Nanoparticles: Treatment of Skin Cancer by Topical Drug Delivery
Received: 04-Aug-2022 / Manuscript No. bsh-22-72813 / Editor assigned: 06-Aug-2022 / PreQC No. bsh-22-72813 (PQ) / Reviewed: 20-Aug-2022 / QC No. bsh-22- 72813 / Revised: 23-Aug-2022 / Manuscript No. bsh-22-72813 (R) / Published Date: 30-Aug-2022 DOI: 10.4172/bsh.1000125
Abstract
Nanotechnology involves the engineering of functional systems at nanoscale, thus being attractive for disciplines ranging from materials science to biomedicine. One of the most active research areas of the nanotechnology is Nano medicine, which applies nanotechnology to highly specific medical interventions for prevention, diagnosis, and treatment of diseases, including cancer disease. Over the past two decades, the rapid developments in nanotechnology have allowed the incorporation of multiple therapeutic, sensing, and targeting agents into nanoparticles, for detection, prevention, and treatment of cancer diseases. Nanoparticles offer many advantages as drug carrier systems since they can improve the solubility of poorly water-soluble drugs, modify pharmacokinetics, increase drug half-life by reducing immunogenicity, improve bioavailability, and diminish drug metabolism. They can also enable a tunable release of therapeutic compounds and the simultaneous delivery of two or more drugs for combination therapy. In this review, we discuss the recent advances in the use of different types of nanoparticles for systemic and topical drug delivery in the treatment of skin cancer. In particular, the progress in the treatment with Nano carriers of basal cell carcinoma, squamous cell carcinoma, and melanoma has been reported.
Keywords
Nano medicine; Nanoparticles; Cancer diseases; Immunogenicity
Introduction
Nanotechnology is a generalization for techniques, materials, and equipment that operate at the nanoscale. It is a revolutionary approach that consists of the design, characterization, preparation, and application of structures, devices, and systems by controlling shape and size at the nanoscale [1]. According to the federal US research and development program agency, the National Nanotechnology Initiative (NNI), nanotechnology involves the development of carrier’s devices or systems sized in 1 to 100 nm ranges although this limit can be extended up to 1000 nm. These biomimetic features, together with their high surface-to-volume ratio and the possibility of modulating their properties, raised the interest of the use in biomedical application with potential applications in imaging, diagnosis, and therapy.
Over the past two decades, the rapid developments in nanotechnology have allowed the incorporation of multiple therapeutic [2], sensing, and targeting agents into nanoparticles, for detection, prevention, and treatment of oncologic diseases.
Nano medicine has an enormous potential to improve the selectivity in targeting neoplastic cells by allowing the preferential delivery of drugs to tumors owing to the enhanced permeability and retention effect (EPR). Furthermore, specific binding of drugs to targets in cancer cells or the tumor microenvironment increases the effectiveness of the specific treatment of cancer cells, while leaving healthy cells intact. Nanoparticles (NP) can also improve the solubility of poorly watersoluble drugs, modify pharmacokinetics, increase drug half-life by reducing immunogenicity, improve bioavailability, and diminish drug metabolism [3]. They can also enable a tunable release of therapeutic compounds and the simultaneous delivery of two or more drugs for combination therapy. In addition, by reducing the drug doses, it is also possible to reduce side effects and ameliorate the patients’ compliance. These engineered Nano carriers offer also the opportunity to use the combination of imaging and drug therapy to monitor effects in real time, as well as the possibility to join the delivery of drug with energy (heat, light, and sound) for synergistic anticancer therapeutic effects.
Although skin cancer is not the most mortal form of cancers, it is the most common form of malignancy in the United States and many other countries. Melanoma represents only a very small proportion of skin cancer incidence, but it accounts for the vast majority of skin cancer deaths. Indeed, at the early stage, melanoma can be surgically removed, with a survival rate of 99%, while metastasized melanoma causes the death of 80% of patients within 5 years from the diagnosis. Other types of skin cancers, basal cell carcinoma and squamous cell carcinoma, are the most common diseases. Excision is the gold standard treatment for these localized diseases. However, in very rare cases, they can diffuse to regional lymph nodes and distant sites. For metastasized skin cancers, nanoparticles provide an effective drug delivery system, allowing anticancer drugs to reach the cancer site specifically and, thus, greatly improve treatment efficacy [4]. In the following sections, we illustrated the major forms of nanoparticles which have been used for systemic and transdermal drug delivery in skin cancers and the specific drugnanoparticles formulations which have been reported for the treatment of basal cell carcinoma, squamous cell carcinoma, and melanoma.
