Neuromuscular Regulation Problems in Attention Deficit Hyperactivity Disorder Assessed by the Motor Function Neurological Assessment
Received: 26-Jan-2015 / Accepted Date: 23-Mar-2015 / Published Date: 30-Mar-2015 DOI: 10.4172/2165-7025.1000255
Abstract
This article presents an overview of experiences and research on the Motor Function Neurological Assessment (MFNU) used as an assessment tool in connection with ADHD in children and adults. The instrument consists of 16 subtests developed over three decades. The MFNU focuses on specific neuromuscular regulation problems associated with ADHD, especially motor inhibition problems and high muscle tone. The aim of our research projects through the last 15 years has been to investigate possible relationships between attention deficit-hyperactivity disorder (ADHD) symptoms and neuromuscular regulation problems using the MFNU as our research tool. We also have investigated reported pain in adults with ADHD. Each of the studies is previously presented in separate articles and in a doctoral thesis in the period 2009 - 2013. The studies confirm that the MFNU measures a consistent pattern of motor regulation problems in persons with ADHD. The problems seem independent of age, may appear in individuals with little or no dyscoordination or motor skills problems and are rarely seen in individuals without ADHD. Our findings show that children with ADHD typically demonstrate marked improvements in muscular regulation 1-1.5 hours after a single dose of 10 mg Methylphenidate (MPH). The problems reoccur when the MPH is metabolized. The probability of positive effect of central stimulants on the core behavioral symptoms of ADHD seems to increase with increasing problem scores on the MFNU. Our research suggests a close functional relationship between the core symptoms of ADHD and the specific muscular regulation problems assessed by the MFNU. Our research also show that adults with ADHD experience a significantly higher level of pain and more widespread pain compared to non-ADHD controls. This might indicate that pain is a long-term secondary effect of heightened muscle tone and restricted movement associated with the ADHD condition.
Keywords: ADHD; Inhibition; MFNU; Motor skills; Neuromuscular regulation; Pain; Tonus
360685Introduction
The Motor Function Neurological Assessment (MFNU) has been developed by the first author in a period of three decades working with children with motor problems associated with learning and attention difficulties. In this article we shall present a short summary of our experiences and research on the instrument in connection with children and adults with the Attention Deficit Hyperactivity Disorder (ADHD) diagnosis [1].
Previous research has shown that children diagnostized with ADHD often have motor skills problems [2-11]. An overlap of 30- 50% has been reported between ADHD and for Developmental Coordination Disorder (DCD) [12,13]. Pitcher et al. [6] found that 58% of boys diagnosed as ADHD-Inattentive (ADHD-I), 49.1% of boys diagnosed as ADHD-Hyperactive and impulsive (ADHD-H) and 47.3% of those diagnosed as ADHD-Combined (ADHD-C) scored in the upper 15th percentile on the Movement Assessment Battery for Children (MABC) [14]. Children with ADHD have been reported to have impaired handwriting [3,15] and impaired balance [16,17]. Synkinesis (overflow) has also been reported [4]. Kroes et al. [18], using the Maastricht Motor Test, found that qualitative domains of Dynamic Balance, Diadochokinesis and Manual Dexterity and a Total Qualitative Score were significantly associated with ADHD. A high association was also found for problems with Static Balance. The quantitative measures obtained from the test showed no predictive value, though.
The definition of Hyperkinetic Disorder (HKD) in the ICD-10 diagnostic manual [19] states that: “Impairment of cognitive functions is common, and specific delays in motor and language development` are disproportionately frequent”. It was previously believed that motor clumsiness observed in people with ADHD and improvement seen in motor performance with central stimulants was primarily related to inattention and impulsiveness [20]. In the differential diagnoses section for DCD the DSM-IV manual [1] stated that “Individuals with Attention-Deficit-Hyperactivity Disorder may fall, bump into things, or knock things over, but this is usually due to distractibility and impulsiveness, rather than to a motor impairment”. However, it has been repeatedly shown that while inattention and impulsivity may be involved in “ADHD clumsiness”, a real motor impairment is very often involved, especially in fine motor skills [6,21]. Movements in children with ADHD are jerkier and require more time than controls to change the direction of movement [22,23]. Kalff and collaborators [24] found that children at risk for ADHD were generally less accurate and more variable in their movements than children with psychopathology or normal controls. These impairments may not always show up when using standardized motor tests like the MABC [14] and neuropsychological test batteries [25]. In our clinical practice motor impairment were only occasionally observed on such tests. Another clinical experience was that the majority of the tested children typically were described by their parents and teachers as normal or even well-functioning in sports and other bodily demanding activities. Nevertheless, Liv Larsen Stray, the first author of this article, experienced that the same children in everyday activities such as meals, play and school work presented obvious motor deficiencies in activities like handwriting, sitting at the desk, participation in gymnastics, playing with toys and with other children, eating and dressing. In a standard motor test situation Stray [26] discovered that the children would typically show a normal performance in the initial stages of a subtest (and consequently met the success criteria of the test). However, when asked to repeat the movements involved in the same subtests in rapid succession over time the movements would typically get progressively restricted, quirky and staccato, requiring increasingly more effort to maintain. Children without ADHD rarely showed such problems. The motor deficiencies involved were identified partly as problems in muscular inhibition (the ability to release the activated agonist when using the antagonist), and partly as a heightened muscle tone and restricted movement in the muscles of the back. Many of the children appeared “stiff” in their body and gait, and easily got out of breath in physically demanding activities, for instance when jumping or running. Walking and running typically assumed a heavy, thumping and boisterous character when the child was involved in physically demanding play and activities. In the school class, the child would typically “hang” over the desk, continually changing position on the chair or searching positions that required minimal effort. When examined by the physiotherapist the same children would very frequently reveal a very high muscle tone in m. Longissimus, m. Latissimus dorsi, m. Iliopsoas, often seriously limiting movement of the thorax, shoulder and hips, causing restricted breathing. M. Longissimus often “felt like bone” when palpated. A heightened muscle tone and corresponding restrictions of movements were also found in the calf muscles and muscles of the feet. To Stray [27] it seemed that the exaggerated muscle tone might be a way of compensating for difficulties in keeping the trunk in an erect position. Normally the stabilization of the trunk is automatically regulated by the proximal stabilizing muscles of the column. This stabilization, which usually require little effort and attention from the individual, seemed for some reason to be deficient in children with ADHD. As with muscular inhibition problems, the heightened tone was rarely seen in children without ADHD. MFNU was also tried out on adults with ADHD showing results very similar to those seen in children. In addition Liv Larsen Stray and her coworkers observed that the adult patients often complained about tiredness and bodily pain [28].
