Research Article Open Access
Multiple Case Study to Describe Influencing Factors on Effectiveness of an Interdisciplinary In-Patient Intervention for Feeding Problems in Children
Lianne Remijn1,2*, Renée Speyer3,4, Pétri CM Holtus1,2, Jacques van Limbeek5 and Maria WG Nijhuis - van der Sanden61HAN University of Applied Sciences, Institute of Health Studies, Postbox 6960 6503 GL Nijmegen, the Netherlands
2Sint Maartenskliniek Research, Postbox 9011, 6500 GM Nijmegen, the Netherlands
3School of Public Health, Tropical Medicine and Rehabilitation Sciences, James Cook University, Townsville City, Queensland 4811, Australia
4Department of Otorhinolaryngology and Head and Neck Surgery, Leiden University Medical Center, Postbox 9600, 2300 RC Leiden, the Netherlands
5Achmea Health Insurance Company, Postbox 1717, 3800 BS Amersfoort, the Netherlands
6Radboud University Medical Center, Radboud Institute for Health Sciences, IQ healthcare, Postbox 9101, 6500 HB Nijmegen, the Netherlands
- *Corresponding Author:
- Lianne Remijn
HAN University of Applied Sciences
Institute of Health StudiesPostbox 69606503 GLNijmegen, the Netherlands
Tel: +31 24 3531320
E-mail: lianne.remijn@han.nl
Received Date: January 07, 2015; Accepted Date: January 29, 2015; Published Date: February 5, 2015
Citation:Remijn L,Speyer R, Holtus PC, Limbeek JV, Nijhuis MWG, et al. (2015) Multiple Case Study to Describe Influencing Factors on Effectiveness of an Interdisciplinary In-Patient Intervention for Feeding Problems in Children. J Child Adolesc Behav 3:184.doi:10.4172/2375-4494.1000184
Copyright: ©2015 Remijn L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Abstract In children with chronic feeding problems diagnoses and physical, cognitive and behavioral impairments vary enormous. In addition to these variables, we hypothesize that personal and environmental factors also contribute to the success of intervention for feeding problems. This exploratory study describes the effectiveness and influencing factors of an intensive, multidisciplinary child and parent centered intervention on calorie intake and solid food consumption. The intervention included a behavioral program, oral motor training, parental coaching and dietary support. The children participating in the intervention could be separated into three groups: tube-fed (n=12), selective food refusal by texture (n=6) and unpredictable food refusal (n=11). For each group we present a descriptive representative case study. Outcome measures were calorie intake and amount of solid food consumed. The average duration of the in-patient feeding intervention was 4.3 weeks (SD 1.4 weeks). Three months after discharge, 50% of the children receiving tube feeding had complete oral intake. Children with selective food refusal by texture made small progresses during the intervention but solid food intake had increased at follow-up. Children with unpredictable food refusal increased their oral intake already during the intervention and maintained these gains at home. The intensive interdisciplinary intervention showed increased calorie and oral intake in most children and reduced tube feeding, but was less successful in children with metabolic dysfunction. Recovery time was longest in the tube feeding group but results varied considerably per child. Successful feeding intervention in children needs to take into account a child's underlying physical and behavioral and environmental factors.
Keywords
Children; Feeding problems; Interdisciplinary intervention; Nutrition; In-patient program; Family centered program
Introduction
The clinical manifestation of feeding problems in children varies from selective food refusal to dysphagia [1-4]. With an incidence of 25 to 35 percent, minor feeding problems are common in early childhood for otherwise healthy children; for children with chronic medical problems, however, the incidence is 40 to 80 percent e.g. [5,6]. The impact of feeding problems on a child’s health ranges from mild to considerable and the relationship between food consumption and long-term health outcomes has become increasingly evident. Early feeding experiences are related to dietary preferences in later life and modulate intake and nutritional status [7-10].
Authors suggest an interaction between oral-motor factors, behavioral issues and environmental factors [11-13]. A child’s refusal to eat results in inadequate development of oral motor skills (e.g. chewing) and this prevents the child from advancing to food textures appropriate to the child’s age [14]. Moreover, inadequate oral motor abilities cause reduced food intake resulting in a significant proportion of malnourished children with neurodevelopmental disorders [15,16]. A child’s feeding disorder also has implications on the child’s family [3,12,17-19]. Parents of children with feeding problems report more stress with regard to social isolation and self-perception than parents of healthy children [20]. Meals and meal preparation take considerable time and result in less time for social activities or for the parent to fulfill developmental activities with the child.