Chemicophysical Characteristics of Nanoparticles Employed for Drug Delivery in Skin Cancers
Many nanoparticles have been studied for the treatment of skin cancers, especially in melanoma treatment, including liposomes, dendrimers, polymerases, carbon-based nanoparticles, inorganic nanoparticles, and protein-based nanoparticles. In the following paragraphs, the characteristics of the common nanoparticles used in skin cancer treatment are described. The aqueous core can be used for encapsulation of water-soluble drugs, whereas the lipid bilayers may retain hydrophobic or amphiphilic compounds. To escape from reticuloendothelial system (RES) uptake after i.e. injection, PEGylated liposomes, “stealth liposomes,” were developed for reducing clearance and prolonging circulation half-life [5]. Liposomes show excellent circulation, penetration, and diffusion properties. The possibility to link the liposomes surface with ligands and/or polymers increases significantly the drug delivery specificity. Early research demonstrated that liposomes remain in the tumor interstitial fluid just near the tumor vessels. Currently, several liposomal formulations in the clinical practice contain several drugs for the treating of different types of cancer, including melanoma. Several other liposomal chemotherapeutic drugs are at the various stages of clinical trials. Moreover, advances with cationic liposomes led to the successful delivery of small interfering RNA (siRNA). Liposomes can also be modified to incorporate a magnetic element for use in monitoring their movement within the body using MRI or to entrap gases and drugs for ultrasound-controlled drug delivery.
Transdermal Drug Delivery Nanoparticles in Skin Cancers
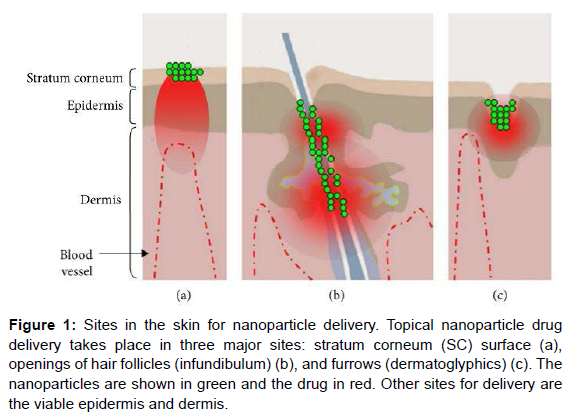
Most chemotherapeutics are administered systemically and are cytotoxic to healthy cells; therefore, cancer patients must endure considerable morbidity. The topical administration of anticancer drugs is an interesting alternative for increasing drug targeting and therapeutic benefits (Figure 1); the major challenge of this kind of treatment is to increase penetration of the antineoplastic tumor drug in sufficient levels to kill tumor cells. Several techniques such as the use of chemical enhancers and the application of an electric field have, therefore, been developed to successfully overcome skin barriers and to reach skin malignancies by favouring drug penetration into the deep layers of the epidermis [6]. The use of chemical penetration enhancers. Is the simplest strategy, causing temporary and reversible disruption of the stratum corneum and leading to increased anticancer drug penetration into the tumor. Moreover, great interest has been shown in nanoparticles delivery systems that can protect anticancer drugs against degradation and, combined with physical methods, significantly increase the tumor penetration of the drugs.
Figure 1: Sites in the skin for nanoparticle delivery. Topical nanoparticle drug delivery takes place in three major sites: stratum corneum (SC) surface (a), openings of hair follicles (infundibulum) (b), and furrows (dermatoglyphics) (c). The nanoparticles are shown in green and the drug in red. Other sites for delivery are the viable epidermis and dermis.
These therapies are used to treat no melanoma skin cancers and their precursor lesions, such as actinic keratosis. Nano carriers could improve skin targeting, improving the drug’s ability to reach and penetrate into tumor cells. Moreover, Nano carriers can improve drug stability and reduce skin irritation by avoiding direct contact of the drug with the skin’s surface. As indicated before, liposomes are one of the most studied Nano carriers for the treatment of cancer.
They are colloidal particles composed of one or several lipid bilayers. Biocompatible with the stratum corneum, increasing the liposome’s affinity for the skin and making them able to release drugs directly to this membrane [7]. Liposomes containing doxorubicin, cisplatin, oxaliplatin, camptothecin, and others have been shown to increase these drugs’ cytotoxicity and to reduce side effects because of direct targeting. Cationic ultra deformable liposomes have also been shown to increase ALA skin permeability in vitro. In vivo, these liposomes result in persistent ALA retention in the skin and induce the production of high levels of PpIX. ALA skin retention was also improved when a traditional ALA containing liposome was examined in vitro. In addition to these ALA studies, 5-fluorouracilloaded noisome (noisome are nonionic surfactant vesicles with a similar structure to liposomes) showed an 8-fold improvement of this drug’s cytotoxicity and penetration when compared to the aqueous solution.
