Multi-nodular Goiter with Intra-tracheal Thyroid Tissue: Ectopic or Implanted? And Ectopic Nasopharyngeal Thyroid Tissue: A Case Report
Received: 30-Jul-2015 / Accepted Date: 17-Aug-2015 / Published Date: 24-Aug-2015 DOI: 10.4172/2161-119X.1000204
Abstract
We present a case of intra-tracheal thyroid tissue in a 44 year old woman who had been treated for multi-nodular goiter with left thyroidectomy 26 years earlier, the thyroid tissue was found in the trachea lumen which may appears to have been implanted at the time of this operation or it is a case of ectopic thyroid tissue. The patient presented with progressive right thyroid lobe swelling. Clinical examination and investigations were carried out. Right thyroidectomy was performed first, then after discovering in laryngostroboscopy, CT scan and MRI, the presence of intra-tracheal lesion narrowing the airways, patient had another procedure to remove the residual left thyroid lobe and the intra-tracheal tissue which was thyroid tissue as confirmed by histology examination. Post-operative I131 whole body-scan showed ectopic thyroid tissue in nasopharynx and residual tissue in thyroid bed. Currently the patient is free of complaint, but further investigation: SPECT-CT Scan was requested for better localization.
Keywords: Thyroid gland, Ectopic thyroid, Implanted thyroid tissue, Trachea
249895Background
The ectopic thyroid is uncommon with the prevalence rate of approximately 1 per 100,000 – 300,000 persons. More than 440 cases have been reported in Europe, America, and Asia to date [1- 5]. Anatomically, the most common sites of ectopic thyroid tissue are lingual, sublingual, thyroglossal and laryngotracheal. In rare cases, esophageal, mediastinal, cardiac, aortic, adrenal, pancreatic, duodenal, gallbladder, mesentery of the small intestine, cutaneous and intra-tracheal sites have been found [6-15]. There is also unique cases of ectopic thyroid tissue include pituitary fossa, sphenoid sinus and uterus [16-18]. To our knowledge, this is the first case of ectopic nasopharyngeal thyroid tissue have been reported or published to date. Additionally there have been rare reports of Implantation of thyroid tissue following blunt trauma, fine needle aspiration biopsy and endoscopic thyroid surgery [19-23].
Case Presentation
A 44- year- old woman, nonsmoker, presented with progressive painless right sided neck swelling since more than 2 years, on examination she has right thyroid lobe enlargement, freely movable, not fixed to the skin, nodular, diffuse and about 4*4 cm in size, with other complaints of increasing dyspnea and swallowing difficulty since few months, she had been treated for asthma by her general practitioner. 26 years earlier, the patient had been treated for multinodular goiter with left hemi-thyroidectomy with subsequent thyroxin replacement therapy. There is family history of thyroid goiter in her sisters and she is allergic to penicillin. During the current presentation, clinical examination showed painless nodular right thyroid lobe swelling adherent and displacing the trachea, together with tremor, tachycardia and some stridor in deep inspiration, thyroid function tests were normal. Indirect laryngoscopy showed restricted mobility of left vocal cord only. The patient underwent completion thyroidectomy by right hemi-thyroidectomy, during the surgery, there was infiltration of thyroid tissue in between the tracheal rings, and small air leak was detected from trachea after shaving off the thyroid tissue which repaired by using prolene 4-0 suture. Histologically: nodular hyperplasia (multinodular goitre), no evidence of malignancy.
