symmetry | ||||||||||||
| Norm | Hyper | Hypo | + | - | +/- | Norm | Hyper | Hypo | Norm | Hyper | Hypo | + | - | +/- | ||
| 1 | Upper Limb | 10.2 | 13.3 | 76.5 | 16.3 | 7.5 | 8.7 | 18.6 | 33.3 | 48.1 | 18.5 | 3.4.4 | 47.1 | 2.5 | 91.3 | 6.2 |
| 2 | Tonic | 16.8 | 15.7 | 67.5 | 20.4 | 66.7 | 12.9 | 21.3 | 30.6 | 48.1 | 21.3 | 31 | 47.7 | 5 | 91.7 | 3.3 |
| 3 | Righting | 17.3 | 14.4 | 68.3 | 56.3 | 11.7 | 32 | 20.2 | 30.6 | 49.2 | 20.2 | 30.6 | 49.2 | 7.2 | 88.8 | 4 |
| 4 | Lower limb | 16.8 | 81.3 | 1.9 | 52.1 | 15.8 | 32.1 | 15.8 | 52.1 | 32.1 | 15.8 | 52.1 | 32.1 | 5.6 | 89.8 | 4.6 |
| 5 | Gross motor | 1.5 | 28.3 | 70.2 | 60.4 | 17.9 | 21.7 | 21 | 30.6 | 48.3 | 20 | 31.7 | 48.3 | 6.5 | 90.4 | 3.1 |
| 6 | Oral facaial/visual and auditory | 0.0 | 20.4 | 79.6 | 25 | 47.7 | 27.3 | 22.9 | 47.7 | 29. 4 |
20.4 | 47.7 | 31.9 | 6.9 | 90.2 | 2.9 |
| 7 | Protection and survival | 0.0 | 70.0 | 30.0 | 18.8 | 72.9 | 8.3 | 0.0 | 75 | 25 | 0.0 | 78.7 | 21.3 | 3.1 | 94.6 | 2.3 |
| 8 | Curiosity/cognition supporting | 20.6 | 44.2 | 35.2 | 62.9 | 16.7 | 20.4 | 12 | 26.1 | 61.9 | 12.1 | 40.2 | 47.7 | 5.8 | 90.4 | 3.8 |
| 9 | Emotional stability / maturation supporting | 0.0 | 11 | 89 | 16.5 | 56 | 27.5 | 16.5 | 27.5 | 56 | 15.6 | 28.3 | 56.1 | 5 | 89.4 | 5.6 |
| Average Total: | 9.2 | 33.2 | 57.6 | 36.5 | 42.3 | 21.2 | 16.5 | 39.3 | 44.2 | 16 | 41.6 | 42.4 | 5.3 | 90.7 | 4 | |
Table 5: The parameter of reflex patterns in the Reflex Profile of 556 children with ASD; MNRI® pre-assessment values (in percentages).
Reflex Profiles of Children diagnosed with ASD
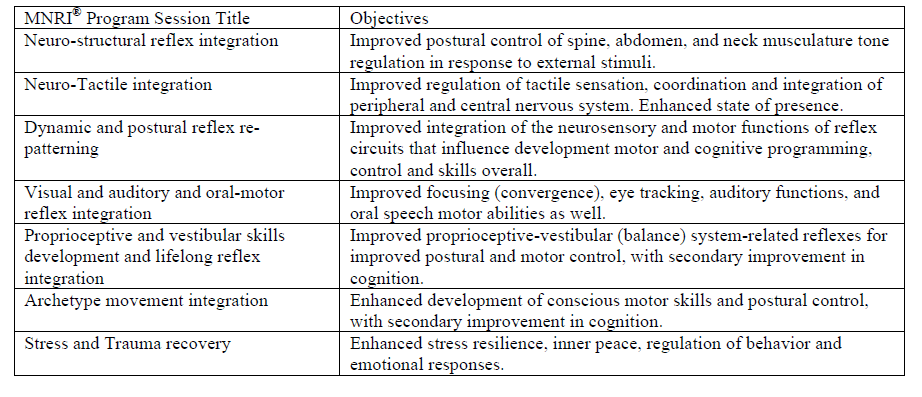
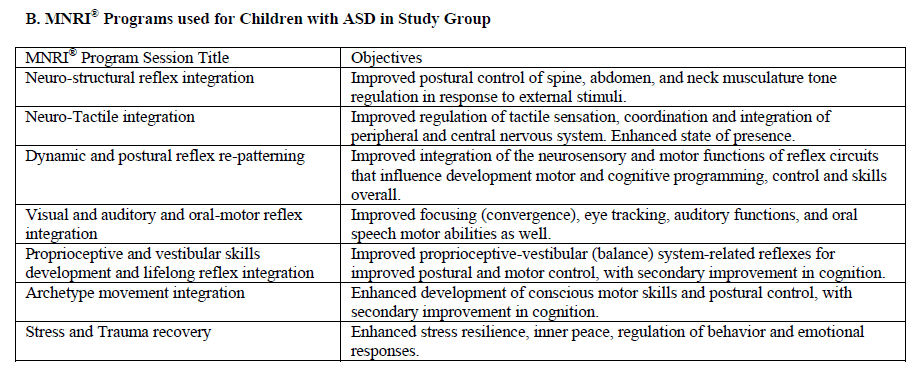
The MNRI Reflex Assessment allows for the creation of a reflex profile for children with ASD and provides the information on the individual differences in their reflex patterns and to use all this to develop an individualized MNRI program. The individualized program targets the correction of disorders in sensory-motor functions of a reflex circuit and neuro-facilitation of reflex parameters to optimize the overall integration of tactile, vestibular, proprioceptive, visual, and auditory systems [See Appendix B].
More detailed analysis of the five parameters of reflexes (within circuit, direction, intensity, symmetry, and timing) has given more data on RID in children diagnosed with ASD. For in-depth analysis, reflex patterns were grouped into nine clusters to highlight tendencies of specific reflexes to influence different areas of functioning of a child with ASD.