The frequent lack of significant problem scores on the quantitative part of standard motor tests [29], and the presence of severe motor regulation problems in the same children in clinical and daily life settings suggested that the “ADHD motor problems” might be interpreted as different in nature from the motor skills problems typically involved in DCD. This interpretation was further substantiated by experiences with the introduction of central stimulants in the testing procedures. When examining the children with and without Methylphenidate (MPH) Stray [27] observed that MPH very often gave a parallel improvement in muscular regulation and in the behavioral ADHD symptoms. This effect was usually seen ½ - 1 hour after a dosage of 10 mg MPH was delivered, rapidly subsiding after 3-4 hours, and coinciding with the reoccurrence of the behavioral ADHD symptoms. Stray [27] also repeatedly observed that when the same children were retested with MFNU without medication, even after years of continuous use of MPH, the motor problems had not improved. This pattern was seen in children of both sexes, and over a wide age range. (Examples of the motor changes were filmed and can be found in the DVD accompanying the MFNU manual [30] and in Stray et al. [31]). On the basis of her observations Liv Larsen Stray developed a dedicated test, the Motor Function Neurological Assessment (MFNU), in order to demonstrate and highlight the motor regulation problems to parents and teachers [27]. The test development took place in close collaboration with the second author, both working at a Norwegian State Resource Centre with well-educated and specialized personnel trained within the fields of ADHD, learning and conduct problems. Diagnostic assessment of ADHD was carried out by multi-professional teams including clinical psychologist, test technicians, teachers, social workers, nurse, physicians and physiotherapists [27].
The MFNU – an Overview of Subtests
In the construction of the MFNU Stray [27,30] emphasized test items that tapped what she had identified as the primary qualities of the motor regulation problems in children with ADHD, i.e. problems with muscular inhibition and a high muscle tone.
In the MFNU muscular inhibition is especially seen in the subtests ‘Thumb movement’, ‘Reciprocal coordination’ and ‘Diadochokinesis’ measuring restrictions in the movement of fingers and forearms. (See Table 1 for a list of the MFNU subtests). A restriction of motion is also seen in the subtests ‘Dynamic balance’ where the foot becomes increasingly “stiff’’ and rigid during the repeated jumping series (Table 1).
| Name of sub-tests | Description |
|---|---|
| 01. Dynamic balance-2 legs | Three sideway jumps within marked squares, back and forth. The entire process is repeated three times without stopping. |
| 02. Dynamic balance-1 leg | Three sideway jumps on one leg within marked squares, back and forth. The entire process is repeated three times without stopping. Both legs are tested. |
| 03. Diadochokinesis-right 04. Diadochokinesis-left |
Pronation-supination of one hand, the elbow flexed 90 degrees. The hand is held as an ”extension” of the lower arm. The exercise is performed for approximately 15–20 seconds. |
| 05. Reciprocal coordination | Alternate clenching of one fist and stretching of the other in a rhythmic manner, for about 15 seconds. Fingers should be nearly completely extended after the hand has been clenched. Elbows at a 90-degree angle, palms facing upwards. |
| 06. Thumb movement | The tip of the other fingers are successively touched with the palmar surface of the tip of the thumb. After each opposition, the child extends and abducts the thumb. Both hands are tested for approximately 20 seconds. |
| 07. Throw ball | The tester plays ball with the child. A fairly large ball is used. The child has to throw with dominant arm in an upwards position. Shoulder movement is scored. |
| 08. Catch ball | The tester plays ball with the child. A tennis ball is used. The child has to catch the ball with one hand, fingers flexed, without touching the body. |
| 09. Walking | Walking with toes alternately pointing outwards (“Chaplin”) and inwards, followed by walking on the outer foot rend (Fog's test) and inner foot rend. |
| 10. Lifting arm | Lies prone, arms in a 45-degree angle from midline, lifting one arm with the palm of the hand facing the floor. |
| 11. Lifting leg | Lies prone, spina iliaca anterior is touching the floor while lifting one stretched leg at a time. |
| 12. ”Flying” | Lies prone, the arm in a 45-degree angle from midline, lifting head, arms and legs. |
| 13. Passive abduction-right hip | Lies supine. Tester holds the child's knee and hip in a flexed position. |
| 14. Passive abduction- left hip | The tester stretches and flexes the leg to elicit a relaxation of the hip muscles, and abducts the leg. The sides are evaluated separately. |
| 15. Passive movement-right foot | Lies supine. Tester examines passive movement with dorsal flexion |
| 16. Passive movement-left foot | and eversion/plantar flexion of the right and left foot. |
| 17. Synkinesis | 'Synkinesis' is not a separate test, but an item for the evaluation of synkinetic movements registered in one or more sub-tests. When observed, the tester tries to correct it. The remaining synkinesis after correction is scored. |
Table 1: The sub-tests of the MFNU.
Problems with a high muscular tone are addressed by the subtest ‘Palpation’, which involves examination of m. Longissimus and m. Latissimus dorsi as well as the mobility of the thorax. The muscular tone in m. Latissimus dorsi is also assessed by the subtest ‘Lifting arm’. A high tone in m. Iliopsoas is tested by the ‘Passive abduction hip’ and ‘Lifting leg (left/right)’ subtests. The calf muscle which are active in maintaining and adjusting body alignment [32] are assessed by the subtest ‘Passive movement of the foot (left/right)’.