The most investigated nanoparticles for topical delivery are solidlipid nanoparticles and polymeric nanoparticles, such as those made from poly (dl-lactic acid) (PLA), poly (lactic-co-glycolic acid) (PLGA), and poly-��-caprolactone (PCL). Both SLNs and polymeric nanoparticles have been shown to promote sustained drug release and protection against drug degradation when topically applied [8]. In addition, they allow for modifications to matrix softness. It appears that nanoparticles can closely contact the superficial junctions of corneocyte clusters and furrows, possibly favoring drug accumulation for several hours. This would allow for the sustained release of anticancer drugs. However, there are controversies regarding the ideal mean diameter, flexibility, and superficial charge of nanoparticles to optimize skin penetration. In conclusion, Nano carriers appear to be promising systems because they offer several advantages, such as low skin irritation and increased protection of encapsulated drug. An especially important advantage of these formulations is that they often increase anticancer drug penetration through the skin. The use of physical methods to improve the penetration of Nano carriers should be considered to increase the anticancer drug’s penetration into the skin and to provide for targeted drug release inside tumor cells.
Drug Delivery Nanoparticles in No melanoma Skin Cancers: Squamous and Basal Cell Carcinomas Among the three main types of skin cancer: melanoma, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC), BCC is the most common form, with an incidence rate that is 4 to 5 times more likely than SCC. However SCC is a common disease also, with a prevalence of more than 700,000 cases each year in the United States. The risk of development of sporadic skin malignancies has been linked to ultraviolet radiation exposure, skin type, family history, prior history of skin tumors, and immunosuppression. However, a variety of hereditary syndromes can result in an increased risk of developing skin tumors, including nevoid BCC syndrome and xeroderma pigment sum. Excision is the gold standard treatment for localized SSC and BBC. This can be obtained through curettage and desiccation, surgical excision, radiation therapy, cryosurgery, Mohs micrographic surgery, and micrographic surgery [9].
Although the majority of SCC and BCC remain locally invasive, 1 to 5% of primary SCC may diffuse to regional lymph nodes and distant sites, such as lungs, liver, brain, and other areas of the skin. On the other hand, although very rare, BCC can metastasize to distant sites of the body, which is considered a terminal condition.
In the case of SCC, a topical 5-fluorouracil (5-Fu) treatment is widely used when other treatments are impractical and for patients who refuse surgical treatment. It is particularly useful for situations in which postoperative healing is impaired, such as lesions that involve the lower limb in elderly patients or those with venous stasis disease.
To improve the penetration of 5-Fu and reduce many negative side effects of conventionally used chemotherapy drugs and control the release of the therapeutic agent, albumin/drug loaded magnetic Nano composite spheres carrying 5-Fu were prepared [10]. Although these compounds have only been granted licenses for the treatment of actinic keratosis, the main clinical application has been in the treatment of non melanomatous skin lesions, mainly for basal cell carcinoma using a topical application. However, due to the hydrophilic nature of ALA, ALA-PDT has been hindered by the rate of ALA uptake into neoplastic cells and its limited penetration into tissue. A first attempt has already been performed by using liposome to better deliver ALA to the deep layers of epidermis.
ALA loaded nanoparticles were also prepared by using chitosan, a linear polymer composed of 2-amino-2-deoxy-��-D-glucan by glycosidic linkages. ALA has also been carried by succinate-modified chitosan (SCHI), physically complexed with folic-acid-modified chitosan, to improve drug penetration and release in the cellular lysosome. Since it has been demonstrated that the inhibition of SHhsignaling can inhibit BCC tumor growth, diverse small molecule inhibitors of specific SHh signals are under study for the BCC targeted therapy [11]. However, until now, the nanoparticle-encapsulated inhibitor of the transcription factor, Gli1 (Nano HHI) belonging to the SHh pathway, has been used only in “in vitro” and “in vivo” models of human hepatic carcinoma (HCCs). In these models, Gli1 inhibition through Nano HHI has profound tumor growth inhibition and ant metastatic effects.