.Several interdisciplinary interventions for children with feeding problems exist [4,22,23]. Although behavioral-based interventions shown positive results in children with developmental disabilities, they have not succeeded in improving oral motor skills in such a way that all food consistencies could be eaten [4,11,13,24]. Likewise, oral-motor based programs do not address the behavioral aspect of the feeding disorder [25,26]. Therefore, it seems appropriate to combine the two approaches in a behavioral-based intervention with oral-motor based elements. To do this, a systematic problem analysis should be the basis for designing a tailored intervention plan.
Such a systematic problem analysis should be based on both child specific problems as well as problems in the environmental conditions. The International Classification of Functioning, Disability and Health version Child and Youth (ICF-CY) of the World Health Organization [21] provides a framework to describe feeding difficulties along four dimensions: (1) Body Function/Structures [gastrointestinal conditions, respiratory status and/or neuromuscular conditions]; (2) Activity and Participation [eating, drinking, learning]; (3) Environmental Factors [parental reaction to the child’s food refusal] and (4) Personal Factors [developmental issues, age]. This framework is helpful in both clinical practice and in research to analyze the complexity of feeding problems in children with feeding problems with various etiologies.
The purpose of this multiple-case report is to describe the characteristics of children with feeding problems using the ICF framework and to get insight in the influencing factors and the effectiveness of the interdisciplinary problem analysis and in-patient intervention to improve calorie intake and solid food consumption.
Methods
Participants
Children aged six months to six years were eligible for the intervention when (i) feeding difficulties had existed for a period of at least six months and (ii) feeding difficulties were related to physical etiology and/or were affecting the child’s health status. Children with diagnosed psychiatric problems or severe developmental disabilities or children in palliative care were excluded from this study. We categorized the children into three groups depending on how the parents characterized the feeding problem. Of the 29 children, 41% were categorized as ‘Tube feeding’ (n = 12; 9 nasogastric tube and 3 gastrostomy tube), 21% were categorized as ‘Selective food refusal by texture’ (n = 6) and 38% were categorized as ‘Unpredictable food refusal’ (n=11). Characteristics of the participants are listed in Table 1.
| ‘Tube feeding’ | ‘Selective food refusal by texture’ | ‘Unpredict able food refusal’ | Total | ||
|---|---|---|---|---|---|
| n (%) | 12 (41%) | 6 (21%) | 11 (38%) | 29 (100%) | |
| Age in years Mean (SD) | 2.3 (0.9) | 3.5 (1.9) | 2.5 (1.3) | 2.5 (1.4) | |
| Gender | Boys (n) | 8 | 5 | 3 | 16 (55%) |
| Girls (n) | 4 | 1 | 8 | 13 (45%) | |
| Weight (SD) |
Mean (SD) | -1.4 (1.3) | -1.2 (1.4) | -1.9 (1.0) | -1.5 (1.2) |
| Range | -3.6 to 0.5 | -3.0 to 0.5 | -4.0 to -1.0 | -4.0 to 0.5 | |
| Height (SD) |
Mean (SD) | -0.4 (1.1) | -1.0 (1.1) | -1.1 (0.7) | -0.8 (1.0) |
| Range | -1.7 to 2.7 | -2.4 to 0,5 | -2.0 to -0.1 | -2.4 to 2.7 | |
| Weight for Height(SD) | Mean (SD) | -1.3 (1.3) | -0.3 (2.2) | -0.9 (1.4) | 0.9 (1.6) |
| Range | -3.2 to 1.9 | -2.4 to 2.6 | -3.7 to 2.1 | -3.7 to 2.6 | |
Table 1: Characteristics of the participating children.
In each subsection of this article we present a representative case study per group.
‘Tube feeding’
B. was a 1.6 years old girl with multiple respiratory problems, kidney dysfunction and delayed psychomotor development. At birth she presented with severe feeding problems and a nasogastric tube was used for feeding. Vomiting occurred at least twice a day. B. refused food by screaming and holding her breath. B.’s parents ceased feeding when B. started crying or vomiting. Because of the dependence of the tube feeding the parents were unable to enroll B. in a childcare facility and the mother had to resign from her job, which resulted in financial problems for the family.
Anthropometric data: SD of age-appropriate height was -2.9, SD of age-appropriate weight was -2.2 and SD weight for height was -0.3.
‘Selective food refusal by texture’
J. was a 5.5 years old boy with unilateral cerebral palsy and mild developmental problems. He was referred for intervention to optimize his intake of solid and lumpy foods. He took medication for constipation. His parents reported long mealtimes, especially diners, where J. was often angry and went into a rage. Parents reported that family meals were stressful for both them and their three children. J’s parents also reported that they were inconsistent in their use of incentives to encourage J. to eat solid foods.
