Research Article Open Access
Neonatal Obstetric Trauma in a Hospital in the Suburbs of Dakar, Senegal
Jean Baptiste Diouf1*, Ndèye Marème Sougou2, Amadou Lamine Fall3, Mariama Kane1 and Ousmane Ndiaye3
1Department of Pediatric, Centre Hospitalier Roi Baudouin Guédiawaye, Dakar, Senagal
2Department of Preventive Medicine and Public Health, Medicine Cheikh Anta Diop University, Dakar, Senagal
3Department of Pediatrics, Medicine Cheikh Anta Diop University, Dakar, Senagal
- *Corresponding Author:
- Diouf JB
Department of Pediatric
Centre Hospitalier Roi Baudouin Guédiawaye
Dakar, Senegal
Tel: 00221338374647
Fax: 00221338770261
E-mail: jeanniokhor@yahoo.fr
Received Date: March 02, 2017; Accepted Date: March 07, 2017; Published Date: March 17, 2017
Citation: Diouf JB, Sougou NM, Amadou Lamine Fall, Kane M, Ndiaye O (2017) Neonatal Obstetric Trauma in a Hospital in the Suburbs of Dakar, Senegal. Neonat Pediatr Med 3: 122. doi: 10.4172/2572-4983.1000122
Copyright: © 2017 Diouf JB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Introduction: Neonatal obstetric traumas remain an important cause of morbidity-mortality. The objective of this study was to study obstetric traumatic lesions of the new-born in the paediatric department of the Centre hospitalier Roi Baudouin. Patients and method: This was a descriptive retrospective study of new-borns with obstetric trauma received at the Centre hospitalier Roi Baudouin’s paediatric ward over a 12-month period. The variables studied were maternal (age, parity, presentation, mode of delivery and place of delivery,) and neonatal (birth weight, type of lesion and diagnosis time). Results: Out of the 1426 new-borns received during the study period, 60 had trauma, a hospital frequency of 4.2%. The average age of new-borns for consultation was 8.85 days. The known and found contributory factors were: birth weight greater than 3500 g and the absence of cry at birth. Births were delivered by midwives (80%), the hospital was the main place of birth (61.7%). The main clinical presentations were: neonatal brachial plexus palsy (38.3%), fracture of the clavicle (33.3%) and caput succedaneum (13.3%). Conclusion: New-born obstetric trauma are relatively frequent at the Centre hospitalier Roi Baudouin The diagnosis is delayed due to a lack of proper examination of the new-born in the delivery room. Systematic examination of new-born at birth would be a reliable means for the detection and early management of this condition.
Keywords
Trauma obstetrical; New-born; Senegal
Introduction
Traumatic lesions are one of the major causes of neonatal morbidity in developing countries. They are often attributable to physical assault during labor. The causal or contributory role of adverse obstetric factors and role and competencies of health workers is clearly evident. Diagnosis involves careful examination of the new-born in the delivery room and the prognosis depends on the precocity of the treatment and the severity of the lesions. Their prevalence is variously appreciated and varies according to the studies. In fact, little work has been done on neonatal obstetric trauma, particularly in Africa. Keita in Guinea Conakry, found in 2002 a frequency of 21.18% and 5.50% compared to hospitalizations and consultations of children with obstetric trauma [1]. Similarly Hermann in Cameroon found in 2014 a hospital frequency of 1.84% of obstetric trauma [2]. In Senegal, a study carried out at the Centre hospitalier Abass Ndao in 2001 on traumatic lesions of the new-born after forceps delivery reported a mortality rate of 10.44% [3]. Guèye, in a study carried out at the Hospital principal in Dakar in 2004, found a prevalence of traumatic lesions of 3 per 1000 in the new-born [4].
This study was conducted to determine the epidemiological characteristics of new-borns with obstetric traumatic lesions and to identify risk factors which was associated to these lesions
Patients and Methods
We conducted a descriptive retrospective study during 12-month from 1 July 2014 to 30 June 2015 at the Centre hospitalier Roi Baudouin. This health facility is located in Guédiawaye, which is one of the four departments in the Dakar region.