The remaining tests, ‘Walking’, ‘Catch/Throw ball’ and ‘Flying’ were included in the battery mostly because they often in a dramatic way would show differences in motor performance with/without MPH. The subtests ‘Throw/catch ball’ were eventually excluded from the present MFNU battery in the 2006 issue mostly because of the supposed dependency of acquired motor skills, and that the subtests seemed redundant.
Reliability
As part of a study of 25 boys with ADHD and 27 normal controls a test of internal consistency (Cronbach’s alpha) was performed on the total set of subtests of both groups. An Alpha of .98 was obtained, with no indications of multidimensionality within the subtests [33], making the use of a total sum score (TS) for all individual subtests meaningful.
A study of rater agreement between physiotherapists who had received supervision in the use of MFNU, showed a high to very high agreement (Kappa ranging from .67 to 1.00) [27]. In another study [26] ten videotaped children with and without ADHD being examined on 17 subtests of the MFNU, were separately scored (from video) by nine physiotherapists with limited MFNU experience. An Intraclass Correlation (ICC) of .99 (95% C.I., .98-1.00, p<.001) was obtained on the MFNU Total Score (TS). (ICC was calculated in SPSS, using the Cronbach two ways mixed effects model, consistency option).
Our conclusions were that the MFNU is a highly reliable tool which gives a consistent measure of the construct involved, provided that the test is administered and scored in a standardized way.
A more thorough presentation of the MFNU test with a detailed account of test administration and scoring procedures is given in the User manual [30] and in the doctoral thesis of the first author [26]. The manual is currently available in Norwegian only. A new and updated English version of the manual is in preparation.
A presentation of four empirical studies
Liv Larsen Stray’s clinical findings, and subsequent empirical studies of the motor function problems in ADHD carried out by Stray and her various research teams have been published in four separate articles since 2009, and in her doctoral thesis [26,31,33-35]. The research had three main purposes. The first was to examine in a controlled way to what extent motor regulation problems as measured by the MFNU are present in the ADHD population, compared to people without ADHD. The other aim was to gain insight into the nature of these problems and how they are related to the neurobiological dysfunctions currently assumed to underlie the ADHD condition. The third aim was to examine the possible relationship between motor regulation problems as assessed by the MFNU and development of chronic pain in adults with ADHD. In this article we shall give an overall presentation of this research. For a more extensive and detailed presentation of the specific material, methods, data analyses applied, and the results and discussion of the issues addressed in each study, we refer to the previously published articles.
Study 1: MFNU as an indicator of motor function problems in boys with ADHD: In the first empirical study [33] we wanted to investigate to what extent children with ADHD-C/Hyperkinetic Disorder (HKD) show motor problems, as measured by the MFNU, and how well the test discriminated between children with ADHD and normal controls. We hypothesized that children with ADHD-C/HKD would display consistently high problem scores, and show significantly more motor problems on all the subtests of the MFNU, compared to children without ADHD. 25 drug naive boys, aged 8-12 (mean 10.2 years, SD 1.3), diagnosed with ADHD-C/HKD and full scale IQs within the normal range (mean 97.6, SD 15.6), was compared on the MFNU with a control group consisting of 27 boys aged 8-11 years (mean age 9.5 SD 1.1) without clinically significant ADHD symptoms.
Results: As hypothized motor regulation problems as defined by the MFNU were highly present in the ADHD group, and very rarely seen in children without ADHD symptoms. The median Total Score (TS) was 28 (of maximum 34) for the ADHD group, compared to a TS of 1 for the control group (p<.0001). Effect size (Cohen’s δ) of the TS between the groups was 1.67. Problems on the individual subtests were present in 80.0-96.0%, typically around 90% of the ADHD group. In the control group the corresponding results were 0.0-44.4%, typically 0.0%. (Two “outlier” subjects in the control group presented symptoms of DCD and were subsequently referred to physiotherapy examination after the MFNU trials).
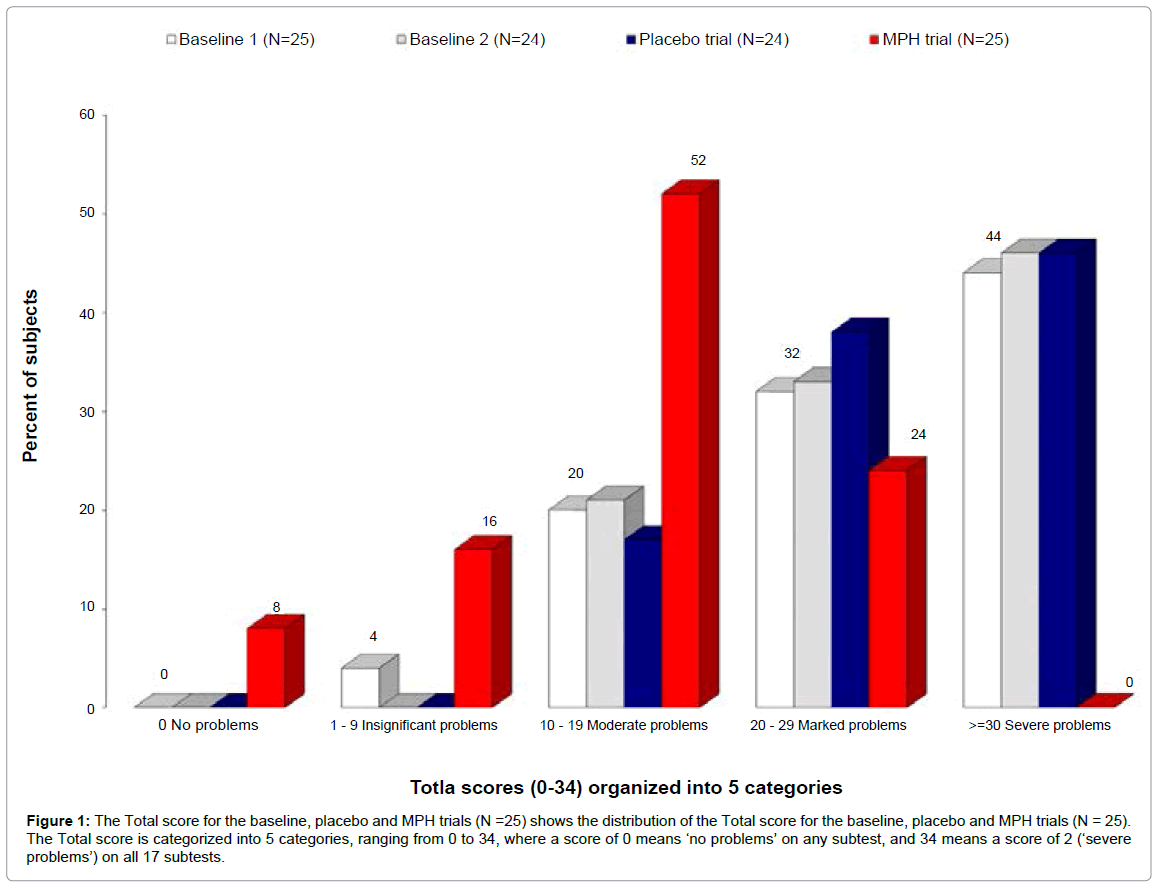
