Neonatal Tetanus in Gabon: About 2 Cases
Received: 25-Feb-2018 / Accepted Date: 15-Mar-2018 / Published Date: 26-Mar-2018 DOI: 10.4172/2572-4983.1000151
Abstract
Background: Poor information about neonatal tetanus cases are assembled in Gabon.
Aim: To recall practitioner about the existing danger of neonatal tetanus despite efforts made by immunization in the country and worldwide.
Observations: We write about two observations in two teaching hospitals at the same period. One treated, and the other lethal. We assess their cases with the commonly used scale in Africa: Dakar Classification.
Conclusion: Despite the worldwide actions against neonatal tetanus, cases appear, and we must screen the mothers with exposure factors.
Keywords: Neonatal tetanus; Gabon; Immunization
Introduction
Neonatal tetanus (NT) is a serious, reportable disease that can be prevented by immunization [1]. To prevent maternal and neonatal tetanus (MNT), the vaccine had been introduced in more than 106 countries by the end of 2016. An estimated 84% of newborns were protected through this vaccination. Between 2000 and May 2016, MNT was eliminated in 40 countries, but remains a public health problem in 18 developing countries, mainly in Africa and Asia, where incidence and mortality are high [2-4]. In developed countries, tetanus is rare due to progress in hygiene and immunization. Neonatal and maternal forms of tetanus are the targets of a global elimination policy launched from 2000 to 2005 [3-6]. The main strategy for achieving elimination is to give women at least two doses of Tetanus Vaccine + tetanus toxoid vaccine before or during pregnancy (Table 1).
| Criterias | 0 | 1 |
|---|---|---|
| 1.Incubation | ≥7 days | <7 days |
| 2.Invasion | ≥2 days | <2 days |
| 3.Wound | Other or unknown | Ombilicus, uterus, burn, intramuscular injection. |
| 4.Paroxysm | Missing | Present |
| 5.Rectal temperature | ≤38.4°C | >38.4°C |
| 6.Neonate pulse | ≤150/min | >150/min |
Table 1: Dakar classification.
In Gabon, tetanus immunization is free under the Expanded Program on Immunization (EPI), targeting children from 0 to 11 months of age and women of childbearing age. The diagnosis of neonatal tetanus is clinical [7] and the classification of Dakar (1977) allows a prognostic score on six points (Table 1).
The purpose of this study was to remind the gravity of neonatal tetanus, the primary role of prevention through vaccination and the obligation to identify and report cases, in order to strengthen the implementation of the MNT elimination initiative. We report two cases of neonatal tetanus observed in two Teaching Hospitals which are reference centers in our health system because of the intensive activity, and the aptitude of their staff.
Case Report 1
A woman was hospitalized at Agondje Teaching Hospital at day 12 of life for vomiting and fever. Her mother is 23 years old, single, with a primary school education level, without a job, living in a suburban district, with no particular surgical or medical record. It was her second pregnancy, followed up by a midwife. She had less than four prenatal visits and an incomplete prenatal check-up. During the pregnancy she had one episode of malaria insufficiently treated. The vaccination status was unknown because of the lack of a maternity record. The delivery took place at home practiced by a family member. The section of the cord was made with a razor blade. On examination, we noted a weight of 3400 grams. The rectal temperature was 39°C, the heart rate was normal, the mucous membranes were well stained and the hydration status was good. All the neonate examination was normal. The diagnosis was that of a probable maternal-fetal bacterial infection associated with malaria and treated as such. At day 16, fourth day of hospitalization, the newborn presented irritability followed by general contractures, exacerbated by light and noise, evolving in a feverish context. The diagnosis of neonatal tetanus was made with an estimated Dakar Score of 4.