J. showed hyposensitivity and hypotonicity of his mouth. He could make limited discrete movements with his tongue and movements were asymmetric. When observing him eating bread, he showed minimal chewing and he gagged when swallowing the piece of bread. Chewing a piece of hamburger took a long time and in the end J. removed the meat out of his mouth. Although his daily calorie intake was appropriate for his age, his diet consisted of excessive milk and sugar products and limited fiber. J. had normal anthropometric data.
‘Unpredictable food refusal’
M. was a 2.5 years old girl with no medical problems except multiple middle ear infections during her first year of life. Her food intake was supplemented with a drink and a powder for 50% of her daily intake. Feeding sessions took a large part of the day. M. was the only child in the family. Her parents reported not knowing how to cope with M.’s food refusal and that M. slept twice a day for three hours at a time. In addition to food refusal M. showed limited interaction with peers and had an aversion to being affectionate.
Despite food supplements, M.’s fluid intake was only 40% and her calorie intake was 80% of the recommended amount. M. was pale and thin and had blue circles under her eyes. Anthropometrics data; SD of age-appropriate height was -0.77, SD of age-appropriate weight was -2.7 and SD weight for height was -2.0.
Setting and Materials
In this exploratory multiple case study data was obtained from 29 children participating in an in-patient feeding intervention at the rehabilitation centre of the Sint Maartenskliniek (Nijmegen, the Netherlands). Therapy sessions lasted 45-60 minutes (inclusive parental instructions) and were held three or four times a day based on the intervention of Clawson et al. [26]. The weekdays feeding intervention varied per child between four to six weeks depending on individual factors (e.g. intervention goal, child’s physical condition, progression in oral intake and parent-child interaction and personal or environmental factors) [24]. The feeding sessions were held in a room by the psychological trainer or speech therapist. Between therapy sessions the children played with peers.
Materials used in the feeding sessions were plastic children’s tableware, regularly available foods and drinks for children, calorie supplements and interactive toys or internet applications with sound and moving elements.
Procedure
Clinical assessment
After enrolling in the centre, parents were requested to keep a diary of their child’s oral intake for seven days and to make a video recording of a representative mealtime with the family. At the assessment, a pediatrician, psychologist, speech therapist and dietician collected data related to each child’s physical and cognitive development, feeding history, current oral motor skills and current food intake. This data was obtained by using three questionnaires (Child Behavior Checklist, Caregiver-Teacher Report Form and Sensory Profile-NL), analysis of the diary and physical examination by the pediatrician and speech therapist. The Child Behavior Checklist for ages 1½-5 is a questionnaire for parents with 99 items concerning behavioral and emotional problems of their child [27]. The Caregiver- Teacher Report Form for ages 1½-5 has 99 items concerning behavioral and emotional problems of the child [27]. The Sensory Profile-NL contains 125 items on processing sensory stimulus in everyday situations [28]. Anthropometric data (weight and height) were also collected and compared with growth curves for diagnose, gender and cultural background.
Parents were also interviewed and asked about their thoughts and expectations about the intervention. The mealtime recording was analyzed by the psychologist in terms of the child’s feeding-related behavior and family members’ reactions to the child’s behavior. Each child’s assessment was distributed over a single day After data analysis the team met and used the ICF framework to determine the body functions, activities, environmental and personal factors. This information was used to formulate a hypothesis on the reasons for the feeding problem and the factors continuing the feeding problem. An overview of this analysis in terms of the ICF framework is illustrated in Table 2.