Study 2: Methylphenidate improves motor functions in children diagnosed with hyperkinetic disorder: In the second study [31] we wanted to further investigate the link between a positive MPH response on the behavioral symptoms of ADHD, and improvements in motor regulation. In a pilot study using an early version of MFNU, consisting of 12 subtests, six drug naive children diagnosed with ADHD were assessed without medication (baseline trial) and 90-120 minutes later with 10 mg MPH. All children showed motor problems on most of the sub-tests on the baseline trial and yielded significant improvement on all subtest on the MPH trial [27]. The purpose of the new study was to explore in a more controlled way the possible neurofunctional relationship between motor regulation problems and MPH response, using the MFNU as a test-retest procedure. Our hypothesis was that a single dose of MPH significantly would improve motor function in children with HKD/ADHD-C, on all subtests of the MFNU compared to performance without medication. The study had a double-blind MPH/placebo crossover design using study capsules with a single dose of 10 mg MPH or placebo. The same ADHD group was used as in Study 1. MFNU was performed four times for each subject (two baseline-, plus MPH- and placebo trials (Figure 1).
Results: Improved performance with MPH was registered on all the subtests of the MFNU. The greatest improvements were observed on subtests constructed to measure increased muscle tone. A Cohen’s δ of 1.27 was found when Total Score for the MPH and baseline trials were compared indicating a large effect size [36]. See Figure 1. We also found that the muscular problems returned undiminished when the MPH was metabolized. There were no detected placebo effects. When the subjects were retested without MPH after 3 previous MFNU session no differences in TS scores were found between the baseline and posttest trials. A positive MPH response on the core symptoms of ADHD at home and at school was obtained for 21 of the 23 subjects
Figure 1: The Total score for the baseline, placebo and MPH trials (N =25) shows the distribution of the Total score for the baseline, placebo and MPH trials (N = 25). The Total score is categorized into 5 categories, ranging from 0 to 34, where a score of 0 means ‘no problems’ on any subtest, and 34 means a score of 2 (‘severe problems’) on all 17 subtests.
Study 3: Motor function and methylphenidate effect in children with ADHD: The purpose of the third study [34] was to further examine the relationship between scores on the MFNU and response to MPH on the core ADHD problems. Our hypothesis was that positive MPH responders would obtain more severe problem scores on the MFNU than non-responders. MFNU profiles of 73 drug naive children and adolescents with ADHD (62 boys and 11 girls, age 5-17 years) diagnosed over a 6 year period (1990-96) were examined. All the children were diagnosed with ADHD independently of the MFNU testing. They were subsequently evaluated for effect of MPH for the core symptoms of ADHD (inattention, hyperactivity and impulsivity). On the basis of the registered MPH response they were retrospectively divided into two groups, medicine responders (MR-group) and non medicine responders (NMR-group), and compared on results on the MFNU. There were no significant age or gender differences between the groups.
Results: As hypothesized the results showed that the high methylphenidate responders (MR-group) had significantly higher problems scores on the MFNU than the low-responders (NMR-group).
Study 4: Motor regulation problems and pain in adults with ADHD: In a fourth controlled study [35] we wanted to investigate to what extent adults with ADHD exhibit the same motor functional problems as demonstrated in children and adolescents with ADHD. We also wanted to examine to what extent bodily pain, reported by many children and adults patients with ADHD, could be associated with a high MFNU problem score. Our hypothesis was that adults with ADHD would display higher problem scores on all of the MNFU subtests compared to non-ADHD controls. We also hypothesized that adults with ADHD would report more widespread pain and higher levels of pain than adults in the non-ADHD control group. The study was carried out on 25 MPH-responsive adults with an ADHD diagnosis, both genders, age 20-51 years (mean 33 years, SD 8.9). The MFNU results of the ADHD group were compared to a control group of 23 subjects, age 24-64 years (mean 41 years, SD 14.1) without ADHD diagnosis. The MFNU tester was blinded to the subject’s group adherence. Instruments measuring reported pain were applied in addition to MFNU (Pain Drawing procedure and Numerical Pain Rating Scale).
Results: As hypothesized the ADHD group showed significantly more motor problems than the control group, with a median Total Score of 25 (mean 21.20, SD=9.5), against 2 in control group (mean 6.30, SD=9.9) (p<.001). Cohen’s δ was 1.52. There were no significant gender differences in either of the groups. Most subjects in the control group had no problems on the MFNU. Significant differences were found on all except one of the 16 subtests (‘Flying’). In the ADHD group 84.0-96.0% showed problems on muscle tone subtests. Less problems were registered on the ‘Synkinesis’, ‘Walking’ and ‘Dynamic balance, 2 legs’ subtests (60%, 56% and 56% respectively). The Pain Drawing procedure and Numerical Pain Rating Scale showed stronger and more widespread pain in the ADHD group than in the control group (p<.001). In the ADHD group 80.0% reported widespread pain, against 17.4% in the control group. Only 8.0% of the ADHD group was without reported pain, compared to 34.8% in the control group.
