Navigating the Intersection of HIV and Pregnancy: Ensuring Health and Well-Being for Mother and Child
Received: 03-Jun-2023 / Manuscript No. JCPHN-23-102316 / Editor assigned: 05-Jun-2023 / PreQC No. JCPHN-23-102316 (PQ) / Reviewed: 19-Jun-2023 / QC No. JCPHN-23-102316 / Revised: 22-Jun-2023 / Manuscript No. JCPHN-23-102316 (R) / Published Date: 29-Jun-2023 DOI: 10.4172/2471-9846.1000425
Abstract
The prospect of pregnancy is an exhilarating journey filled with hopes and dreams. For women living with HIV, however, the journey becomes more complex as they must navigate the intersection of HIV and pregnancy. With advancements in medical care and a comprehensive approach to prenatal care, women with HIV can now experience healthy pregnancies and reduce the risk of transmitting the virus to their babies. In this article, we explore the challenges, considerations, and strategies for ensuring the health and well-being of both mother and child in the context of HIV and pregnancy
Keywords
HIV; Pregnancy; Childcare; PMTCT; Caesarean delivery
Introduction
HIV, or Human Immunodeficiency Virus, is a chronic viral infection that attacks the immune system, making individuals more susceptible to infections and illnesses. When a woman with HIV becomes pregnant, there are important factors to consider ensuring the best possible outcomes for both her and her child [1].
Methodology
Preventing mother-to-child transmission (PMTCT)
The prevention of mother-to-child transmission (PMTCT) is a crucial aspect of managing HIV and pregnancy. With proper medical interventions and adherence to treatment, the risk of transmitting HIV to the baby can be significantly reduced. Key strategies for PMTCT include:
Antiretroviral therapy (ART): Pregnant women with HIV are often prescribed antiretroviral medications to control the virus and reduce the risk of transmission. ART is safe and highly effective in suppressing the viral load, allowing women to have healthy pregnancies with minimal transmission risk [2, 3].
Prenatal care: Regular prenatal visits are essential for monitoring the mother's health and the development of the baby. These visits provide an opportunity to assess viral load, adjust medication if necessary, and address any concerns or complications that may arise during pregnancy.
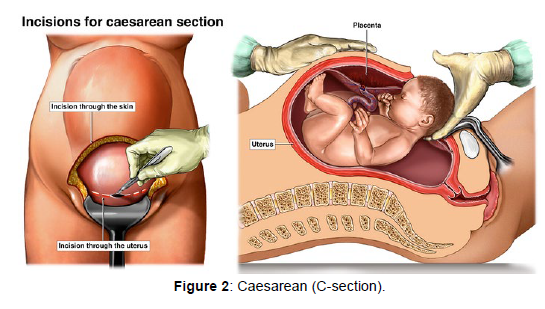
Caesarean delivery: In certain situations, a scheduled caesarean delivery may be recommended to further reduce the risk of transmission. This decision is usually made based on the mother's viral load, overall health, and other factors.
Infant prophylaxis: After birth, new-borns may receive antiretroviral medication for a specific duration to further minimize the risk of acquiring HIV.
Psychological and emotional support
Living with HIV can bring about unique emotional and psychological challenges for expectant mothers. Pregnancy can trigger anxiety, fear of transmitting the virus, and concerns about the baby's health. It is crucial to provide comprehensive support, including counselling and mental health services, to address these concerns and promote emotional well-being [4, 5].
Education and awareness
Education plays a vital role in empowering women with HIV to make informed decisions regarding pregnancy and PMTCT. Access to accurate and up-to-date information about HIV transmission, treatment options, and available support services allows women to take an active role in their healthcare and make decisions aligned with their preferences and circumstances.
Community support and advocacy
Creating a supportive and stigma-free environment is essential for women living with HIV during pregnancy. Community support groups, advocacy organizations, and peer networks can provide a safe space for sharing experiences, gaining knowledge, and receiving encouragement. Promoting awareness and understanding in society at large helps combat discrimination and ensure that pregnant women with HIV receive the care and support they deserve.