| ICF code | Description | ‘Tube feeding’ | ‘Food refusal by texture’ | ‘Unpredictable food refusal’ | Total | |
|---|---|---|---|---|---|---|
| Body function | n=12 | n=6 | n=11 | n=29 | ||
| b 117/ b147 | Intellectual functions/ psychomotor function | 4/12 | 2/6 | 1/11 | 7/29 | |
| b 122 | Global psychosocial function | 1/12 | 2/6 | 3/11 | 6/29 | |
| b 125 | Dispositions and accomodation | 4/12 | 1/6 | 9/11* | 14/29 | |
| b 126 | Temperament and personality functions | 6/12 | 3/6 | 4/11 | 13/29 | |
| b 130 | Energy and drives functions | 6/12* | 1/6 | 1/11 | 8/29 | |
| b 134 | Sleep functions | 1/12 | 6/11* | 7/29 | ||
| b 140 | Attention functions | 1/12 | 3/6* | 2/11 | 6/29 | |
| b 152 | Emotional functions | 5/12 | 3/6 | 7/11 | 15/29 | |
| b 250/ b270 | Taste/Sensory function related to temperature and other stimuli | 7/12 | 1/6 | 9/11 | 17/29 | |
| b 280 | Pain | 3/12* | 1/11 | 4/29 | ||
| b 435 | Immunological system function | 5/12 | 4/11 | 9/29 | ||
| b 510 | Ingestion functions | 6/12 | 6/6* | 7/11 | 19/29 | |
| b 515 | Digestive functions | 4/12 | 3/11 | 7/29 | ||
| b 525 | Defecation | 3/12 | 3/6 | 4/11 | 10/29 | |
| b 735 | Muscle tone function | 1/12 | 1/6 | 2/29 | ||
| b 760 | Control of voluntary movement functions | 2/12 | 3/6* | 5/29 | ||
| b 761 | Spontaneous movement functions | 1/12 | 2/6 | 1/11 | 4/29 | |
| Body structures | ||||||
| s 250 | Structure of middle ear | 3/11* | 3/29 | |||
| s 330 | Structure of pharynx | 1/12 | 2/6 | 4/11* | 7/29 | |
| Activities/participation | ||||||
| d 250 | Handling psychological demands | 2/12 | 1/6 | 7/11* | 10/29 | |
| d 330 | Speaking | 3/12 | 2/6 | 1/11 | 6/29 | |
| d 550 | Eating | 7/12 | 4/6 | 7/11 | 18/29 | |
| d 560 | Drinking | 4/12 | 1/6 | 1/11 | 6/29 | |
| d 710 | Basic interpersonal interactions | 1/12 | 1/6 | 6/11* | 8/29 | |
| d 815 | Preschool education | 2/12* | 2/29 | |||
| Enviromental factors | ||||||
| e 110 | Products or substances for personal consumption | 3/6 | 5/11 | 8/29 | ||
| e 310 | Immediate family | 3/12 | 1/6 | 8/11* | 12/29 | |
| e 410 | Individual attitudes of immediate family members | 8/12 | 2/6 | 10/11* | 20/29 | |
| e 580 | Health services, systems and policies | 12/12* | 2/6 | 1/11 | 15/29 | |
| Personal factors | ||||||
| age/ negative experiences/ not feeling well /refusal behavior | 9/12 | 1/6 | 10/11 | 20/29 | ||
Table 2: Overview of signs and symptoms classified conform the International Classification of Functioning, Disability and Health (ICF ) per feeding group.
‘Tube feeding’
Team’s conclusion: B. was a girl with a complicated medical history resulting in tube feeding but at presentation was in a healthy state. She was small and thin but had a sufficient height and weight for her age. The girl had missed the critical period for oral feeding [10,29,30] and lacked the ability to eat a variety of tastes and consistencies. B. was used to getting attention from her family in periods of distress. B.’s parents were anxious about giving her food because of previous vomiting and breath holding.
The goal of the 4-week behavioral intervention therapy was to reduce B.’s food refusal behavior and reduce the amount of tube feeding.
‘Selective food refusal by texture’
Team’s conclusion: J. was a boy with partial food refusal caused by oral motor problems related to neurological disease and inconsistent use of strategies by J.’s parents to encourage J. to eat.
The goals of the 4-week oral-motor therapy were to teach J. to chew on soft and hard foods, to structure the mealtimes by using behavioral techniques and to optimize J.’s intestines by changing the quality of his food intake.
‘Unpredictable food refusal’
Team’s conclusion: M. was a malnourished girl with no energy level. M. had no impairments of body functions. The strong-willed girl had learned to avoid food and drinks and her parents were unable to cope with her behavior during feeding.
The goal of the 4-week therapy was to improve M.’s nutritional status using a maximum of food supplements and to reduce M.’s food avoidance by using the behavioral intervention.
Feeding intervention
The intervention consisted of a behavioral program given by a psychologist, an oral-motor program given by a speech therapist or a combination of both programs given by both the psychologist and the speech therapist. The behavioral program was based on the studies by de [13,15,24] and included positive reinforcement, tangible rewards (non-contingent access to preferred items), extinction of inappropriate behaviors and the use of shaping and fading techniques. During the behavioral therapy, the child sits on the therapist’s lap and is given a small amount of food just under the child’s current acceptance level. When the child accepts this given amount of food over three consecutive sessions, the amount is increased by 25 grams (if acceptance level was below 100 grams) or 50 grams (if acceptance level was above 100 grams). The child received a tangible reward (e.g. music toy) and/or verbal reward (‘well done’) after every bite in a standardized order.