Discussion
Our studies suggest that motor regulation problems, as measured by the MFNU, are highly represented in the ADHD population in general, and virtually non-present in people without ADHD. The problems are found across gender and age, and seem to be most highly represented in individuals with a positive response to central stimulants on the core problems of ADHD. The high incidence of reported pain in adults with ADHD, shown in our fourth study, might suggest that that long term effects of muscular regulation problems, especially the demonstrated heightened muscular tone, are at least partly involved in the development of chronic pain in these individuals.
The results of our first study indicate that problems related to motor functions are more frequent in the ADHD population than hitherto assumed. Our research suggests that the motor problems most typically seen in ADHD may not primarily be accounted for by comorbid deficiencies in motor skills (DCD), nor inattention/distraction or behavioral disinhibition, as has been believed for the last decades. While inattention, lack of motivation and noncompliance might affect the results on the MFNU in some cases, it is highly unlikely that such factors can account for the test scores in any significant ways. In the design and testing procedures of the MFNU several measures are taken to deal with attentional and motivational issues [30]. The tasks are fairly simple to perform, i.e. requiring little motor skills or concentration. All subtests that involve a task performed by the test subject include a guided training period until the tester is ensured that the child knows what to do. The special testing procedure applied, and a scoring system that is based on a qualitative evaluation of performance and movement, would generally rule out possible error sources related to distraction or noncompliance [26]. The tasks performed by the subjects neither put a heavy demand on self-regulatory skills like planning, sustained attention and vigilance often involved in motor skills tasks [11].
It is more likely that motor skills- and dyscoordination problems might influence the MFNU results, particularly in the ‘Synkinesis’ and ‘Walking’, ‘Dynamic balance’ and the ball subtests, perhaps also the ‘Flying’ test. Many of the other tests will also need certain basic motor and coordination skills in order to be performed in a correct way (e.g. the ‘Diadochokinesis’, ‘Reciprocal coordination’ and ‘Thumb movement’). Other subtests though, like ‘Lifting arm/leg’, ‘Palpation’, ‘Passive movement of hips’ and ‘Passive movement of foot’ involve basically no motor skills. The very high incidence of problem scores in people with ADHD on the MFNU therefore seems best accounted for by our suggestion that there are specific motor regulatory deficiencies associated with ADHD, and that these deficiencies might be functionally related to the root causes of the ADHD condition itself. Such a possible functional relationship between the behavioral symptoms of ADHD and motor regulation problems is substantiated by the results of our second and third study which investigated the possible effects of MHP on motor regulation problems as measured by the MFNU. The results clearly demonstrate a very parallel effect of MPH on the behavioral symptoms of ADHD and on the muscular regulation problems measured by the MFNU. Improvements were seen on all subtests, and the problems reoccurred when the medicine was metabolized, as did the behavioral symtoms. There were also no observed training effects of repeated MFNU sessions, which is parallel to the often observed lack of effects of training on attention and self control in individuals with ADHD.
The results of the third study further substantiate the possible link between the presence of motor regulation problems and the neurofunctional processes that are positively affected by MPH in people with ADHD. More research is needed in order to corroborate these findings and to fully understand the possible neurobiological processes involved [26]. However, the results point at unresolved issues related to current diagnostic practice and to the possible inconsistencies in the concept of ‘ADHD’. Are the current diagnostic criteria, exclusively based on behavioral symptoms, effective in the differentiation between possible subtypes of the condition? [37,38]. And might a lack of motor regulation problems in cases meeting the behavioral criteria of ADHD be an indicator of other clinical conditions than ADHD? Udal et al. [17] for instance found that children diagnosed with bipolar disorder, scored significantly lower than the ADHD subjects on the MFNU. It is highly probable that ambiguities in the present diagnostic criteria and differences in diagnostic practice might lead to ADHD diagnoses with quite varied etiologies, many of which may have little neurodevelopmentally in common with the typical positive MPH responder with a high MFNU score.
On the other hand a positive MPH response cannot be used as an indicator of ADHD. It has been shown that central stimulants may have a positive effect on areas that might not be directly involved with ADHD [39,40]. It is also conceivable that MPH might have a direct effect on motor skills problems involved in DCD that are functionally independent of ADHD. Improvements with MPH on motor skills in ADHD with comorbid DCD have been shown in several studies [11,41- 43]. In a review of recent research on this issue Kaiser et al. [11] found that the proportion of children with ADHD who improved their motor skills to the normal range by using medication varied from 28% to 67% between studies. The great variability of the results may indicate that the testing methods used are more or less sensitive to possible specific facets of motor functional problems involved in the MPH response. As mentioned such specific facets need not be deficiencies in motor skills as such. No known studies besides ours have for instance addressed the specific motor regulation problems identified by the MFNU in relation to effects of central stimulants. It is therefore hard to tell from traditional studies of ADHD with comorbid DCD which facets of motor functions that improve with MPH and which do not. Fox et al. [44] found improvements with MPH on motor tasks in individuals with ADHD with no known comorbidity with DCD. They observed that the ADHD subjects had no problems learning the basic skills involved in the tasks and in retaining these skills on later repetition of the tests. However it was also observed that the performance speed was significantly reduced without MPH independent of the skills acquired compared to control subjects. This study confirms our own observations, in that people with ADHD may be highly skilled in activities involving motor control and coordination, for instance sports, but still reveal problems in the regulation of muscular inhibition and muscle tone when tested with the MFNU. What is suggested from our studies is that the MFNU adresses specific problems involved with the neuromuscular regulation of movement, not primarily motor skills. Our finding that MPH seems to specifically address these facets of motor function give support to a hypothesis that muscular inhibition problems and a heightened muscular tone might represent integral aspects of the ADHD condition itself, i.e. that muscular regulation problems are expressions of ADHD at a neuromuscular level, and as such may be seen as physical markers of the condition. More research is needed, however, to determine whether the specific problems addressed by the MFNU are exclusive to the ADHD condition, or might be present in other neurodevelopmental disorders as well.