Pregnancy is a joyous and transformative experience, regardless of one's HIV status. With proper medical care, adherence to treatment, and a supportive environment, women living with HIV can have healthy pregnancies and greatly reduce the risk of transmitting the virus to their babies. By embracing a comprehensive approach that includes medical interventions, psychological support, education, and community advocacy, we can ensure that every woman has the opportunity to embrace motherhood with confidence, compassion, and optimal health outcomes for both herself and her child [6, 7].
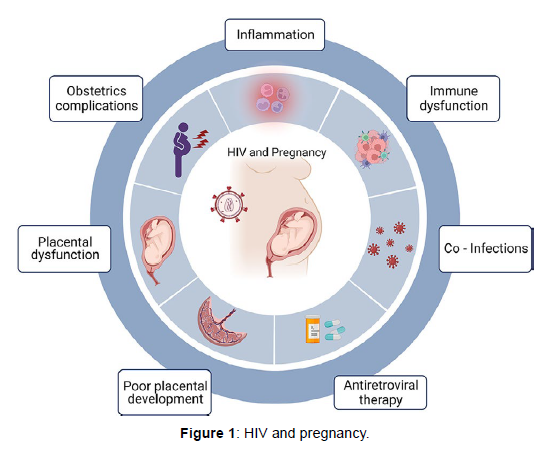
The intersection of HIV and pregnancy presents unique challenges and concerns for both expectant mothers and their unborn children. HIV, or Human Immunodeficiency Virus, is a global health issue that affects millions of individuals worldwide. However, with proper medical care, support, and access to antiretroviral therapy (ART), it is possible for women living with HIV to have safe and healthy pregnancies, reducing the risk of mother-to-child transmission and ensuring a brighter future for both mother and child (Figure 1).
HIV is a virus that attacks the immune system, making individuals more susceptible to infections and diseases. When a woman becomes pregnant while living with HIV, additional considerations come into play, as the virus can be transmitted to the baby during pregnancy, childbirth, or breastfeeding. However, with appropriate interventions, the risk of mother-to-child transmission can be significantly reduced, allowing for a higher likelihood of a healthy pregnancy and birth.
Preventing mother-to-child transmission of HIV is a primary goal in managing HIV and pregnancy. Here are key strategies employed to minimize the risk:It is essential for women to receive regular HIV testing before and during pregnancy. If HIV is diagnosed, immediate access to antiretroviral therapy (ART) is crucial. ART not only improves the health of the mother but also significantly reduces the chances of transmitting the virus to the baby [8-10].
Viral load suppression: Through consistent adherence to ART, women can achieve viral load suppression, reducing the amount of HIV in their blood to undetectable levels. This greatly minimizes the risk of transmission to the baby (Figure 2).
Planned caesarean delivery: In cases where the viral load is detectable near the time of delivery or the woman's health condition requires it, a planned caesarean delivery may be recommended. This helps reduce the exposure of the baby to HIV during childbirth.
Preventing transmission during breastfeeding: In resourcerich settings, where safe alternatives are available, it is generally recommended that women living with HIV avoid breastfeeding. However, in resource-limited settings where the risk of other infant illnesses is high, exclusive breastfeeding coupled with ART can be a viable option.
Alongside medical interventions, expectant mothers living with HIV require comprehensive support and care:
Prenatal Care: Regular prenatal check-ups are essential to monitor the health of the mother and the developing baby. These visits include HIV-specific care, such as viral load monitoring and adjustments to ART, if necessary.
Emotional support: The emotional well-being of pregnant women with HIV is crucial. Support groups, counseling services, and connections with others who have experienced similar journeys can provide much-needed emotional support, reducing stress and anxiety [11].