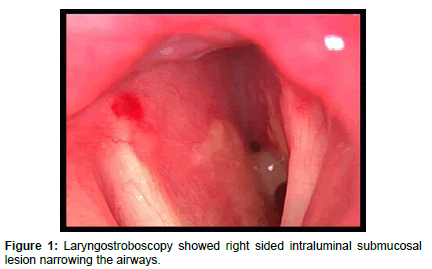
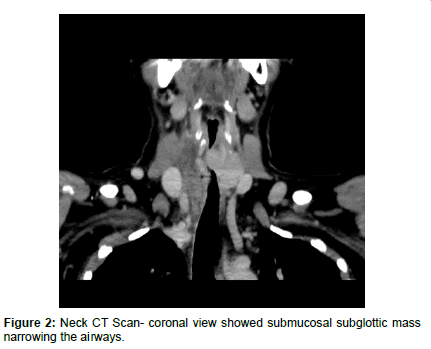
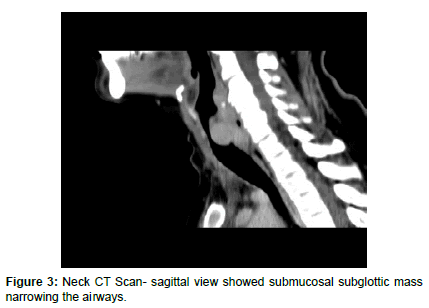
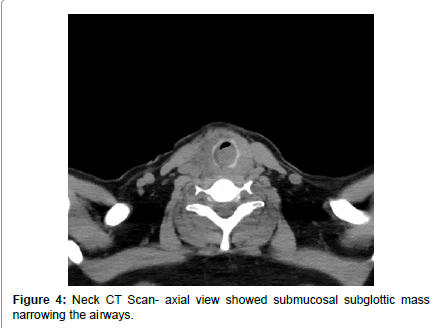
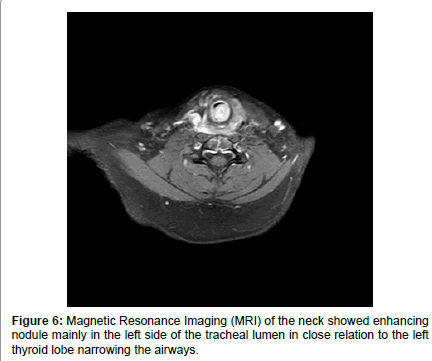
On post-operative first day, patient developed biphasic stridor without any sign of neck swelling or hematoma, laryngostroboscopy showed restricted mobility of left vocal cord and submucosal rounded smooth intraluminal lesion on the right side causing marked narrowing in subglottic area, and this low mobility of left vocal cord can be attributed to the previous surgery on left side (Figure 1). Computed Tomography Scanning of the neck showed submucosal intraluminal mass extending from subglottic area to about the level of third tracheal ring, causing narrowing more than 50% of the airways (Figures 2-5). Magnetic Resonance Imaging (MRI) of the neck showed enhancing nodule mainly in the left side of the tracheal lumen in close relation to the left thyroid lobe, suggestive of either an ectopic thyroid nodule or abnormally implanted thyroid tissue post prior surgeries (Figure 6).
Drain was removed next day, patient still complains of stridor, so patient was planned for excision of the tracheal lesion with or without surgical tracheostomy and tracheal stenting. Surgery was done two days later, starting with surgical tracheostomy and then we were unable to remove the intra-tracheal lesion sub-mucosally using debrider and bronchoscope, so we did an external approach (Laryngofissure) by median cricoidotomy extending through first three tracheal rings, exposing the endo-sublglottis area and endo upper trachea, submucosal removal of lesion, re-approximating and suturing mucosal edges, suturing of cricoid and trachea bu absorbable sutures, following by completion thyroidectomy in left side and finishing by closure of tracheostomy, frozen section of this intra-tracheal lesion confirmed thyroid tissue.
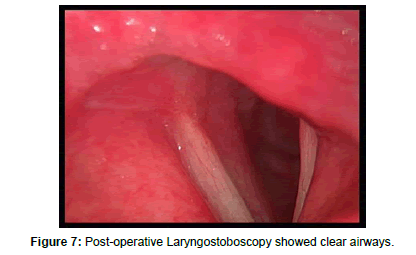
Following surgery, the patient was kept intubated in ICU for 6 days to keep endotracheal tube in place as a stent, and then Microlaryngotracheoscopy under general anesthesia was done and revealed patent airways so patient was extubated with uneventful postoperative course without any stridor or respiration difficulty, patient was discharged few days later. Endoscopic control after two weeks showed fixed left vocal cord, mobile right vocal cords and clear subglottic area (Figure 7).