In Table 5, the orange colored areas demonstrate outstanding differences and areas of dominance, whereas yellow areas show it to be even with other parameters. This table provides the information for each of the five reflex parameters. Lack of coherence in sensitivity, for example, for upper limb reflexes (Hands Pulling, Hands Grasp, Hands Supporting) which is often hypo may be hyper for the lower limbs (Babinski, Foot Grasp, Foot Tendon Guard). Also many children with ASD demonstrate hyposensitive upper and lower limb reflexes and head righting, which are in dissonance with hypersensitive and hyperactive protective responses, and can be interpreted as poor sensory-motor development that activates even more defense mechanisms since the protection mechanisms are not sufficient. Assessment data concerning the symmetry parameter of reflex patterns is also important because responses for stimuli on left and right side of the body in 100% of all patterns should be asymmetrical. Symmetry is an important indicator in a neurological evaluation of reflex responses. Asymmetry causes asynchronicity in motor aspect reflex response (uneven biomechanics), muscle tone regulation, and speed of response.
Assessment of reflexes within nine clusters according to their effect on sensory and motor systems, behavioral and emotional regulation markers, protective responses, and cognitive functions can help to identify general tendencies of reflex patterns that impact different aspects of an individual’s functioning and well-being. Our long-term clinical observations, Reflex Profile Assessments, and corrective work with children with ASD has led us to hypothesize the neurophysiological causes of RID. Particularly, children with ASD often have:
1) Challenges during neonatal and possibly even prenatal development in the areas of proprioceptive tactility (poor functioning of deep touch, pressure, and stretch receptors), and at infancy when disorientation of differentiation in tactile stimulus from proprioception takes place as a result of incorrect decoding of stimulus by extrapyramidal and higher (cortical) levels of the nerve system.
2) Hypersensitivity in the auditory and/or visual system and also dissonance in functions and coordination of these two systems.
3) Confusion of the decoding system dealing with differentiation between nociceptive and proprioceptive ascending pathways. This type of confusion increases hyper-sensitivity reactivity pushing the brain to interpret neutral stimulus as pain or danger, causing over-protection or the opposite – hyposensitivity, lack of activity, and an inability to protect personal boundaries and one’s own body, and even supports destructive behavior such as self-aggression.