Education and empowerment: Equipping women with knowledge about HIV, treatment options, and the importance of adherence to medication empowers them to make informed decisions about their health and the well-being of their baby.HIV and pregnancy present complex challenges, but with proper medical care, support, and access to antiretroviral therapy, women living with HIV can navigate pregnancy and childbirth with reduced risks of mother-to-child transmission. Early detection, adherence to treatment, and consistent prenatal care are vital components of ensuring healthy outcomes for both mother and child. By promoting awareness, advocating for accessible healthcare, and providing comprehensive support services, we can work together to create a world where HIV-positive women can embrace the joy of motherhood while safeguarding the future health of their children.
The journey to motherhood is filled with joy, hope, and anticipation. However, when a woman living with HIV becomes pregnant, it introduces additional considerations and challenges. HIV, or Human Immunodeficiency Virus, is a viral infection that weakens the immune system, but with the right knowledge, medical care, and support, women living with HIV can have healthy pregnancies and give birth to HIV-negative babies. This article explores the intersection of HIV and pregnancy, emphasizing the importance of comprehensive care and highlighting the progress made in preventing mother-to-child transmission [12, 13].
HIV is primarily transmitted through unprotected sexual intercourse, sharing needles, or from an HIV-positive mother to her child during pregnancy, childbirth, or breastfeeding. When a woman becomes pregnant, it is crucial for her to receive appropriate medical care, including HIV testing, counseling, and access to antiretroviral therapy (ART). By managing HIV effectively during pregnancy, the risk of transmitting the virus to the baby can be significantly reduced.
Over the years, significant advancements have been made in preventing mother-to-child transmission of HIV. The cornerstone of PMTCT is the administration of antiretroviral drugs to both the mother and the new-born. When taken as prescribed, these medications can suppress the viral load, reducing the risk of transmission to less than 1%. Additionally, avoiding breastfeeding when alternatives are available further minimizes the risk.
Comprehensive prenatal care is essential for women living with HIV. It involves regular medical check-ups, laboratory tests, and monitoring of the mother's health and the baby's development. The healthcare team, including obstetricians, HIV specialists, and counsellors, work collaboratively to ensure the mother's health, manage HIV, and provide necessary support throughout the pregnancy (Table 1).
| HIV and Pregnancy Statistics | Numbers/Percentages |
|---|---|
| Number of women living with HIV globally | 38 million |
| Prevalence of HIV among pregnant women worldwide | 1.5 million (estimated) |
| Percentage of pregnant women with HIV receiving antiretroviral therapy (ART) | 76% |
| Risk of mother-to-child transmission of HIV without intervention | 15-45% |
| Risk of mother-to-child transmission of HIV with appropriate interventions | Less than 1% |
| Number of new pediatric HIV infections annually | 1,60,000 |
| Number of children infected with HIV through mother-to-child transmission annually | 85,000 |
| Percentage of pregnant women living with HIV receiving prenatal care | 80% |
| Percentage of HIV-positive pregnant women aware of their HIV status | 90% |
| Percentage of pregnant women receiving HIV testing and counseling | 95% |
| Percentage of HIV-positive pregnant women receiving antiretroviral therapy (ART) for prevention of mother-to-child transmission | 94% |
| Percentage of pregnant women living with HIV opting for formula feeding instead of breastfeeding | Varies based on cultural and socioeconomic factors |
Table 1: Key statistics and information related to HIV and pregnancy.
Promoting maternal health and well-being
Managing HIV during pregnancy not only focuses on preventing transmission but also emphasizes the overall health and well-being of the mother. This includes addressing other medical conditions, providing appropriate nutrition, managing mental health, and offering support to cope with the emotional aspects of living with HIV. By supporting the mother's overall well-being, the pregnancy experience can be enhanced, contributing to positive outcomes for both the mother and the child.Education and support play vital roles in empowering women living with HIV during pregnancy. Access to accurate information about HIV, treatment options, potential risks, and available resources enables informed decision-making. Support groups and counseling provide a safe space for women to share experiences, seek guidance, and build a network of individuals who understand their unique challenges [14, 15].