The study population consisted of children with any type of obstetric trauma.
The following variables were studied:
Maternal
• Age divided into 5 categories: (18 years-22 years), (23 years-27 years), (28 years-32 years), (33 years-37 s) and >37 years old.
• Gestity: the number of pregnancies.
• Parity divided into primiparous women (1 child birth) pauciparous women (2 to 3 deliveries) and multiparous women (>3 deliveries).
Pregnancy Follow-up of
• The number of prenatal consultations.
• The number of tetanus toxoid vaccine doses received.
• The biological assessment.
• Obstetric ultrasound.
Per-natal data
• Place of delivery.
• The qualification of the birth attendant.
• The term of pregnancy established from the date of the last menstruation or from the early ultrasound.
• The mode of presentation: cephalic, breech.
• Mode of delivery: vaginal, instrumental extraction, caesarean section.
• The Apgar score in the 5th minute divided into 3 groups: Apgar lower than 4, between 4 and 7 and higher than 7.
• The cry of the new born at birth.
• Birth weight assessed within one hour of birth using a scale of 10 gram precision.
Post-natal data
• The age of the child at the time of diagnosis.
• Neonatal obstetric trauma observed.
The data were entered in the Microsoft Office Excel software and analysed by the SPSS.20.0 software. In the analysis a descriptive and analytical study was made. The threshold of significance of the tests was set at 5%.
Results
Characteristics of mothers
The average age was 27 years with extremes ranging from 18 to 40 years. The age group of (23-27) is more representative with 30%. Most women (31.7%) were primigravida while pauciparous women accounted for 51.7% and primiparous women 30%. Regarding the follow-up of pregnancy, (Table 1) the majority of women (76.7%) received proper follow-up with a number of prenatal consultations higher than 3; Seventy percent (70%) received at least 2 doses of tetanus toxoid vaccine and 91.7% had a biological and ultrasound assessment.
| Variables | No. of persons | Percentage (%) | |
|---|---|---|---|
| (18 yrs-22 yrs) | 15 | 25 | |
| (23 yrs -27 yrs) | 18 | 30 | |
| Maternal | (28 yrs -32 yrs) | 14 | 23,3 |
| age | (33 yrs -37 yrs) | 10 | 16,7 |
| >37 yrs | 3 | 5 | |
| 1 | 19 | 31,7 | |
| 2 | 15 | 25 | |
| 3 | 14 | 23,3 | |
| Gestity | 4 | 8 | 13,3 |
| 5 | 1 | 1,7 | |
| >5 | 3 | 5 | |
| Primiparous | 18 | 30 | |
| Parity | Pauciparous | 31 | 51,7 |
| Multiparous | 11 | 18,3 | |
| Number of CPNs | <4 | 14 | 23,3 |
| ≥4 | 46 | 76,7 | |
| 0 | 3 | 5 | |
| Dose of TTV received | 1 | 8 | 13.3 |
| 2 | 42 | 70 | |
| 3 | 7 | 11.7 | |
| Biological assessment | Yes | 55 | 91,7 |
| No | 5 | 8.3 | |
| Obstetrical ultrasound | Yes | 55 | 91.7 |
| No | 5 | 8,3 |
PNC: Prenatal consultation
TTV: Tetanus toxoid vaccine
Table 1: Characteristics of mothers.
Pernatal and neonatal data
Childbirths occurred in born in 61.7% of cases. 80% were performed by midwives, 16.6% by medical officers and 1.7% by nurses or matrons. There was no statistically significant relationship between the occurrence of lesions and the qualification of the birth attendant (p=0.962). The majority (95%) of women had given birth at term and cephalic presentation was predominant (96.7%). Vaginal deliveries accounted for 90%, instrumental extraction 6.7%, and caesarean section 3.3%.