4) Lack of coordination in different components and functions of the reflex circuit: sensory receptors, electrical conductivity in the neurons, neurotransmitter release, possibly also metabolic processes in the cells. For example: This lack of coordination may occur when too many sensory neurotransmitters (substance-P or glutamate) are released as the result of hypersensitivity and too little inhibitory interneuron neurotransmitters are released into gamma motor neurons (GABA and dopamine) [33]. Or, there could be a lack of coherent work between alpha and gamma motor neurons and their connections with muscle fibers (too much or too little acetylcholine neurotransmitters) [29] affecting tone regulation in muscle and the movement biomechanics.
5) Incorrect functioning of the stress-axis (HPA - hypothalamuspituitary gland-adrenals) of the organism caused by past or present acute or chronic stress, or traumatic experience.
MNRI training targeted facilitation and rerouting of poor or nonintegrated reflexes in children with ASD should begin as early as possible so improvements in functions of the automatic and voluntary motor performance can happen more quickly, thus saving them neurodevelopmental time. Because a child with ASD exhibits a multidysfunctional disorder, the therapy program should provide a multidirectional approach based on the individual pathological characteristics and neurodeficits of the child. A priority task of the MNRI modality concerning children with ASD is to facilitate their neurodevelopment, and improve their emotional, social, and cognitive functioning through reflex integration and enhancement of their neuroplasticity. The MNRI program addressing these developmental needs is realized by professionals utilizing such sub-programs as: MNRI Repatterning of Dysfunctional Dynamic and Postural Reflex Integration, MNRI Neuro-Structural Reflex Integration, MNRI Archetype Movement and Lifelong Reflex Integration, MNRI Neuro-Tactile Reflex Integration, MNRI Oral-Facial Reflex Integration, MNRI Birth & Post-Birth Reflex Integration, MNRI Proprioceptive & Cognitive Reflex Integration, and MNRI Visual & Auditory Reflex Integration.
The data above demonstrates that children diagnosed with ASD benefit from early intervention based on MNRI reflex integration processes – early facilitation of their improvement in gross and fine motor coordination, postural control, emotional and behavioral regulation, and language – receptive and expressive speech, thinking and learning skills. MNRI re-patterning exercises address neurodevelopmental mechanisms, resulting in:
1) Physical growth (often in height and weight)
2) Rerouting of natural reflex nervous system pathways and supporting neurophysiological mechanisms of development
3) Reduction in learning stress
4) Enhancement of neuroplasticity as seen in improvement of coordination systems and abilities
5) Increase of the state of presence (being ‘here and now’), motivation, and a more positive attitude
6) Improved quality in motor, emotional, and cognitive abilities.
This study represents an initial step in documenting the efficacy of the reflex integration therapy modality, specifically MNRI, for improving the functioning, quality of life, and learning abilties of children with ASD and other developmental disabilities.
This research has found that many baseline reflexes of ASD participants’ were dysfunctional or pathological, as would be predicted by what is known of ASD. Participants’ summarized results of the reflex assessment (Table 3) showed improvement in ASD children’s sensory-motor and other skills following completion of MNRI training sessions (Table 4, Figure 1). These improvements in reflex pattern functions correspond with the enhancement in motor skills and appear to affect positively also the sensory-motor integration, cognitive, verbal development and language, and communication skills, and decrease in behavioral problems.
A comparative analysis of reflex development data in children in the Study Group (with ASD that participated in the MNRI training) with results of children in Control Group 1 (with ASD that did not have the MNRI treatment) shows that the change in level of reflex patterns development are statistically significant in the Study Group (p<0.05), versus results in Control Group 1, in which the dynamic statistically is not significant (p>0.05) (Table 3). This shows an obvious positive effect of using MNRI with children with ASD.
The similar comparison of results of reflex development of children in the Study Group, Control Group 1 (ASD with no MNRI treatment), and pre- and post-tests in Control Group 2 (neurotypical children with no MNRI treatment) also reveals that the changes took place only in the Study Group, where the MNRI program was applied (Table 3). This confirms that the fact, positive changes in reflex patterns in such short time happens only thanks to the specialized program that was used. Also, it appears that no evident changes occurred, when this type of integrative work was not done, independently if the participant was in the group with developmental deficits or in the group of children with neurotypical functions.