The focus of the oral-motor program was to practice the oral skills of managing different food consistencies. The child receives standardized verbal instructions with visual and tactile support during the session. Regular contact was maintained between the psychologist, speech therapist and the dietician to ensure each child received optimal and adequate nutrition. Weekly meetings were held with the intervention team and the parents to discuss progress and child nutrition. Parents were taught feeding techniques and strategies on how to manage their child’s food refusal behavior.
Outcome Measures and Data Analysis
Outcome measures
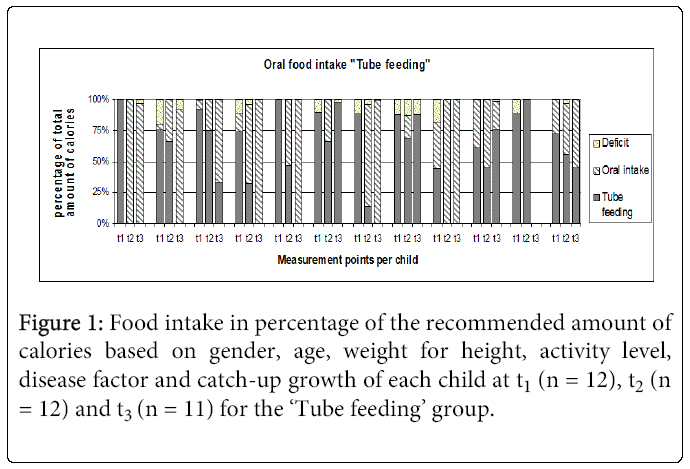
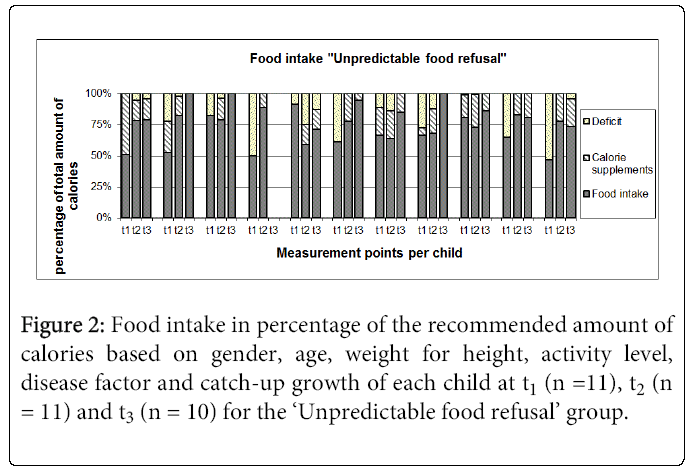
Food intake was derived from the 7-day feeding diary. Average food intake was compared with the recommended amount of calories and fluid based on child gender, age, weight, height, activity level, disease factor and catch-up growth and was calculated by means of the Schofield formula [31]. Data on calorie intake (k.cal) was computed at three measurement moments: the week leading up to the assessment day (t1), the week prior to discharge (t2) and three months after discharge (t3). In addition to calorie intake we also collected groupspecific data: for the ‘Tube feeding’ group we separated calorie consumption into oral intake and tube feeding, for the ‘Unpredictable food refusal’ group we separated calorie consumption into normal oral intake and supplements and for ‘Selective food refusal by texture’ group we separated calorie consumption into the amount of solid, puree and liquid intake (k.cal).
Data analysis
Descriptive statistics were used to describe characteristics of the participating children and to describe the outcome measures of the total group and subgroups. To allow comparison between evaluation moments and between participants, we transformed the change in calorie intake per group into z-scores. All statistics were performed using SPSS (version 17.1).
Results
Treatment frequency and duration
The mean duration of the intervention was 4.3 weeks (60.7 therapy sessions). The ‘Tube feeding’ group received the most therapy sessions (mean 66.9) and the ‘Selective food refusal by texture’ group had the fewest number sessions (mean 51.0). Frequency data for the ‘Unpredictable food refusal’ group are skewed as two children had an extended stay in the in-patient intervention due to family factors (inappropriate home environment and parental psychiatric problems). The parental coaching sessions are included in the count but sessions with the dietician are not included.
Tube feeding
Before the intervention, 12 children required tube feeding for 20 to 100% of their dietary needs. At discharge two of these children were no longer receiving tube feeding and at follow-up another four children had ceased receiving tube feeding. The remaining five children (follow-up data of one child is missing) received (partial) tube feeding at follow-up (range= 30-90%). Two of them decreased tube feeding by 50 and 75% compared to pre-intervention data. Both these two children had co-morbid medical problems (cardiac defect; multiple congenital malformations of the skeleton, muscles, heart and kidneys). The maximum duration of the feeding sessions was 30 minutes and these two children were often too fatigued to eat the necessary amount. The oral meals were completed with tube feeding to prevent stressful feeding sessions and malnutrition. Three children were not successful in decreasing the tube feeding had metabolic dysfunctions and also gastrointestinal problems with episodes of extreme vomiting. Figure 1 presents the evaluation of the oral feeding.