As hypothesized, the adult ADHD group participating in our fourth study, reported significantly more widespread pain (both in the upper and lower body) and a higher pain level than the control group. Little research has been done in this area. Kessler et al. [45] found that workers with ADHD have significantly more chronic pain than other workers. It is also reported that people with ADHD often have diagnoses such as fibromyalgia or chronic fatigue [46]. It is presently unclear what might account for the heightened levels of reported pain in individuals with ADHD. Treister et al. [47] demonstrated that ADHD subjects had a heightened sensitivity to pain compared to normal controls, and also showed a significantly increase in pain threshold and tolerance with MPH. The researchers suggest that the high pain sensitivity might be associated with the low dopaminergic activity reported in ADHD, and that the regulatory effect of MPH on this activity may explain the changes in pain sensitivity with MPH. Our own research points at similar connections between dopaminergic activity and motor regulatory functions [34]. Seen in this perspective it is not improbable that development of chronic pain, and possibly also fatigue, may be related to the long-term consequence of prolonged muscular tensions, restricted movements and breath, and ineffective use of energy demonstrated in people with ADHD through the MFNU. Further research validation with different methods is needed to conclude on this issue, however.
Limitations
The subjects included in our two first studies were carefully selected to identify a well-defined HKD/ ADHD C sample, excluding subjects with conduct disorder, depressive or anxiety disorder, Asperger or Tourettes syndrome, known epilepsy or other ADHD conditions (ADHD-predominantly inattentive or hyperactive/impulsive type). This would imply that our conclusions from the two first studies cannot be generalized to the broader ADHD population as defined by the DSM-manual. However clinical experience and our findings in Study 3 and 4 clearly suggest that people with less defined ADHD symptoms, independent of gender and age, show the same muscular patterns, and very frequently also responds positively to MPH on the MFNU. These observations open for the possibility that high MFNU scores (and accompanying positive MPH response) are not exclusive to ADHD, but might also be found in other related neurodevelopmental conditions [48-50]. Such conditions might for instance be dysregulation of affect [51] or disorders of hypersensitivity and perceptual modulation, perhaps also Tourettes syndrome, certain autistic conditions [52-55], prematurity, fetal alcohol effects (FAE), or even post-traumatic stress condition or attachment disorders. The presently limited knowledge of the incidence of MFNU-problems in other clinical populations than ADHD prohibits a diagnostic use of the instrument. Further research into these issues might possibly change this picture.
For a further discussion of other possible limitations of our results and conclusions we refer to the individual articles and to the doctoral thesis.
Practical Implications
Throughout the last decades, we have repeatedly observed that the use of MFNU can have a profound effect on parents’ and teachers’ perception of the child when they are given the opportunity to take part in the assessment sessions, and subsequently are given an explanation of how the child’s every day functioning is affected by the muscular regulation problems revealed by the test. Preconceptions of the child as stubborn, undisciplined or lazy will then typically change into a new and more supportive understanding where the child is seen as struggling with real functional problems [56]. This psychoeducative use of the MFNU was, and still is the main purpose of the test. However, as shown in this article, the test has other possible applications. Today the MFNU is commonly used by physiotherapists and physicians within the Norwegian local health care system and in many psychiatric health care institutions for children [57-61]. At present the instrument is increasingly applied as a supplementary tool in the diagnosis of ADHD, and some places also as a part of the testing procedures in the evaluation of effects of central stimulants. Because of the high inter-tester reliability and fairly simple administration and scoring procedures (when administered by trained physiotherapist or physicians) the MFNU has proven suitable also as a research tool.
The MFNU cannot be used diagnostically as a standalone tool, but may be of value as a screening instrument in the pre-referral phase in cases where the person shows significant symptoms of impulsivity, restlessness or inattention. It might also be useful in the evaluation of chronic pain in patients with a prior history of poor concentration, emotional or behavioral dysregulation.
Our research indicates that the impairments involved in muscle regulation problems seen on the MFNU seem hard to alleviate through training. People with ADHD may have been medicated for years and still have the same motor regulation problems when taken off the medicine. This does not necessarily mean that motor skills training is useless or that people with ADHD cannot learn to master the motor challenges involved in daily activities. A high problem score on MFNU may imply though that these skills must be trained in alternative ways to circumvent and compensate for the deficiencies in muscular regulation. Experience from working with patients with ADHD has shown that stretching of the m. Erector spinae, m. Latissimus dorsi, m. Iliopsoas and muscles in the leg and foot usually gives an immediate subjective feeling of alleviation both of muscular tension and of pain. Intensive stability training using slings has been effective for some children with ADHD [57]. Yoga and certain martial arts like Taekwon- Do are often subjectively reported to have effect, though needing daily repetitions. Horse riding with the right guidance has also been reported to be a way to handle the “stiffness” generated by the high muscle tone in gross movement muscles [61]. Further exploration of these and other possible ways of dealing with the muscle regulation problems in ADHD is needed.
Conclusion
While many children with ADHD display DCD problems our experience is that the typical motor difficulties observed in children with ADHD in daily activities are different from ordinary motor skills and dyscoordination impairments uncovered by standardized motor tests. The term ‘muscular regulation problems’ used in this article emphasizes that the impairments measured by the MFNU is conceptually closer to the self-regulation problems believed to be central to the ADHD-condition, than to the motor skills problems defined by the DCD diagnosis. A possible functional relationship between the behavioral symptoms of ADHD and muscular regulation problems measured by the MFNU is substantiated by the results of our research on the effects of MPH on MFNU performance. The marked improvements in both core ADHD behavior and MFNU-score, and subsequent reversal of symptoms when the medication is metabolized, give support to a hypothesis that muscular inhibition problems and a heightened muscular tone represent integral features of the ADHD condition itself, with little relations to motor skills problems. Seen in this perspective it is also quite possible that much of the perceived discomfort and bodily pain demonstrated in our study on adults with ADHD, might be understood as secondary effects of such neuromuscular aspects of the ADHD condition. Further research both with broader samples of ADHD, and with other clinical groups without ADHD-symptoms, is needed to clarify the exact relationships in these matters, however.