The woman’s perineum was intact in 53.4% of cases while in 23.3% there was a perineal laceration or galling. Similarly, an episiotomy was performed in 23.3% of cases. The majority of children (43.3%) had an Apgar score between 4 and 7 at the 5th minute of life. Birth cry were present in 80% of cases, and there was a statistically significant relationship between the absence of cry at birth and the occurrence of neonatal obstetric trauma (p=0.019). With regard to the new-born, 60% of the children had a birth weight higher than 3500 grams and there was a statistically significant relationship between a birth weight greater than 3500 grams and the occurrence of a neonatal obstetric trauma (p=0.011). The average age of newborns at the time of diagnosis was 8.85 days with extremes ranging from 1 to 41 days.
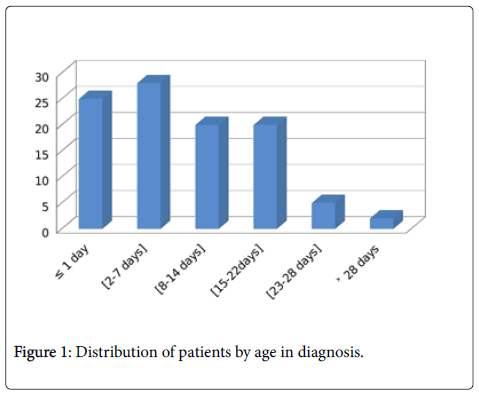
Only 25% of children were diagnosed within 24 hours of birth. The majority of children (28%) were diagnosed between 2 and 7 days and 2% of children beyond 28 days.
Traumatic lesions
The most significant trauma in neonates was the neonatal brachial plexus palsy (38.3%), clavicle fracture (33.3%), and caput succedaneum (13.3%). Femoral fracture, sternocleidomastoid haematoma and facial paralysis were less frequent and each represented 1.7% (Table 2).
| Variables | No. of persons | Percentage (%) | |
|---|---|---|---|
| Delivery place | In born | 37 | 61.7 |
| Out born | 23 | 38,3 | |
| Qualification of birth attendant | Midwife | 48 | 80 |
| Medical officer | 10 | 16.6 | |
| Nurse | 1 | 1.7 | |
| Matrone | 1 | 1.7 | |
| Pregnancy term | At term | 57 | 95 |
| Not at term | 3 | 5 | |
| Presentation | Céphalic | 58 | 96.7 |
| Breech | 2 | 3.3 | |
| Delivery mode | Vaginal | 54 | 90 |
| Vaginal assisted by instrument | 4 | 6.7 | |
| Caesarean | 2 | 3.3 | |
| Perineal lesions | Tearing | 14 | 23.3 |
| Episiotomy | 14 | 23.3 | |
| Intact perineum | 32 | 53.4 | |
| Apgar at birth | < 4 | 4 | 6.7 |
| (4-7) | 30 | 50 | |
| >7 | 26 | 43.3 | |
| Scream at birth | Yes | 48 | 80 |
| No | 12 | 20 | |
| Birth weight | ≤3500 grams | 24 | 40 |
| >3500 grams | 36 | 60 |
Table 2: Pernatal and neonatal data.
Discussion
Our aim was to study the epidemiological characteristics of newborns with obstetric traumatic lesions and those of their mothers in order to identify the risk factors and associated factors with these lesions (Table 3). Thus, it was noted a hospital frequency of 4.2% for traumatic obstetric lesions. It is higher than the literature found in lot of african hospital [2,4]. On the other hand, it is lower than that found in Guinea which was 21.18% and 5.50% compared to hospitalizations and consultations of children with obstetric trauma [1]. This high frequency observed in our study and that of Guinea can be explained by the fact that these series deal with trauma in relation to all newborns received in consultation and / or hospitalization and not in relation to all live births during the study period (Figure 1).
| Diagnosis | No. of pers. | Percentage (%) |
|---|---|---|
| Neonatal brachial plexus palsy | 23 | 38.3 |
| Clavicle fracture | 20 | 33.3 |
| Caput succedaneum | 8 | 13.3 |
| Cephalohaematoma | 4 | 6.7 |
| Femur fracture | 1 | 1.7 |
| sternocleidomastoid haematoma | 1 | 1.7 |
| Humerus fracture | 2 | 3.3 |
| Facial paralysie | 1 | 1.7 |
Table 3: Diagnosis of traumatic lesions.