Calorie intake
Figure 2 presents the information on calorie intake for children with unpredictable food refusal for the period from t1 to t3. In addition to an insufficient calorie intake, some children had a one-sided and incomplete menu at t1. Three months after discharge almost all children had a sufficient calorie intake. However, in 8 cases supplemental calories in powder form were added to food or drinks. The children with selective food refusal by texture generally had a sufficient calorie intake and they showed no significant change in calorie-intake.
The ‘Tube feeding’ group had the largest improvement in calorie intake during the treatment (z-score Δ t1-t2 = 2.3; Δ t2-t3 = 1.1). The ‘Unpredictable food refusal’ group increased their calorie intake after the treatment more than during the treatment (z-score Δ t1-t2 = 0.7; Δ t2-t3 = 1.3). Results at follow-up suggest that parents of both groups were generally able to maintain and even increase the calorie intake at home.
Age appropriate oral intake
Children with selective food refusal by texture could be divided into those who did not accept solid food (n = 4) and those who ate solid and lumpy food but had poor chewing skills due to neurological problems (cerebral palsy, prematurity; n = 2). The therapy for all children in this group was focused on developing chewing technique rather than on increasing the amount of solid food consumed. As a result, the amount of solid food intake during treatment for this group decreased but increased after discharge. At follow-up the amount of solid food being eaten by the 6 children was more than double the preintervention amount (from 115 to 310 grams per day).
ICF framework
We shared the children into three groups based on their specific food intake. Using the ICF classification we noticed differences between the three groups and their environment. The children with tube feeding had physical problems and as result of multiple medical treatments they were anxious about eating. Two of the children in this group were not able to enroll at childcare because of the tube feeding and/or vomiting.
The children with food refusal by texture showed more motor and attention problems and had difficulties with defecation whereas children in the other groups had more vomiting.
The children with unpredictable food refusal had difficulties with psychosocial function, dispositions and accommodation and sleeping. Approximately 30% of these children had multiple ear inflammations, enlarged tonsils or food intolerance. Most parents of children in this group were unable to give clear structure and instructions or provide positive rewards for eating. This resulted in children not participating in family mealtimes and the child having his/her own ritual for eating. In three cases we were concerned about the child’s social emotional development and we referred the child for further assessment.
‘Tube feeding’
B. received 78 sessions during 4.2 weeks of intervention. At t1 B. was 100% dependent on tube feeding and received 800 ml per day via tube feeding, which meant a lack of 100 kcal. B.’s first feeding therapy sessions started with 10 grams of custard and fruit puree. After three successful sessions, the amount was doubled. Her meals were extended with pureed vegetables. After two weeks of the intervention, B.’s parents became involved in the training. The parents were taught how to use firm instructions and how to cope with B.’s refusal behavior. During the weekdays parents were coached in the feeding sessions. In the weekend’s they made video recordings to discuss with the psychologist.
At the end of the intervention, the tube feeding was reduced to 25% and she ate 5 homogenized meals a day. The mealtimes took a maximum of 30 minutes. Three weeks after discharge the feeding tube was permanently removed. B. still required calorie supplements. At follow up, the mealtimes were reasonable in terms of time demands and child behavior, but drinking and non-homogenized consistencies caused substantial refusal behavior. A three-month outpatient intervention with therapy sessions once a week with the speech therapist resulted in adequate calorie and fluid intake in mealtimes.
‘Selective food refusal by texture’
J. received 60 sessions (30 with the speech therapist; 30 with the psychologist) over a period of 4 weeks. At t1 J.’s calorie intake was sufficient but the amount of fluids consumed was 200 ml below the daily recommendation. Starting with crunchy crackers and using visual and auditory feedback, the speech therapist taught J. how to chew. He then learned how to bite off pieces of food, move and extend his tongue laterally and to form a bolus and control a swallow. Due to J.’s oral hyposensitivity, we adapted the foods (e.g. baked instead of boiled potatoes and easy to chew meat). He was rewarded when he finished a meal within 20 minutes. J.’s parents understood the relationship between cerebral palsy and oral motor problems and they accepted the need for J. to have easy-to-chew food. After 4 weeks of intervention, J. ate a cracker before bread and succeeded in finishing his meal within a given time. His consumption of liquids was adequate and the digestive medication had ceased being given. Three months after discharge J.’s parents reported that mealtimes were now cozy and were no longer stressful.