Drug Delivery Nano systems in Melanoma
At present, the most common drug used for the treatment of melanoma is dacarbazine (DTIC), which is a US Food and Drug Administration- (FDA-) approved, first-line treatment for patients with melanomas. The median survival time of patients with metastasized melanoma is only 6−10 months, and the 5-year survival rate is less than 20%. Therefore, improved treatment efficiency is urgently needed for melanoma. As discussed above, many nanoparticles have been studied for the treatment of melanoma, including liposomes, dendrimers, polymerases, carbon-based nanoparticles, inorganic nanoparticles, and protein-based nanoparticles. It has been shown that delivering the chemotherapeutic agent doxorubicin by gold nanoparticles was very effective against a melanoma cell line. Lo Prete et al. applied a cholesterol-rich Nano emulsion to deliver etoposide in a mouse model of melanoma. It decreased side effects, increasing maximum tolerated dose fivefold, and increased the inhibition of tumor growth by concentrating etoposide at the tumor site (a fourfold higher concentration in tumor than with free etoposide). Doxorubicin was packed in a nanoparticle with additional antibody against CD44, to specifically target malignant cells [12]. The response rate was 25.6% in the chemotherapy naive cohort and was 8.8% in the previously treated cohort. Despite the severe side effects such as neutropenia, thrombocytopenia, neurosensory problems, fatigue, nausea, and vomiting, the authors found that the addition of bevacizumab to nabpaclitaxel and carboplatin (regimen ABC) shows promising activity in terms of both median progression free survival and overall survival.
Sato et al. designed a magnetite nanoparticle by conjugating N-propionyl-cysteaminyl phenol with magnetite and used this in a B16F1 xenograft mouse model. Electron microscopy demonstrated that this particle appeared only in melanoma cells. It was shown that the melanoma cells were degraded after the application of an external alternating magnetic field to increase the temperature in the tumor to 43∘C. The nanoparticle had a 1.7- to 5.4-fold greater effect than the used alone magnetite did [13, 14]. A recent study showed that curcumin further increased the efficacy of magnetite nanoparticles.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Singh R, Lillard JW (2009) “Nanoparticle-based targeted drug delivery”. Exp Mol Pathol 86(3):215–223.
- Bharali DJ, Khalil M, Gurbuz M, Simone TM, Mousa SA (2009) “Nanoparticles and cancer therapy: a concise review with emphasis on dendrimers”. Int J Nanomed 4(1): pp. 1–7.
- Sanvicens N, Marco MP (2008) “Multifunctional nanoparticles-properties and prospects for their use in human medicine”. Trends Biotechnol 26(8):pp. 425–433.
- Allen TM, Cullis PR (2004) “Drug Delivery Systems: Entering the Mainstream”. Science 303:pp. 1818–1822.
- Emerich DF, Thanos CG (2006) “The pinpoint promise of nanoparticle-based drug delivery and molecular diagnosis”. Biomol Eng 23(4):pp. 171–184.
- Jain R K, Stylianopoulos T (2010) “Delivering Nano medicine to solid tumors”. Nat Rev Clin Oncol 7(11):pp. 653–664.
- Jabr-Milane L S, van Vlerken LE, Yadav S, Amiji MM (2008) “Multi-functional Nano carriers to overcome tumor drug resistance”. Cancer Treat Rev 34(7):pp. 592–602.
- Misaka H, Zachariasb N, Songc Z (2013) “Skin cancer treatment by albumin/5-Fu loaded magnetic nano composite spheres in a mouse model”. J Biotechnol 164 (1):pp. 130– 136.
- Zhang L, Zhang N (2013) “How nanotechnology can enhance docetaxel therapy”. Int J Nanomed 8(1):pp. 2927–2941.
- Torchilin VP (2005) “Recent advances with liposomes as pharmaceutical carriers”. Nat Rev Drug Discov 4(2):pp. 145–160.
- Yuan F, Leunig M, Huang SK, Berk DA, Papahadjopoulos D et al.( 1994) “Micro vascular permeability and interstitial penetration of sterically stabilized (stealth) liposomes in a human tumor xenograft”. Cancer Res 54(13):pp. 3352–3356.
- Slingerland M, Guchelaar H, Gelderblom H (2012) “Liposomal drug formulations in cancer therapy: 15 years along the road”. Drug Discov Today 17:pp. 160–166.
- Yano J, Hirabayashi K, Nakagawa S (2004) “Antitumor activity of small interfering RNA/cationic liposome complex in mouse models of cancer”. Clinical Cancer Res 10(22):pp. 7721–7726.
- Muthu MS, Feng S (2013) “Theranostic liposomes for cancer diagnosis and treatment: Current development and pre-clinical success”. Expert Opin Drug Deliv 10(2):pp. 151– 155.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Wasilewska A (2022) Nanoparticles: Treatment of Skin Cancer by Topical Drug Delivery. Biopolymers Res 6: 125. DOI: 10.4172/bsh.1000125
Copyright: © 2022 Wasilewska A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.