Conclusion
HIV and pregnancy present a complex intersection that requires specialized care and support. With advancements in medical treatment,comprehensive prenatal care, and PMTCT strategies, the risk of mother-to-child transmission of HIV can be significantly reduced. It is essential to provide women living with HIV the necessary resources, information, and support to ensure a healthy pregnancy and birth of an HIV-negative baby. By addressing the specific needs and challenges at this intersection, we can empower women to navigate this journey with confidence and give their children the best possible start in life.
References
- Jurate V, Mika S, Petri L (2002) Electrokinetic soil remediation--critical overview. Sci Total Environ 289: 97-121.
- Zhiping S, Hui Z, Yunhong Z (2010) Polyimides: Promising energy-storage materials. Angew Chem Int Ed 49: 8444 - 8448.
- Cavallaro G, Lazzara G, Milioto S (2010) Dispersions of Nanoclays of Different Shapes into Aqueous and Solid Biopolymeric Matrices. Extended Physicochemical Study. J Surf Colloids 27: 1158-1167.
- Lee J, Cameron I, Hassall M (2019) Improving process safety: what roles for digitalization and industry 4.0? Process Saf Environ Prot 132: 325 - 339.
- Baraud F, Tellier S, Astruc M (1997) Ion velocity in soil solution during electrokinetic remediation. J. Hazard Mater 56: 315-332.
- Hong Ji, Weiqiu Huang, Zhixiang Xing, Jiaqi Zuo, Zhuang Wang, et al. (2019) Experimental study on removing heavy metals from the municipal solid waste incineration fly ash with the modified electrokinetic remediation device. Sci Rep 9: 8271.
- Le Borgne S, Paniagua D, Vazquez-Duhalt R (2008) Biodegradation of organic pollutants by halophilic Bacteria and Archaea. J Mol Microbiol Biotechnol 15: 74-92.
- Agamuthu P, Abioye OP, Aziz AA (2010) Phytoremediation of soil contaminated with used lubricating oil using Jatropha curcas. J Hazard Mater 179: 891-894.
- Bergerson JA, Keith D (2010) The truth about dirty oil: is CCS the answer? Environ Sci Technol 44: 6010 -6015.
- Carlson HK, Stoeva MK, Justice NB, Sczesnak A, Mullan MR, et al. (2015) Monofluorophosphate is a selective inhibitor of respiratory sulfate‐reducing microorganisms. Environ Sci Technol 49: 3727-3736.
- Biró B, Köves-Péchy K, Vörös I, Takács T, Eggenberger P, et al. (2000) Interrelations between Azospirillum and Rhizobium nitrogen-fixers and arbuscular mycorrhizal fungi in the rhizosphere of alfalfa in sterile, AMF-free or normal soil conditions. Appl Soil Ecol 15:159-168.
- Chaney R, Angle JS, Mcintosh M, Reeves R, Li YM, et al. (2005) Using hyperaccumulator plants to phytoextract soil Ni and Cd. J Biosci 60: 190-198.
- Faridul A, Tae YK, Song YK, Sadia SA, Prabhat P, et al.(2015)Effect of molybdenum on nodulation, plant yield and nitrogen uptake in hairy vetch. Soil Sci Plant Nutr 61: 664-675.
- Begum N, Qin C, Ahanger MA, Raza S, Khan MI, et al. (2019) Role of Arbuscular Mycorrhizal Fungi in Plant Growth Regulation: Implications in Abiotic Stress Tolerance. Front Plant Sci 10: 1-5.
- Bellenger J, Wichard T, Kustka A(2008) Uptake of molybdenum and vanadium byanitrogen-fixing soil bacterium usingsiderophores.Nature Geosci1: 243-246.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar , Crossref
Citation: Lawrence I (2023) Navigating the Intersection of HIV and Pregnancy:Ensuring Health and Well-Being for Mother and Child. J Comm Pub HealthNursing, 9: 425. DOI: 10.4172/2471-9846.1000425
Copyright: © 2023 Lawrence I. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 624
- [From(publication date): 0-2023 - Mar 12, 2025]
- Breakdown by view type
- HTML page views: 540
- PDF downloads: 84