Myiasis of the Tracheostomy Wound: A Case Report with Review of Literature
Received: 12-May-2015 / Accepted Date: 30-Jun-2015 / Published Date: 07-Jul-2015 DOI: 10.4172/2161-119X.1000198
249720Introduction
Myiasis is a parasitic infestation of live human or vertebrate animal tissues or cavities caused by dipterous larvae (maggots) which feed on the host dead or living tissue, liquid body substances or ingested. Human myiasis is extremely rare in Europe and in the developed countries but it is not an uncommon parasitic infestation in the tropics and subtropics, like Indian and African countries.
Flies causing myiasis can be classified into two groups, based on the relationship with their hosts: Obligate parasites, specifically producers of myiasis, can develop only on live hosts; Facultative parasites, their larvae feed primarily on cadavers or vegetables, but can sporadically infest human or animal tissues. Removal of maggots by applying anaesthetic ether and turpentine oil locally on the tissue (in the ratio of 1:4) and careful removal is the best treatment of choice. Myiasis of natural orifices like ear, nose, and oral cavity are more common, but myiasis of tracheostomy wound site is a very rare entity with only 3 literatures published worldwide. This case report discuss the importance of proper health education to the patient regarding the tracheostomy wound care, also the various causes for it and the over way eradication plans.
Case Report
In May 2015, a 57-year-old male attended our outpatient department. He had undergone tracheostomy, 4 months earlier in the department of ENT RG Kar medical college. The patient had an ulcero proliferative growth over the vocal cords narrowing the glottis chink, for which tracheostomy with direct laryngoscopy assisted biopsy was carried out. He opted for radiotherapy as primary modality of treatment. After 4 months the family members noticed a small quantity of blood leaking from the area of tracheostomy tube, with many whitish larvae on the skin around it.
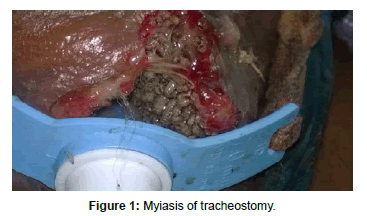
During examination of the tracheotomised patient, we observed many larvae between the tube and the tracheal wall (Figure 1). We considered application of ether for removal of the maggots, as turpentine oil can cause chemical pneumonitis. Patient was taken in the procedure room where antiseptic dressing and draping were done. Ribbon gauge was placed gently and carefully in the area between skin and tracheostomy tube so that it can soak ether. After that ether soaked cotton balls were applied around the tracheostomy coordinating with patient`s respiration so that after application of ether patient exhales. In this method there was minimal inhalation of ether and approximately 30 larvae were removed (Figure 2). At this point, the skin around the tracheostomy was washed again with an antiseptic solution. Special care was taken to avoid removal of the inner tube during change of tracheostomy tube with possible risk of larvae falling in the bronchial tree. The possible consequence would have been pneumonia and live foreign body in airway.
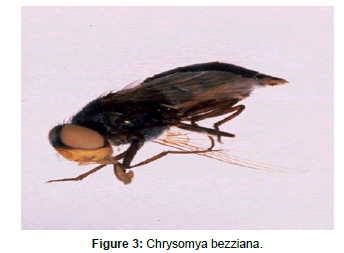
Larvae were placed in containers and taken to the microbiology laboratory. Larvae which developed into adult flies, of both sexes, were dissected and in the laboratory, the microbiologist observed and photographed macroscopic and microscopic characters which are important for species diagnosis. The isolated parasite was identified as coming from the species Chrysomya bezziana (Figure 3).
Discussion
Myiasis was considered, by Hindu mythology, as “God’s punishment of sinners [1]
According to the tropism of the tissue, dipterous larvae are divided into [2]:
a. Cutaneous myiasis: these invading dermo-epidermal layers of the host
b. Myiasis of natural orifices: nose, ear, oral, pharyngeal myiasis;
c. Myiasis with inner migration: larvae migrate inside the body before emerging at skin level.
In our case the predisposing factors for such infestation could be – 1) Extension of laryngeal growth into extra laryngeal tissue and skin; 2) Odour of decomposition that can attract flies; 3) Persistent vegetative state; 4) Poor hygiene, habit of keeping the area uncovered and irregular cleaning of tracheostomy tube. 5) Smaller dimension of the surgical tracheostomy.
According to Sahay [3] the most common months for the myiasis is march to june. This patient also presented in ENT department in the month of May, the commonest genera in india responsible for infection is Chrysomyia [4]. In our case was also the fly was later found to be chrysomyia. Aural myiasis is most common in paediatric age group, whereas nasal myiasis is more common in adult age group [5]. Clearing the maggots with turpentine oil, ether wash and antiseptic dressing is very important.
Hospital admission may be useful to avoid spreading of the tissue lesions or bronco-pulmonary complications since larvae, in the bronchial tree, can behave as a live foreign body. With proper antibiotics, intermittent removal of maggots and regular dressing chances of recurrence are quite less.
Conclusion
Maggot infestation in tracheostomy wound is quite rare even in tropical country like India. Although this is not a lethal disorder, knowledge of this disease is necessary from preventive, diagnostic and curative standpoints. The prognosis is better when there are no associated complications, hospital admission and proper care is very essential. Clearing the maggots with ether meticulously, tracheostomy care and treatment of underlying disease is very vital. It is also important to send the larvae for culture to classify the generic group. This case is described because to keep in mind that with proper care, the condition can be controlled and cured. Myiasis of tracheostomy wound site needs special care at home as well as at hospital. Proper patient education about tracheostomy care, habit of regular cleaning and keeping the area covered is essential for prevention of this problem and judicious intervention with proper knowledge of the surrounding airway and disease process is needed to treat such a case.
References
- Bosmia AN, Zimmermann TM, Griessenauer CJ, Shane Tubbs R, Rosenthal ELÂ (2014) Nasal myiasis in Hinduism and contemporary otorhinolaryngology. J Relig Health.
- Lakshmi Kant Sahay(1959) study of maggots and their otorhinolaryngeal manifestations. Indian journal of otolaryngology 11:146-168.
- Shakeel M, Khan I, Ahmad I, Iqbal Z, Hasan SA (2013) Unusualpseudomyiasis with Muscadomestica (housefly) larvae in a tracheostomy wound: a case report and literature review. Ear Nose Throat J 92: E38-41.
- BlejterJ (2012) TracheostomyWoundMyiasis in a Child: Case Report and Review of the Literature. Case Reports in Pediatrics.
Citation: Manickam A, Sengupta S, Saha J, Basu SK, Das JR, et al. (2015) Myiasis of the Tracheostomy Wound: A Case Report with Review of Literature. Otolaryngology 5:198. DOI: 10.4172/2161-119X.1000198
Copyright: © 2015 Manickam A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 18802
- [From(publication date): 7-2015 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 14042
- PDF downloads: 4760