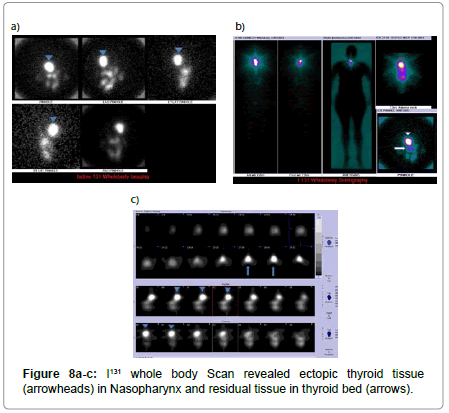
I131 whole body Scan was performed after 1 month and showed ectopic thyroid tissue in nasopharynx and residual tissue in thyroid bed (Figures 8).
Endocrinologist advised to do SPECT-CT Scan for better localization and Radio ablation of this residual thyroidal tissue but patient refused. At present, patient attends the voice clinic for voice therapy without any symptoms of airway obstruction and endocrinology clinic for follow up her thyroid function.
Discussion
First ectopic thyroid case was reported as a lingual thyroid by Hickman in the year of 1869 [24]. Ectopic thyroid is a developmental defect of thyroid gland that leads to presence of thyroid tissue at sites other than its normal cervical location. Presence of two ectopic foci of thyroid tissue is rare, only a very few cases of dual ectopia have been reported in the world literature and it is extremely rarer to have dual ectopic thyroid with a normally located pre-tracheal thyroid gland as our presented case [25-27]. Scintigraphy, using Technetium-99m, I-131, or I-123, is the most important diagnostic tool for ectopic thyroid but CT scan and MRI may help in defining the extension and location of the ectopic thyroid gland and fiberoptic laryngoscopy is recommended in order to visualize directly the intra-tracheal mass and biopsy is required for a histologic diagnosis [28-30]. Intra-tracheal ectopic thyroid tissue can cause progressive dyspnea, airway obstruction, stridor, cough, swallowing difficulty, and hemoptysis. The symptoms of ectopic intra-tracheal thyroid can easily be mistaken for those of asthma as in our case [31]. Treatment choices of ectopic thyroid tissue are: surgery, radioiodine ablation, and thyroid-suppression therapy [18]. Asymptomatic and euthyroid patients with ectopic thyroid tissue do not require any treatment, but when medical treatment fails in dysfunction thyroid patients or there are obstructive symptoms, haemorrhage or suspicion of malignancy, then surgery should be considered. Some surgeons consider excision in all cases [32]. The mainstay of treatment for ectopic intra-tracheal thyroid tissue is surgical excision and the endocrinologist advised the radioiodine ablation for the ectopic nasopharyngeal thyroid tissue in our present case. A variety of surgical techniques have been applied in the management of ectopic intra-tracheal thyroid tissue. Patients have two options: removal of the lesion via an open cricoid procedure, as we did in this case, or removal via an endoscopic laser-assisted approach [31,32].
In this case report, the intra-tracheal thyroid tissue was most probably dual ectopic foci with the other foci in the nasopharynx, but there is another weak probability that it was directly implanted into the tracheal lumen during the patient’s initial treatment for multi-nodular goitre in right lobe of the thyroid gland, while details of that surgical procedure were not available, implantation might occurred during surgery and the resultant remnant remained quiescent for 26 years before enlarging and ecoming symptomatic. There are rare reported cases of thyroid tissue implantation following blunt trauma, fine needle aspiration biopsy and endoscopic thyroid surgery, and there are only five documented cases of intra-tracheal thyroid tissue associated with previous thyroidectomy [33-36]. These patients presented 4 to 21 years after their original thyroid surgery, with dyspnea or stridor, the tissue was resected or iopsied in all cases, and found to contain benign thyroid tissue.
In this case a pre-op indirect laryngoscopy to assess vocal cord movement and airway patency was not enough to put a pre-op diagnosis and therefore a better surgical strategy and plan, also there was no any preoperative radiologic investigations such as ultrasound or CT Scan that would be helpful in planning surgery and would know the presence of thyroid remnants in the bed of the previous surgery so it may prevent severe subsequent morbidity.