Acknowledgements
We are grateful to Sorlandet Hospital, Norway, to Sørlandet Resource Centre, Kristiansand, Norway, the University of Stavanger, Norway, the Regional academic community for autism, ADHD, Tourettes syndrome and narcolepsy and Helse Sorost, Norway for support and funding of the studies referred to in this article.
References
- APA (2000) Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association.
- Piek JP, Pitcher TM, Hay DA (1999) Motor coordination and kinaesthesis in boys with attention deficit-hyperactivity disorder. Dev Med Child Neurol 41: 159-165.
- Tseng MH, Henderson A, Chow SM, Yao G (2004) Relationship between motor proficiency, attention, impulse, and activity in children with ADHD. Dev Med Child Neurol 46: 381-388.
- Denckla MB, Rudel RG (1978) Anomalies of motor development in hyperactive boys. Ann Neurol 3: 231-233.
- Sergeant JA, Piek JP, Oosterlaan J (2006) ADHD and DCD: a relationship in need of research. Hum MovSci 25: 76-89.
- Pitcher TM, Piek JP, Hay DA (2003) Fine and gross motor ability in males with ADHD. Dev Med Child Neurol 45: 525-535.
- Meyer A, Sagvolden T (2006) Fine motor skills in South African children with symptoms of ADHD: influence of subtype, gender, age, and hand dominance. Behav Brain Funct 2: 33.
- Iversen S (2006) Children with developmental problems and disorders: selected aspects of motor and multidisciplinary assessment and intervention in Faculty of Medicine University of Bergen: Bergen.
- Harvey WJ, Reid G (2003) Attention deficit/hyperactivity disorder: a review of re search on movement skill performance of and physical fitness. Adapt PhysActiv Q 20: 1-25.
- Brossard-Racine M, Shevell M, Snider L, Belanger SA, Majnemer A (2012) Motor skills of children newly diagnosed with Attention Deficit Hyperactivity Disorder prior to and following treatment with stimulant medication. Res DevDisabil 33: 2080-2087.
- Kaiser ML, Schoemaker MM, Albaret JM, Geuze RH4 (2014) What is the evidence of impaired motor skills and motor control among children with attention deficit hyperactivity disorder (ADHD)? Systematic review of the literature. Res DevDisabil 36C: 338-357.
- Kadesjö B, Gillberg C (1998) Attention deficits and clumsiness in Swedish 7-year-old children. Dev Med Child Neurol 40: 796-804.
- Kaplan BJ, Wilson BN, Dewey D, Crawford SG (1998) DCD may not be a discrete disorder. Hum MovSci 17: 471-490
- Henderson SE, Sugden DA (1992) Movement assessment battery for children. London, UK.The Psychological Corporation.
- Racine MB, Majnemer A, Shevell M, Snider L (2008) Handwriting performance in children with attention deficit hyperactivity disorder (ADHD). J Child Neurol 23: 399-406.
- Raberger T, Wimmer H (2003) On the automaticity/cerebellar deficit hypothesis of dyslexia: balancing and continuous rapid naming in dyslexic and ADHD children. Neuropsychologia 41: 1493-1497.
- Udal A, Malt U, Lovdahl H, Gjaerum B, Pripp A, et al. (2009) Motor function may differentiate attention deficit hyperactivity disorder from early onset bipolar disorder. Behavioral and Brain Functions 5: 47.
- Kroes M, Kessels AG, Kalff AC, Feron FJ, Vissers YL, et al. (2002) Quality of movement as predictor of ADHD: results from a prospective population study in 5- and 6-year-old children. Dev Med Child Neurol 44: 753-760.
- Hashimoto E, Sakaguchi S, Shiga M, Ikeda N, Toki S, et al. (2001) Epidemiological studies of tobacco smoking and dependence in Japan. Alcohol 24: 107-110.
- Knights RM, Hinton GG (1969) The effects of methylphenidate (Ritalin) on the motor skills and behavior of children with learning problems. J NervMent Dis 148: 643-653.
- Miyahara M, Piek J, Barrett N (2006) Accuracy of drawing in a dual-task and resistance-to-distraction study: motor or attention deficit? Hum MovSci 25: 100-109.
- Yan JH, Thomas JR (2002) Arm movement control: differences between children with and without attention deficit hyperactivity disorder. Res Q Exerc Sport 73: 10-18.
- Eliasson AC, Rösblad B, Forssberg H (2004) Disturbances in programming goal-directed arm movements in children with ADHD. Dev Med Child Neurol 46: 19-27.
- Kalff AC, de Sonneville LM, Hurks PP, Hendriksen JG, Kroes M, et al. (2003) Low- and high-level controlled processing in executive motor control tasks in 5-6-year-old children at risk of ADHD. J Child Psychol Psychiatry 44: 1049-1057.
- Reitan RM, Wolfson D (1993) The Halstead-Reitanneuropsychological test battery: theory and clinical interpretation. (2ndedn), Tucson, Ariz, Neuropsychology Press.
- Stray LL (2009) Motor problems in Children with ADHD and clinical effects of Methylphenidate as assessed with the MFNU in Faculty of Arts and Education, Stavanger.
- Stray LL (2001) Motorikk hos barn med ADHD: en retrospektivstudieavmotoriskevansker hos barn med ADHD basert pa modifisertfunksjonsnevrologiskundersøkelse (MFNU). inMedisinskfakultet. Universitetet i Bergen: Bergen.
- Ellertsen B, Stray LL, Johnsen IMB. Adult ADHD in clinical neuropsychology.Examination of adult patients.
- Bjelland T (2001) Some Norwegian children with AD / HD with proven benefit of stimulant medication. Skolepsykologi: 11-21.