‘Unpredictable food refusal’
M. received 76 sessions over 4 weeks. At first she showed extreme food refusal behavior and tangible rewards were not an effective strategy. M. started with preferred food during three therapy sessions a day. Therapy focused on consuming calorie enriched juices. M. learned to eat custard and puree and to drink 700 ml a day divided over 6 portions. M. often appeared unhappy during the sessions. M. showed limited affection towards her parents. During the inpatient intervention we discussed our observations with the parents. At follow-up M.’s physical condition had improved but mealtimes remained stressful. Parents agreed on referring M. to the psychiatrist for further investigation.
Discussion and conclusion
In this study we described a 4-6 week in-patient multidisciplinary intervention including a behavioral program based on theories of operant conditioning combined with oral motor training, parental coaching and dietary support to be effective for children with feeding problems. For children with severe metabolic disorders was the intervention limited successful to increase oral food intake, but parents reported that their child vomited less and that they had more insight into their child’s oral intake pattern.
The average length of 4-6 week intervention in our study was shorter than in other studies; however, the number of therapy sessions required to reduce tube feeding is in line with these studies [12,23,25]. Parents were unanimously positive about the duration of the 4-6 weeks, possible because of the high frequency of intervention sessions. In the literature, researchers report good results when parents are given a more prominent role in the intervention [26,32] and this fits our findings. We did no systematically analyze the reduction of parental stress, but we hypothesize that providing parental training to transfer intervention elements to the home setting was a key factor for the success of our intervention. The in-patient setting enabled us to observe characteristics of both children and parents in addition to the feeding sessions Parents were taught how to offer their child food, how to reward their child for food acceptance and how to ignore their child’s refusal behavior. By changing the parents’ perception and interpretation of their child’s behavior, parents gained insight into their child’s temperament and how to cope with the conflicts during feeding and during sleeping. Therefore, the primary goal for children with tube feeding was not eliminating the tube feeding as fast as possible, but focused on the capacity of parents to handle the refusal behavior of their child. Success was not limited to type or presence of chronic illness but also to the personal factors of the children, character and coping style as illustrated in the three cases.
Of the 29 children in the present study, 26 made progress in their qualitative as well as in their quantitative food intake. The individual adapted menu with food supplements made by the dietician resulted in clear recommendation and reduced worries about the food intake of their child. In our study, 67% of the children who were receiving tube feeding at admittance to the intervention had reduced the amount of tube feeding by the end of the intervention. Based on our findings it seems that a total reduction of tube feeding in such a heterogeneous group is not to be expected especially in cases with complicated medical issues such as in metabolic illness.
Although we did not quantify the degree of improvement in oral motor skills in children with ‘Selective food refusal by texture’, we found that the average amount of solid food consumed almost trebled for the group at follow-up. The subgroup of children with neurological impairments was able to improve chewing technique, which led to a safer handling of solid and lumpy foods. This is in line with the results published by Clawson et al. [26]. Parents learned to stimulate good chewing and to adapt the meals to the oral motor abilities of their child.
Definite conclusions on the success of the intervention need to be postponed. We tried to handle the heterogeneity of the group in this study by defining subgroups based on the feeding problem instead of based on the diagnosis and found that the degree of physical and behavioral problems differed largely per group. It seemed to be appropriate as the ratio of behavioral and oral-motor program components was linked to the goal of the intervention, but this was also linked to the subgroup profile. This study provides insight for a well-documented much larger cohort study to offer insight into the barriers and facilitators leading to success of the intervention.
Acknowledgements
The authors express their appreciation for the cooperation of the children and their parents during the feeding intervention. We are very grateful to Babette Hermans, dietician, Tessa Broekhuijsen and Dorine van Bentum-Schouwink, psychologists from the Sint Maartenskliniek, for their efforts during the intervention and data collection. We also thank Yvonne Heerkens for her support with the ICF classification.
References
- Field D, Garland M, Williams K (2003) Correlates of specific childhood feeding problems J Paediatr Child Health 39: 299-304.
- Chatoor I, Ganiban J (2003) Food refusal by infants and young children: diagnosis and treatment. CognBehavPract 10: 138-146.
- Arvedson JC (2008) Assessment of pediatric dysphagia and feeding disorders: clinical and instrumental approaches DevDisabil Res Rev 14: 118-127.
- Williams KE, Field DG, Seiverling L (2010) Food refusal in children: a review of the literature Res DevDisabil 31: 625-633.
- Rudolph CD, Link DT (2002) Feeding disorders in infants and children PediatrClin North Am 49: 97-112, vi.
- Manikam R, Perman JA (2000) Pediatric feeding disorders J ClinGastroenterol 30: 34-46.