The average age of mothers was 27 years with extremes varying between 18 and 40 years. The age group of (23-27) is more representative with 30%. These results are similar to those found in other series [4-6]. These similar averages correspond to the period of genital activity and do not constitute a factor favouring obstetric trauma. No link was found between the occurrence of a lesion and an age group in our series.
In our study, the mean parity was 2.4. Pauciparous women accounted for 51.7% while primiparous women 30%. Primiparity is considered to be a factor that contributes to obstetric trauma especially if it is associated with other factors such as macrosomia and shoulder dystocia [7-9]. Despite the high number of primiparas and pauciparas in our study, we did not find any link with the occurrence of neonatal obstetric trauma.
The majority of mothers (76.7%) received proper follow-up with more than 3 PNCs, seventy percent (70%) of women had received at least 2 doses of TTV and 91.7% had undergone a biological assessment and an obstetric ultrasound. These results indicate that most mothers had a relatively correct follow-up of their pregnancy in our conditions.
A proper follow-up of pregnancy with early detection of fetal-pelvic disproportions can help prevent the occurrence of obstetric trauma.
In our study, the majority of women (61.7%) had given birth in hospitals. The delivery was performed by a midwife in 80% of cases and a medical officer in 16.6%. In one study in Cameroon, deliveries were performed at 44.3% by nurses and the health centre was the main place of delivery (42.8%) [2]. For Keita in Guinea, the delivery was performed in 59% by midwives and 38.8% by obstetricians [1].
We identified a birth weight greater than 3500 grams as a factor associated with the occurrence of obstetric trauma (p=0.011). In Senegal, Guèye M. in 2003 found a percentage of 2.98% in macrosomia and 8.95% in hypotrophy [4]. Ndiaye et al. had found a prevalence of 2.7% for the low weight new-born and 10.8% for macrosomia [3]. Obstetric trauma is favoured by macrosomia, macrocrania and fetalpelvic disproportion [10].
In our study, 20% of new-borns had not screamed at birth. The absence of cry at birth was identified as a factor associated with the occurrence of neonatal obstetric trauma (p=0.019). Similarly, 43% of the new-borns had an Apgar score between 4 and 7 at the 5th minute of life and in 5% of the new-borns; this score was less than 4. For Guèye, more than half of new-borns (75%) had fetal distress [4].
Holden et al. [10], in a 6-month study in England, found 43% of fetal distress in new-borns with trauma. Obstetric trauma is often associated with perinatal asphyxia [11].
In our study, 58 new-borns were born vaginally and 2 by caesarean section. Of the neonates born vaginally, 4 were extracted through vacuum. Similarly, 53.4% of women had delivered with an intact perineum.
In the study conducted at the Hôpital principal in Dakar, 7.46% of neonates were extracted through caesarean section, the rest vaginally of which 67.16% through forceps [4]. Hameed, in 2010 found in Baghdad that 70% of newborns were born vaginally against 30% through caesarean section [12].
The average age of newborns at the time of diagnosis was 8.85 days with extremes ranging from 1 to 41 days. In a study in Cameroon, the average age of newborns was 12.49 ± 9.39 days [2].