Case Report 2
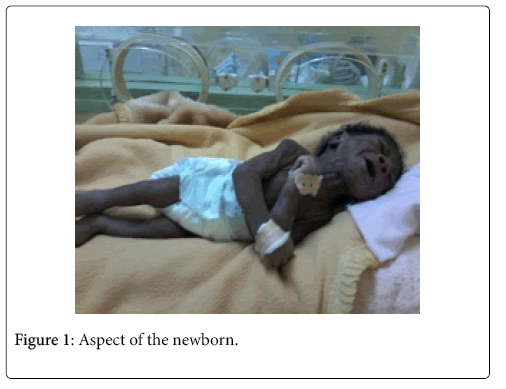
Another woman was hospitalized at the Libreville Teaching Hospital at day 9, her mother was 20 years old, single, with a primary school education level, without a job, living in a suburban district, with no particular surgical or medical record. It was her second pregnancy with only one prenatal consultation, incomplete antenatal checkup and no tetanus vaccination. The progress of the pregnancy was normal. The delivery took place at home, practiced by a traditional birth attendant without aseptic measures. The section of the cord was made with a razor blade. In the history of the disease, the signs appeared suddenly at day 6 of life by an impossibility to feed associated with generalized contracture appearing gradually. We noticed a weight of 2600 grams, rectal temperature was 40°C, heart rate was 195 beats per minute; the general condition was altered with a grey color and a poor state of hydration. The child had contractures with the opisthotonos (Figure 1), emphasized by light and sound.
The per-critical consciousness was normal, there was no cry. There was a respiratory distress with flutter of the nose, an intercostal impression and a polypnea of 76 cycles per minute. The abdomen was distended and the rest of the examination was unremarkable. The diagnosis of neonatal tetanus was made with an estimated Dakar Score of 5.
The management of these two cases consisted in antibiotic therapy with penicillin G, oxygen therapy, serotherapy, subcutaneous tetanus immunotherapy, administration of phenobarbital (Gardenal®) and diazepam (Valium®). The adjuvant measures were the sensory isolation of the patient by protecting from light and noise sources (Figure 2), nursing and nutritional intake by gavages.
The evolution was satisfactory in observation 1, marked from the second day of treatment by the disappearance of contractures, an apyrexia and a Dakar score estimated at 1. The newborn was out of service at D28 of life. In the observation 2, it was marked by the occurrence in J25 of life of a nosocomial infection having led to the death at J33 of life.
Discussion
Neonatal tetanus typically occurs in newborns who suckle and cry during the first few days, then progressively develop a difficulty and then inability to suck because of trismus (contraction of the jaws), general stiffness with spasms or convulsions and opisthotonos (contracted back hyperextension) [8]. In both cases, the clinical diagnosis of NT was made in the presence of febrile behavior and tone disorders, neonates born at home, unvaccinated mothers, absence of asepsis at the time of treatment. Child birth, the method of sectioning the cord and the lack of information about home cord care. The signs were obvious: hypertonic crises with preserved consciousness, evolving against a background of global hypertonia. This was a serious tetanus for the 2 children according to the Dakar international classification, with a mortality risk higher than 80% for an estimated score of 5 and a short incubation period.
NT appeared within 3 to 14 days after birth as classically. Evocative symptoms were refusal to suckle, unexplained crying, fever. The evolutionary stage was that of the trismus invasion phase and the state phase with a generalized permanent contracture associated with acute paroxysmal contracture attacks. A complication appeared to type of nosocomial infection.
The goals of the treatment were to neutralize the non-fixed toxin on the central nervous system, treat the symptoms, avoid super infections, while preserving the vital functions. The treatment was continued for approximately 3 weeks for the survivor. The delay in treatment was delayed and the lethality high.
Tetanus is an infectious disease whose incidence, mortality and lethality closely reflect the level of socioeconomic development, health and immunization coverage of a country's population.
These 2 observations focus on indicators that can guide the risk of NT recrudescence in our environment and on which actions must be carried out at the national level. These are the immunization coverage of women of child bearing age, the proportion of home birth and the reporting of NT cases.
We find the same circumstances of classic events described in the literature in cases of NT, such as the insufficient number of prenatal consultations, the absence of doses of Antietam’s vaccine, home delivery, in areas suburban often poorly sanitized, lack of qualification of the midwife, average age of 9 days, umbilical portal and death rate of 50% [9,10]. This situation can be explained by the limited access to maternal and child health services in relation to the low socioeconomic level of parturient.