Conclusions
Even ectopic intra-tracheal thyroid tissue is rare, it should be considered as a possible cause of airway obstruction, particularly in those who have goiters. The current case highlights the possibility of Intra-operative thyroid tissue implantation in the trachea and shows the need for careful tissue handling during thyroid surgery, so ectopic thyroid tissue should be considered in the differential diagnosis even in the presence of a normal thyroid gland.
Standard thyroid workup before any surgical intervention should include imaging such as thyroid ultrasound or CT Scan and an assessment of the vocal cords by fiberoptic nasolaryngoscopy or laryngostroboscopy to ensure the status following previous surgery and prior to any further surgical treatment.
Consent
Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images.
Authors’ Contributions
MSJ: conception and design, writer, revision and approval of the final version. JK, HT: conception and design, revision and approval of the final version. GY: conceived of the study, and participated in its design and coordination and helped to draft the manuscript. AA: revision and approval of the final version.
References
- Di Benedetto V (1997) Ectopicthyroid gland in the submandibular region simulating a thyroglossal duct cyst: a case report. J Pediatr Surg 32: 1745-1746.
- Babazade F, Mortazavi H, Jalalian H, Shahvali E (2009) Thyroid tissue as a submandibular mass: a case report. J Oral Sci 51: 655-657.
- Ulug T, Ulubil SA, Alagol F (2003) Dual ectopicthyroid: report of a case. J LaryngolOtol 117: 574-576.
- Kalan A, Tariq M (1999) Lingual thyroid gland: clinical evaluation and comprehensive management. Ear NoseThroat J 78: 340-34, 345-9.
- Yoon JS, Won KC, Cho IH, Lee JT, Lee HW (2007) Clinical characteristics of ectopicthyroid in Korea. Thyroid 17: 1117-1121.
- Salam MA1 (1992) Ectopicthyroid mass adherent to the oesophagus. J LaryngolOtol 106: 746-747.
- Gamblin TC, Jennings GR, Christie DB 3rd, Thompson WM Jr, Dalton ML (2003) Ectopicthyroid. Ann ThoracSurg 75: 1952-1953.
- Rieser GD, Ober KP, Cowan RJ, Cordell AR (1988) Radioiodide imaging of strumacordis. Clin Nucl Med 13: 421-422.
- Williams RJ, Lindop G, Butler J (2002) Ectopic thyroid tissue on the ascendingaorta: an operativefinding. Ann ThoracSurg 73: 1642-1643.
- Shiraishi T, Imai H, Fukutome K, Watanabe M, Yatani R (1999) Ectopic thyroid in the adrenal gland. Hum Pathol 30: 105-108.
- EyüboÄŸlu E, Kapan M, Ipek T, Ersan Y, Oz F (1999) Ectopic thyroid in the abdomen: report of a case. SurgToday 29: 472-474.
- Maino K, Skelton H, Yeager J, Smith KJ (2004) Benign ectopic thyroid tissue in a cutaneous location: a case report and review. J Cutan Pathol 31: 195-198.
- Takahashi T, Ishikura H, Kato H, Tanabe T, Yoshiki T (1991) Ectopic thyroid follicles in the submucosa of the duodenum. Virchows Arch A Pathol Anat Histopathol 418: 547-550.
- Ihtiyar E, Isiksoy S, Algin C, Sahin A, Erkasap S, et al. (2003) Ectopic thyroid in the gallbladder: report of a case. Surg Today 33: 777-780.
- Güngör B, Kebat T, Ozaslan C, Akilli S (2002) Intra-abdominal ectopicthyroidpresentingwithhyperthyroidism: report of a case. SurgToday 32: 148-150.
- Malone Q, Conn J, Gonzales M, Kaye A, Coleman P (1997) Ectopic pituitary fossa thyroid tissue. J Clin Neurosci 4: 360-363.
- Yilmaz F, Uzunlar AK, Sögütçü N (2005) Ectopic thyroid tissue in the uterus. Acta Obstet Gynecol Scand 84: 201-202.
- Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K (2011) Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol 165: 375-382.
- Harach HR, Cabrera JA, Williams ED (2004) Thyroid implants aftersurgery and blunt trauma. Ann DiagnPathol 8: 61-68.
- Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, et al. (2005) Needle tract implantation of papillary thyroid carcinoma after fine-needle aspiration biopsy. World J Surg 29: 1544-1549.
- Tamiolakis D, Antoniou C, Venizelos J, Lambropoulou M, Alexiadis G, et al. (2006) Papillary thyroid carcinoma metastasis mostprobably due to fine needle aspiration biopsy. A case report. Acta Dermatovenerol Alp PannonicaAdriat 15: 169-172.
- Lee YS, Yun JS, Jeong JJ, Nam KH, Chung WY, et al. (2008) Soft tissue implantation of thyroid adenomatous hyperplasia afterendoscopicthyroidsurgery. Thyroid 18: 483-484.
- Love RL, Ahsan F, Allison R, Keast A, Lambie N (2012) Multinodular goitre arising in the tracheal lumen: implantation or ectopic? J LaryngolOtol 126: 100-102.
- Hickman W (1869)Congenitaltumor of the base of the tongue, pressing down on the epiglottis and causingdeath by suffocation sixteenhoursafterbirth. TransPathol Soc Lond 20:160–161.
- Harisankar CNB (2013) Dual ectopicthyroid in the presence of atrophic orthotopic thyroid gland in a patient withacquiredhypothyroidism: Evaluation withhybrid Single-Photon Emission Computed Tomography/Computed Tomography. Indian J Nucl Med. 28: 26–27.
- Choudhury BK, Saikia UK, Sarma D, Saikia M, Choudhury SD, et al. (2011) Dual EctopicThyroid with Normally Located Thyroid: A Case Report. Journal of Thyroid Research.
- Sood A, Sood V, Sharma DR, Seam RK, Kumar R (2008) Thyroid scintigraphy in detecting dual ectopic thyroid: areview. Eur J Nucl Med Mol Imaging 35: 843-846.
- Bersaneti JA, Silva RD, Ramos RR, Matsushita Mde M, Souto LR (2011) Ectopic thyroid presenting as a submandibular mass. Head Neck Pathol 5: 63-66.
- Peters P, Stark P, Essig G Jr, Lorincz B, Bowman J, et al. (2010) Lingual thyroid: an unusual and surgically curable cause of sleepapnoea in a male. SleepBreath 14: 377-380.
- Yinlong Y, Quan L, JinMiao Q, Youqun X, Yifei P, et al. (2010) EctopicIntratrachealThyroid: case report. SouthernMedical Journal.
- Ramaniraj M, Jousal CP (2012) Dual ectopicthyroid – A case report of avery rare disease. JORL 2 Issue: 201.
- Soylu L, KiroÄŸlu F, Ersöz C, Ozcan C, Aydogan B (1993) Intralaryngotracheal thyroid. Am J Otolaryngol 14: 145-147.
- Byrd MC, Thompson LD, Wieneke JA (2003) Intratrachealectopic thyroid tissue: a case report and literaturereview. EarNoseThroat J 82: 514-518.
- Dowling EA, Johnson IM, Collier FC, Dillard RA (1962) Intratrachealgoiter: aclinico-pathologicreview. Ann Surg 156: 258-267.
- Osammor JY, Bulman CH, Blewitt RW (1990) Intralaryngotrachea lthyroid. J LaryngolOtol 104: 733-736.
Citation: Jabbr MS, Kassouma J, Salman HT, Youssef G (2015) Multi-nodular Goiter with Intra-tracheal Thyroid Tissue: Ectopic or Implanted? And Ectopic Nasopharyngeal Thyroid Tissue: A Case Report. Otolaryngology 5:204. DOI: 10.4172/2161-119X.1000204
Copyright: © 2015 Jabbr MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15682
- [From(publication date): 9-2015 - Jul 02, 2025]
- Breakdown by view type
- HTML page views: 11036
- PDF downloads: 4646