- Sullivan PB, Juszczak E, Lambert BR, Rose M, Ford-Adams ME, et al. (2002) Impact of feeding problems on nutritional intake and growth: Oxford Feeding Study II Dev Med Child Neurol 44: 461-467.
- Mennella JA, Ventura AK (2011) Early feeding: setting the stage for healthy eating habits Nestle Nutr Workshop SerPediatr Program 68: 153-163.
- Beauchamp GK, Mennella JA (2011) Flavor perception in human infants: development and functional significance Digestion 83 Suppl 1: 1-6.
- Coulthard H, Harris G, Emmett P (2010) Long-term consequences of early fruit and vegetable feeding practices in the United Kingdom Public Health Nutr 13: 2044-2051.
- Burklow KA, McGrath AM, Valerius KS, Rudolph C (2002) Relationship between feeding difficulties, medical complexity, and gestational age NutrClinPract 17: 373-378.
- Greer AJ, Gulotta CS, Masler EA, Laud RB (2008) Caregiver stress and outcomes of children with paediatric feeding disorders treated in an intensive interdisciplinary program. J PediatrPsychol 33: 612-620.
- Vaz PC, Piazza CC (2011) Behavioural approaches to the management of paediatric feeding disorders. In: Southall A, Martin C (Edn.) Feeding Problems in Children; a practical guide: Birmingham: Radcliffe Publishing pp: 53-73.
- Piazza CC (2008) Feeding disorders and behavior: what have we learned? DevDisabil Res Rev 14: 174-181.
- Eckman N, Williams KE, Riegel K, Paul C (2008) Teaching chewing: a structured approach Am J OccupTher 62: 514-521.
- Marchand V (2009) Nutrition in neurologically impaired children. J PediatrGastroenterolNutr 14: 395-401.
- Hewetson R, Singh S (2009) The lived experience of mothers of children with chronic feeding and/or swallowing difficulties Dysphagia 24: 322-332.
- Southall A (2011) Family and wider system perspectives. In: Southall A, Martin C (Eds), Feeding Problems in Children; a practical guide: Birmingham: Radcliffe Publishing pp: 133-151.
- Crist W, Napier-Phillips A (2001) Mealtime behaviors of young children: a comparison of normative and clinical data J DevBehavPediatr 22: 279-286.
- Garro A, Thurman SK, Kerwin ME, Ducette JP (2005) Parent/caregiver stress during pediatric hospitalization for chronic feeding problems J PediatrNurs 20: 268-275.
- World Health Organization (2008) International Classification of Functioning, Disability and Health Children & Youth version (ICF-CY), Geneva.
- Silverman AH (2010) Interdisciplinary care for feeding problems in children NutrClinPract 25: 160-165.
- Sharp WG, Jaquess DL, Morton JF, Herzinger CV (2010) Pediatric feeding disorders: a quantitative synthesis of treatment outcomes Clin Child FamPsychol Rev 13: 348-365.
- de Moor J, Didden R, Korzilius H (2007) Behavioural treatment of severe food refusal in five toddlers with developmental disabilities Child Care Health Dev 33: 670-676.
- Gisel EG (1996) Effect of oral sensorimotor treatment on measures of growth and efficiency of eating in the moderately eating-impaired child with cerebral palsy Dysphagia 11: 48-58.
- Clawson EP, Kuchinski KS, Bach R (2007) Use of behavioural interventions and parent education to address feeding difficulties in young children with spastic diplegic cerebral palsy. NeuroRehabilitation 22: 397-406.
- Verhulst FC, van der Ende J (2003) Dutch translation of Child Behavior Checklist and Caregiver Teacher Report Form. Kinder- en Jeugdpsychiatrie Erasmus Medical Centre – Sophia.
- Dunn W (2006) Sensory Profile-NL (Dutch translation). Pearson Assessment and Information BVAmsterdam.
- Illingworth RS, Lister J (1964) The Critical Or Sensitive Period, With Special Reference To Certain Feeding Problems In Infants And Children J Pediatr 65: 839-848.
- Coulthard H, Harris G2, Fogel A2 (2014) Exposure to vegetable variety in infants weaned at different ages Appetite 78: 89-94.
- Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work Hum NutrClinNutr 39 Suppl 1: 5-41.
- Casey SD, Perrin CJ, Lesser AD, Perrin SH, Casey CL, et al. (2009) Using descriptive assessment in the treatment of bite acceptance and food refusal BehavModif 33: 537-558.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 14483
- [From(publication date):
February-2015 - Dec 19, 2024] - Breakdown by view type
- HTML page views : 10032
- PDF downloads : 4451