Tetanus cannot be eradicated due to the persistence of the causative agent in the environment. The prevention of NT is based on the vaccination of all women aged from 15 and 49, pregnant or not, with an improvement of hygiene measures of deliveries. The elimination of MNT is defined as the reduction of incidence to less than one case of neonatal tetanus per 1,000 live births in all districts of all countries [11]. These cases of NT constitute a failure of the health system. Gabon analysis of the VAT2 + coverage of pregnant women show just under half of women who received at least two doses during their last pregnancy and that efforts should be made. Other countries have made progress, such as Burkina Faso and Cameroon, where national immunization coverage has increased from 57% to 80% and from 54% to 81% respectively [12]. These results are a consequence of the intensification of routine immunization associated with additional vaccination campaigns carried out in the high-risk districts of NT. These campaigns have provided global protection against maternal tetanus [13]. Childbirth assisted by qualified health personnel ensures compliance with hygiene rules and postnatal care adapted for the mother-child relationship in order to reduce infant and maternal mortality [14]. The proportion of assisted deliveries remains low in Africa and varies by country; it is greater than 70% in Gabon [12]. The persistence of home deliveries may be related to the low educational attainment of this population of women and the lack of regular awareness of the benefits of childbirth in a health facility.
Conclusion
NT remains a severe pathology easy to diagnose, for which prevention through vaccination remains the best mean of control. Early management in a referral health facility reduces sequelae and determines prognosis. Progress is still to be made in eliminating MNT by strengthening a national policy of several indicators, such as: the implementation of vaccination campaigns for women of reproductive age and the improvement of childbirth conditions. In addition, the establishment of epidemiological surveillance will make it possible to evaluate the effectiveness of the MNT elimination strategy and to identify the high-risk districts of NT in order to optimize the response.
References
- Kra O, Aoussi E, Aba YT (2014) Current aspects of tetanus in the service of Infectious and Tropical Diseases, Treichville Teaching Hospital (Abidjan). Rev Tunisied’Infectiol 4: 173-177.
- WHO (2011) The coverage of routine immunization worldwide 2010, progress towards polio eradication: Afghanistan and Pakistan, 2010-2011.Wkly Epidemiol Rec. 86: 509-512.
- UNICEF (2015) Unissons-nous pour les enfants. Santé. Elimination du tétanosmaternel et néonatal.
- UNICEF, UNFPA,WHO (2015) Eliminerdurablement le tétanosmaternel et néonatal. Plan stratégique 2012-2015. p: 28.
- UNICEF, OMS, FNUAP (2010) Elimination du tétanosmaternel et néonatald’ici à 2005. Stratégiespermettantd’éliminer le tétanos et d’évitersaréapparition, p: 36.
- Vandelaer J, Birmingham M, Gasse F, Kurian M, Shaw C, et al. (2003) Tetanus in developing countries: an update on the maternal and neonatal tetanus elimination initiative. Vaccine 21: 3442-3445.
- Guignard J, Cloup M (1981) Tétanosnéo-natal-Encycl. Méd. Chir. Pédiatrie. Paris.
- Joyce MP, Vandelaer J (2010) Tétanosmaternel et neonatal-TMN. Manuel - Contrôle des Maladies Transmissibles. GLOBE.
- Sow PS, Seydi M, Diop BM, Dia NM, Manga NM, et al. (2003) Facteurspronostiques du tétanos neonatal à Dakar. Med Mal Inf 33: 150-154.
- Sow PS, Diop A, Diop BM, FayeMA, Ki-ZerboG, et al. (1995) Les aspects épidémiologiques du tétanosnéonatal à Dakar. Med Mal Inf 25: 1178-1182.
- OMS (1994) Notes et activités: l’éliminationmondiale du tétanosnéonatal; progrèsréalisés. Bulletin de l’OrganisationMondiale de la santé. 72: 165-175.
- WHO (2006) Tetanus Vaccine: WHO position paper. WklyEpidemiol Rec 81: 198-208.
- Ministère de la Santé et de la Prévention (2009) Plan national de development sanitaire, PNDS 2009-2018,pp: 1-86.
Citation: Minko JI, Kamgaing EK, Steeve MR, Koko J, Ategbo SJ (2018) Neonatal Tetanus in Gabon: About 2 Cases. Neonat Pediatr Med 4: 151. DOI: 10.4172/2572-4983.1000151
Copyright: © 2018 Minko JI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5658
- [From(publication date): 0-2018 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 4793
- PDF downloads: 865