The results of reflex assessment and the dynamics of development of skills in different areas of activity reveal that children in Study Group have benefited from the MNRI techniques significantly. In contrast, in both Control groups, where the children did not have the MNRI treatment, the improvement in reflex patterns and skills did not take place: Control Group 1 (with children with ASD showed changes correspondingly at p>0.05 and p>0.05 for both tests), and in Control Group 2 (with children of neurotypical development; correspondingly at p>0.05 and p>0.05 for both tests). The research data validates the previous clinical observations that dysfunctional reflex patterns to not correct themselves spontaneously. In-depth knowledge of reflexes, evaluation of the level of reflex maturation and its parameters (identifying what aspects are poorly developed or dysfunctional, or pathological) and targeted correction procedures are needed to improve dysfunctional reflex patterns and skills [See Appendix B]. The MNRI method offers techniques and procedures leading to significant improvement in sensorimotor development and overall neurological functioning in children with ASD (which is also noticed in other disorders, such as cerebral palsy and brain damage, Down syndrome, Fragile-X, Prader-Willi syndrome) as measured in Table 4.
Clinical observations of specialists from different helping disciplines (OTs, SPs, PTs, special educators, and psychologists among others) and parents and children’s attendants also note that children with ASD after the MNRI treatment improve their motor programming, planning and control, balance and posture, strength and precision of movements, space-time orientation, speed of perception and response, better presence of mind, easier focusing, improved memorizing, and expressive and/or comprehensive language.
Conclusion
As toddlers, children with ASD skip and have no chance to explore the development of genetically given unconditioned reflexes [5,7,34]. These children may initially grow rather well during the first months and years of their lives. Some develop perceptively well in the areas of gross motor coordination, intelligence, (and may even develop language earlier than their peers). But later parents often report that their children unexpectedly lose these abilities and skills, often after some significant stress. Note: our previous questionnaire addressed to a group of 1600 patents of children with ASD revealed that 86.6% of them stated that their children lost their achieved skills when stress or trauma occurred. In these cases, a global delay in unconditional reflexes and the lack of their progressive development into conditioned reflex patterns were observed. This important detail of the delay in unconditioned reflex patterns is one of the earliest signs of possible risk for ASD. It can be pivotal that reflex integration procedures be offered as early intervention to work with this kind of reflex development delay. The MNRI approach is to use the reflex integration as a tool for children demonstrating developmental challenges, whatever their age. All children with ASD can benefit from the support and rerouting/repatterning correction of sensorimotor patterns and poorly developed or dysfunctional reflexes [7,34].
The MNRI Assessment offers unique information on reflex profiles of children diagnosed with ASD which can serve as data to orient specialists in creating individualized programs for therapy that corresponds with their specific growth challenges. MNRI Reflex Assessments done for children with ASD show that most of their reflex patterns (86.7%) are at a dysfunctional level that, in this model, indicates Reflex Integration Disorder (RID) which is statistically recognized as when 25% of reflex patterns are dysfunctional. MNRI research provides statistically valid data in formulating the hypothesis that RID is an important underlying cause of ASD. Children with ASD show that their dysfunctional reflex patterns count 36% and 64% of very low and low level of development, which can be interpreted as RID being linked to the official diagnosis of ASD.
A comparison of results of improvement in reflex parameters prior to and after the MNRI therapy showed that positive change occurred in: reflex circuit (restoration of sensory-motor links in a reflex circuit), direction (the coordinated work of the motor neurons to create the proper tone and movement), and symmetry in the response. These changes can be explained as a positive achievement in re-patterning or ‘rerouting’ and restoring the reflex pattern and bringing it back to its genetically designed state and function in the nervous system supporting profoundly a tendency towards normal development and integration of all systems. The MNRI program, in other words, ‘teaches and trains’ the brain to improve the functioning of its own sensorymotor links on the level of primary reflex responses (which corresponds to its chronological time of integration within the biomechanics of a reflex pattern, its protective and developmental aspects all together).