- Stray LL, Iversen S, Stray T, Ellertsen B, Ruud A (2006) MFNU - Motor Function Neurological Examination User Manual.
- Stray LL, Stray T, Iversen S, Ruud A, Ellertsen B (2009) Methylphenidate improves motor functions in children diagnosed with Hyperkinetic Disorder. Behavioral and Brain Functions 5: 21
- Stray LL, Stray T, Iversen S, Ruud A, Ellertsen B, et al. (2009) The Motor Function Neurological Assessment (MFNU) as an indicator of motor function problems in boys with ADHD. Behav Brain Funct 5: 22.
- Stray LL, Ellertsen B, Stray T (2010) Motor function and methylphenidate effect in children with attention deficit hyperactivity disorder. ActaPaediatr 99: 1199-1204.
- Stray LL, Kristensen Ø, Lomeland M, Skorstad M, Stray T, et al. (2013) Motor regulation problems and pain in adults diagnosed with ADHD. Behav Brain Funct 9: 18.
- Milich R, Balentine AC, Lynam DR (2001) ADHD combined type and ADHD predominantly inattentive type are distinct and unrelated disorders. ClinPsycholSciPract 8: 463-488.
- Barkley RA (2001) The Inattentive Type of ADHD As a Distinct Disorder: What Remains To Be Done. ClinPsycholSciPract 8: 489-493.
- Johnstone M (1974) The effects of methylphenidate on postoperative pain and vasoconstriction. Br J Anaesth 46: 778-783.
- Moore JL, McAuley JW, Long L, Bornstein R (2002) An Evaluation of the Effects of Methylphenidate on Outcomes in Adult Epilepsy Patients. Epilepsy Behav 3: 92-95.
- Bart O, Podoly T, Bar-Haim Y (2010) A preliminary study on the effect of methylphenidate on motor performance in children with comorbid DCD and ADHD. Res DevDisabil 31: 1443-1447.
- Flapper BC, Houwen S, Schoemaker MM (2006) Fine motor skills and effects of methylphenidate in children with attention-deficit-hyperactivity disorder and developmental coordination disorder. Dev Med Child Neurol 48: 165-169.
- Bart O, Daniel L, Dan O, Bar-Haim Y (2013) Influence of methylphenidate on motor performance and attention in children with developmental coordination disorder and attention deficit hyperactive disorder. Res DevDisabil 34: 1922-1927.
- Fox O, Adi-Japha E, Karni A (2014) The effect of a skipped dose (placebo) of methylphenidate on the learning and retention of a motor skill in adolescents with Attention Deficit Hyperactivity Disorder. Eur Neuropsychopharmacol 24: 391-396.
- Kessler RC, Lane M, Stang PE, Van Brunt DL (2009) The prevalence and workplace costs of adult attention deficit hyperactivity disorder in a large manufacturing firm. Psychol Med 39: 137-147.
- Young JL, Redmond JC (2007) Fibromylagia, chronic fatigue, and adult attention deficit hyperactivity disorder in the adult: a case study. Psychopharmacol Bull 40: 118-126.
- Treister R, Eisenberg E, Demeter N, Pud D (2015) Alterations in pain response are partially reversed by methylphenidate (Ritalin) in adults with attention deficit hyperactivity disorder (ADHD). Pain Pract 15: 4-11.
- Ruud A, Arnesen P, Stray LL, Vildalen S, Vesterhus P (2005) Stimulant medication in 47,XYY syndrome: a report of two cases. Dev Med Child Neurol 47: 559-562.
- Gillberg C (2010) The ESSENCE in child psychiatry: Early Symptomatic Syndromes Eliciting Neurodevelopmental Clinical Examinations. Research in Developmental Disabilities 31: 1543–1551.
- Mueller S, Costa A, Keeser D, Pogarell O, Berman A, et al. (2014) The effects of methylphenidate on whole brain intrinsic functional connectivity. Hum Brain Mapp 35: 5379-5388.
- Villemonteix T, Purper-Ouakil D, Romo L (2014) [Is emotional dysregulation a component of attention-deficit/hyperactivity disorder (ADHD)?] Encephale .
- Stray T (2013) DAT - Kon: a tool for differentiation of behavioral and concentration problems in children.
- Degangi GA, Breinbauer C, Roosevelt JD, Porges S, Greenspan S (2000) Prediction of Childhood Problems at Three Years in Children Experiencing Disorders of Regulation during Infancy. Infant Mental Health Journal 21: 156-175.
- Ghanizadeh A (2009) Can Behavioral Sensory Processing Problems Guide Us to a Better Pharmacological Management of Children with Attention Deficit Hyperactivity Disorder? A Case Report. Psychiatry 12: 40-43.
- Mangeot SD, Miller LJ, McIntosh DN, McGrath-Clarke J, Simon J, et al. (2001) Sensory modulation dysfunction in children with attention-deficit-hyperactivity disorder. Dev Med Child Neurol 43: 399-406.
- Stray LL (2004) Handicap Understanding and inclusion. Spesialpedagogikk: 20-27.
- Bye KC, Kjeldstad AB, Nyborg B (2011) Intensivstabilitetstreningav barn med AD/HD.
- Hugdahl T, Buicioto H, Helgemo H, Hoven G, Jozefiak T, et al. (2004) Quality Assurance Project. Can ADHD diagnosed by local support services? St. Olavs Hospital: Trondheim.
- Skranes JS, Lohaugen GC (2013) Barnelegensoppgaver.Supplerendemedisinskeundersøkelse
- Hokkerup B (2012) Quality of movement and motor problems in patients with ADHD, implications for Therapeutic riding approach. The IOPTP Newsletter: 8-13.
Citation: Stray LL, Stray T, Kristensen O (2015) Neuromuscular Regulation Problems in Attention Deficit Hyperactivity Disorder Assessed by the Motor Function Neurological Assessment. J Nov Physiother 5:255. DOI: 10.4172/2165-7025.1000255
Copyright: © 2015 Stray LL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 24954
- [From(publication date): 4-2015 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 20171
- PDF downloads: 4783