The diagnosis of obstetric trauma should be performed in the delivery room and systematic examination of the newborn at birth would be a reliable means for the detection and early management of this pathology (Table 4).
| Authors | Types of lesions | Percentage |
|---|---|---|
| Guèye [4] | Neonatal brachial plexus palsy | 11.94% |
| Senegal | Clavicle fracture | 7.46% |
| Caput succedaneous | 28.36% | |
| Hermann [2] | Neonatal brachial plexus palsy | 70.6% |
| Cameroon | Clavicle fracture | 22.5% |
| Caput succedaneous | - | |
| Borna [14] | Neonatal brachial plexus palsy | 8.78% |
| Iran | Clavicle fracture | 37.83% |
| Caput succedaneous | - | |
| Our study | Neonatal brachial plexus palsy | 38.3% |
| Clavicle fracture | 33.3% | |
| Caput succedaneous | 13.3% |
Table 4: Distribution of the different obstetric lesions based on authors.
The most significant trauma in our series were neonatal brachial plexus palsy (38.3%), clavicle fracture (33.3%) and caput succedaneous (13.3%). Our results do not differ from those found in the literature in which the most frequent obstetric trauma are neonatal brachial palsy, cephalohaematoma, caput succedaneous and clavicle fracture [13,14].
Conclusion
This study shows that the prevalence of obstetric traumatic lesions remains high in neonates in the Dakar suburbs. A birth weight greater than 3500 grams and an absence cry at birth are the factors associated with the occurrence of these lesions. The diagnosis is delayed due to a lack of proper examination of the new-born in the delivery room. Systematic examination of the new-born at birth would be a reliable means for the detection and early management of this pathology.
References
- Keita M, Radji M, Doumbouya N (2001)Traumatismes d’origine obstétricale : fréquence et stratégies de prise en charge dans le service de chirurgie (Guinée Conakry). Med Afr Noire 40: 430-433.
- Hermann ND (2014) Aspects épidémiologiques, cliniques et thérapeutiques des traumatismes obstétricaux du nouveau-né reçus à l'hopital gynéco obstétrique et pédiatrique de Yaoundé. Health Sci Dis 15
- Ndiaye O, Diouf L, Sylla A, Ba M, Diallo R, et al. (2001) Lésions traumatiques du nouveau-né après accouchement par forceps à la maternité de l'Hôpital Abass Ndao. Dakar Med 46: 36-38.
- Guèye M, Assane Sylla, Faye PM (2012) Newborns obstetrical injuries in principal hospital center of Dakar. Dakar Med 57: 203-212.
- Ozdener T, Engin-Ustun Y, Aktulay A, Turkcapar F, Oguz S, et al. (2013) Clavicular fracture: Its incidence and predisposing factors in term uncomplicated pregnancy. Eur Rev Med Pharmacol Sci.17: 1269-1272.
- Murguía-González A, Hernández-Herrera RJ, Nava-Bermea M (2013) Risk factors of birth obstetric trauma. Ginecol Obstet Mex. 81: 297-303.
- Demissie K, Rhoads GG, Smulian JC ( 2004) Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. Br Med J 329: 24-29.
- Ju HCY, Donovan T (2009) Fetal macrosomia and pregnancy outcomes. Aust N Z J Obstet Gynaecol 49: 504-509.
- Tandon S, Tandon V (2005) Primiparity : A risk factor for brachial plexus injury in the presence of shoulder dystocia. Journal of Obstetrics and Gynaecology 25: 465-468.
- Holden R., Morsman DG., Davidck GM, O'Connor GM, Coles EC, et al. (1992) Extemal ocular trauma in instrumental and normal deliveries. Br J Obstet Gynecol 2: 132-134.
- Henri BJ (1990) Obstétrique Pratique a Maloine 2ème édition. 52: 413-416.
- Hameed NN (2010) Neonatal Birth Traumas: Risk factors and types. J Fac Med Baghdad 3: 241-245.
- Broux C, Andrini P, Douchin S (2010) Extensive hematoma of the scalp. Renoble Presse Med. 16: 1451-1454.
- Borna H, Rad SM, Borna S (2010) Incidence of and risk factors for birth Trauma in Iran. Taiwan J obst et Gynecol 2: 170-173.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 3725
- [From(publication date):
June-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 2864
- PDF downloads : 861