This research shows that the level of development of reflex patterns in children with ASD after MNRI therapy modality improved significantly for 86% of assessed reflexes (26 reflex patterns out of 30; the coefficient of change is valid-0.49 before the MNRI program and 0.61 after the intervention at the p<0.001) [35-37]. Statistical analysis of the data demonstrates significant improvement in all reflex patterns evidencing a noteworthy degree of positive benefit of the MNRI program available to children with ASD during 8 days of 6-hour daily intervention. The MNRI treatment opens up the possibility of improved neurodevelopment, learning, creativity, and growth as the unique personalities for children with ASD unfold.
References
- Grzadzinski R, Huerta M, Lord C (2013) DSM-5 and autism spectrum disorders (ASDs): an opportunity for identifying ASD subtypes. Mol Autism. 4: 12.
- Amaral D, Dawson G, Geschwind D (2011). Autism Spectrum Disorders. Oxford University Press. USA.
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, et al. (2008) Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 47: 921-9.
- Van Steensel F, Bögels S, Perrin S (2011) Anxiety Disorders in Children and Adolescents with Autistic Spectrum Disorders: A Meta-Analysis. Clin Child FamPsychol Rev. 14: 302-317.
- Masgutova S, Masgutov D (2015) Reflex Integration Disorder as a New Treatment Paradigm for Children with Autism.In book: Reflexes: Portal to Neurodevelopment and Learning(2015) A Collective Work. SMEI. USA. Pg. 171-180.
- Lemer P (2014) Outsmarting Autism. The Ultimate Guide to Management, Healing, and prevention. World Association Pub, Tarentum, Pennsylvania, USA. Pg. 6-83, 236-266, 275-289.
- Lemer P (2008) Envisioning a bright future. Interventions that work for children and adults with autism spectrum disorders. OEP Foundation. USA Pg. 71-115, 290-296.
- Rutter M, Silberg J (2002) Gene-environment interplay in relation to emotional and behavioral disturbance. Annual Review of Psychology 53: 463-490.
- O’Reilly R, Morlet T, Cushing S (2013) Manual of Pediatric Balance Disorders. San Diego. Plural Publishing Inc. USA.
- Gutstein S (2009)The RDI book. Forging new pathways for autism, Asperger’s and PDD with relationship development intervention program. Connections Center Publishing. Houston. USA.
- RandallP, Parker J (1999) Supporting the families with autism. Chichester. Willey. England.
- Goldstein S, Schwebach A (2004) The comorbidity of Pervasive Developmental Disorder and Attention Deficit Hyperactivity Disorder: results of a retrospective chart review. J Autism DevDisord. 34: 329-39.
- PileckiW, Masgutova S, Kowalewska J, Masgutov D, Akhmatova N, et al. (2012) The impact of rehabilitation carried out using the Masgutovaneurosensorimotor reflex integration method in children with cerebral palsy on the results of brain stem auditory potential examinations. In Advances in Clinical and Experimental Medicine.Official Organ of the Wroclaw Medical University. 3: 21.
- Pilecki W, KipiÅÂ?ski L, Szawrowicz-PeÅÂ?ka T, KaÅÂ?ka D, Masgutova S (2013)Spectral Brain Mapping in Children with Cerebral Palsy Treated by the MasgutovaNeurosensorimotor Reflex Integration Method. Journal of the Neurological Sciences. 333: e550.
- SechenovI (1863-1995) Physiology of behavior. Scientific works-Edd: Moscow. Russia: M. G. Jaroshevsky.
- Perry B (2006) Applying Principles of Neurodevelopment to Clinical Work with Maltreated and Traumatized Children. In book: Working with traumatized youth in child welfare by N. B. Webb. NY: Guilford Press. New York.
- Vygotsky L (1986) The child psychology. The problems of child development. Book - 4. Russia: Pedagogika. Moscow.
- Myles B, Huggins A, RomeLake M, Hagiwara T, Barnhill G, et al. (2003) Written language profile of children and youth with Asperger syndrome: From research to practice. Education and Training in Mental Retardation and Developmental Disabilities 38: 362-369.
- Masgutova S, Akhmatova N, Lebedinskaya O(2013) Clinical-Immunological Assessment of Therapy Effect of the Neuro-Sensory-Motor Integration Program of Reflex Patterns in Airway Chronic Inflammatory Diseases. Event Abstract. International Congress in Milan. Front. Immunol.
- Pavlov IP (1960) Conditioned reflexes: An investigation of the physiological activity of the cerebral cortex. Dover Publications Inc. New York.
- Asratian EA (1983) Selected works. Reflexive theory of high nerve system activity. Science. Pg. 328.
- SelyeH (1974) Stress without distress. JB Lippincott Co. Philadelphia, USA.
- Krefft A (2007) Diagnosis of functions of invisible phenomena (Statistic Mathematic Analysis). PL: Oficyna Wydawnicza Politechniki WrocÅÂ?awskiej. WrocÅÂ?aw.
- Bernstein N (1997) Bio-mechanics and physiology of the movement. Moscow, Russ.
- Bobath K, Bobath B (1984) The neurodevelopmental treatment. In: Scrutton D, editor. Management of the Motor Disorders of Children with Cerebral Palsy. Blackwell Scientific Publications Ltd. UK. Pg. 6-18.
- Montessori M (1995) The absorbent mind. New York. Henry Holt and Company. USA. Pg. 107-110.
- Piaget J (1936) Origins of intelligence in the child. Routledge&Kegan Paul. London.
- Campbell S (2004) Watch me grow! A unique, 3-dimensional, week look at baby’s behavior and development inside the womb. Carroll & Brown Publishers Limited. London, UK.
- Haines D (2002) Fundamental Neuroscience. Edinburgh. Elsevier.
- Melillo R, Leisman G (2004) Neurobehavioral Disorders of Childhood: An Evolutionary Perspective. Springer. USA
- Ningan X, Xiaohong L, Yan Z (2015) Inflammatory cytokines: Potential biomarkers of immunologic dysfunction in Autism Spectrum Disorders. Mediators Inflamm.
- Light L (2015) Auditory Processing Disorders: Why Use MNRI? One Audiologist’s Perspective.In book:Reflexes: Portal to Neurodevelopment and Learning. A Collective Work. Florida. SMEI. p. 68-9.
- Cellot G, Cherubini E (2014) GABAergic signaling as therapeutic target for autism spectrum disorders. Front Pediatr. 2: 70.
- Masgutova S K (2006) Infant reflex integration in movement development. In SK Masgutova, ARegner and MDE Ronin-Walknowska (Eds.). Materials of Polish National Conference: Modern Methods of Stimulation of Movement Development and Learning in Children with Difficulties in Learning, ADHD and Autism. Poland. Pp: 5-28.
- Barashniev J (2001) Prenatal Neurology (Russ). Moscow. Triada-X. p. 640.
- Masgutova S, Akhmatova N, Kiselevsky M (2008) Clinic-immunological assessment of effect of the therapy program of neuro-sensory-motor integration of reflex patterns at chronic inflammatory diseases of respiratory system. Russian Immunology Journal. 2: 454-463.
- Masgutova S, Masgutov D (2015)MNRI Assessment for Determining the Level of Reflex Development. In book: Reflexes: Portal to Neurodevelopment and Learning.(2015). A Collective Work. Florida. p. 201-209.
Appendix A. Questionnaire of Dynamic Changes of Children’s Abilities
Appendix B. MNRI® Programs used for Children with ASD in Study Group
Relevant Topics
- Behavioral Psychology
- Chiari malformation
- Chronic Traumatic Encephalopathy
- Congenital Brain Defects
- Duchenne Muscular Dystrophy
- Epilepsy and Seizures
- Genetic and Metabolic Disorders
- Genetic Epilepsies
- Headaches and Migraines
- Movement Disorders
- Neonatal encephalopathy
- Neurodevelopmental Disorders
- Neurogenetic Disorders
- Neurological Complications of AIDS
- Neuromuscular Disease
- Pediatric Brain Tumour
- Pediatric Sleep Disorders
- Stroke and Perinatal Injuries
Recommended Journals
Article Tools
Article Usage
- Total views: 37452
- [From(publication date):
December-2016 - Mar 29, 2025] - Breakdown by view type
- HTML page views : 35819
- PDF downloads : 1633