MRI Imaging of Focal Adenomyosis and Adenomyotic Cyst: Case Report
Received: 25-Jan-2018 / Accepted Date: 21-Feb-2018 / Published Date: 26-Feb-2018 DOI: 10.4172/2167-7964.1000292
Abstract
Adenomyosis is defined by the presence of ectopic endometrial glands and stroma within the myometrium. This happens when the normal boundary between the endometrial basal layer and the myometrium is disrupted. It proposed that it may be due to uterine trauma, pregnancy, postpartum endometritis, or caesarean delivery. Adenomyosis has been noted to occur in about 30% of the general female population and the reported prevalence of adenomyosis in hysterectomy specimens varies from 5% to 70%.
We report a case of a 42 year old female, nulligravida, with a medical history of complete spontaneous miscarriage five years ago; with uncontrolled bleeding which it need to be treated with cervical cerclage.
Actually she has a menstrual menometrorrhagia and dysmenorrhea treated with oral contraceptive pills but it did not stop. Transvaginal sonography showed a globular uterine enlargement with one leiomyoma and uterine wall thickening. Vascular malformation or adenomyosis were suspected. A MRI was performed which it showed findings in respect with adenomyosis.
Keywords: Adenomyosis; MRI; Endometrial glands; Sonography
Introduction
Adenomyosis is a common benign uterine disease characterized by the presence of ectopic endometrial glands and stroma within the myometrium. This happens when the normal boundary between the endometrial basal layer and the myometrium is disrupted. It proposed that it may be due to uterine trauma, pregnancy, postpartum endometritis, or caesarean delivery. Three forms of adenomyosis have been described: diffuse, focal and cystic. The patients usually refer vaginal bleeding, dyspareunia and chronic pelvic pain. Although the definitive diagnosis is by histopathological analysis, we have the cross sectional imaging techniques. By transvaginal ultrasound the diagnosis is often difficult to make, because it sometimes cannot be differentiated from leiomyomas. Magnetic resonance imaging (MRI) is also a noninvasive technique and may be more helpful than ultrasound in distinguishing adenomyosis from a leiomyoma. Actually hysterectomy is the definitive treatment for adenomyosis. We report MRI features of focal adenomyosis.
Case Report
In this case report, we present the case of a 42-year-old female, nulligravida, with a medical history of complete spontaneous miscarriage five years ago, with uncontrolled bleeding which it needed to be treated with cervical cerclage.
Actually she has a menstrual menometrorrhagia and dysmenorrhea treated with oral contraceptive pills but it did not stop. Transvaginal sonography showed a globular uterine enlargement with uterine wall thickening and one leiomyoma. Vascular malformation or adenomyosis were suspected. So a magnetic resonance imaging (MRI) was performed.
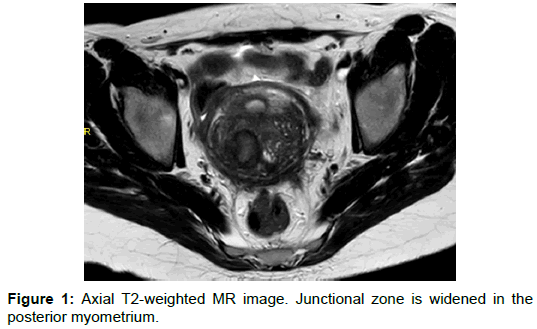
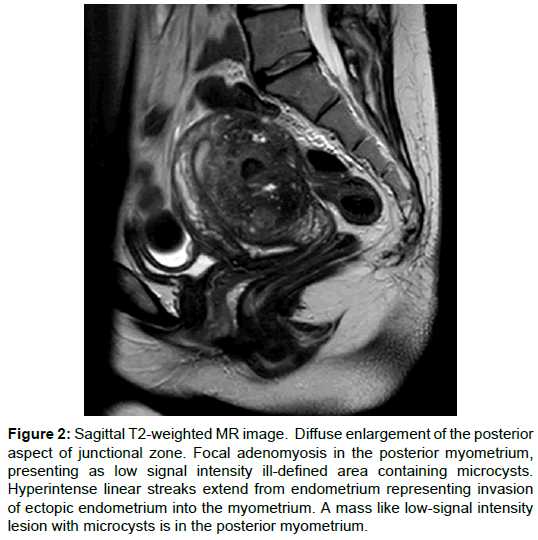
MRI showed a diffuse enlargement of the posterior aspect of junctional zone, with a mass like low signal intensity ill-defined area in the posterior myometrium containing micro cysts. Hyperintense linear streaks extend from endometrium into the myometrium (Figures 1 and 2).
Figure 2: Sagittal T2-weighted MR image. Diffuse enlargement of the posterior aspect of junctional zone. Focal adenomyosis in the posterior myometrium, presenting as low signal intensity ill-defined area containing microcysts. Hyperintense linear streaks extend from endometrium representing invasion of ectopic endometrium into the myometrium. A mass like low-signal intensity lesion with microcysts is in the posterior myometrium.
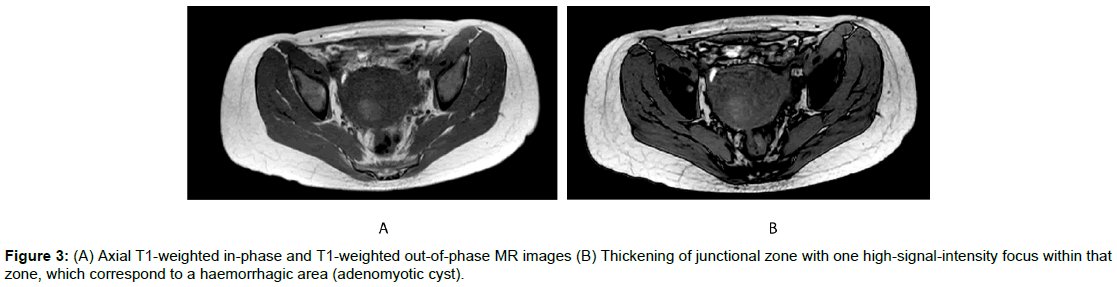
On axial T1-weighted in-phase and out-of-phase, it was identified one high-signal-intensity focus within that zone, which corresponds to a haemorrhagic area (Figures 3a and 3b).
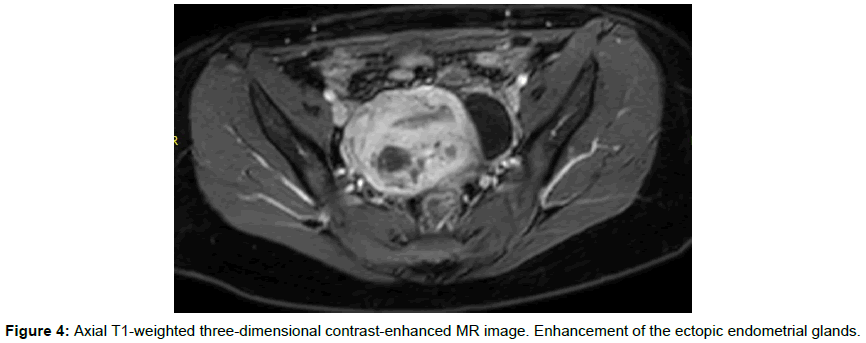
Axial T1-weighted three-dimensional contrast-enhanced showed an enhancement of the ectopic endometrial glands (Figure 4).
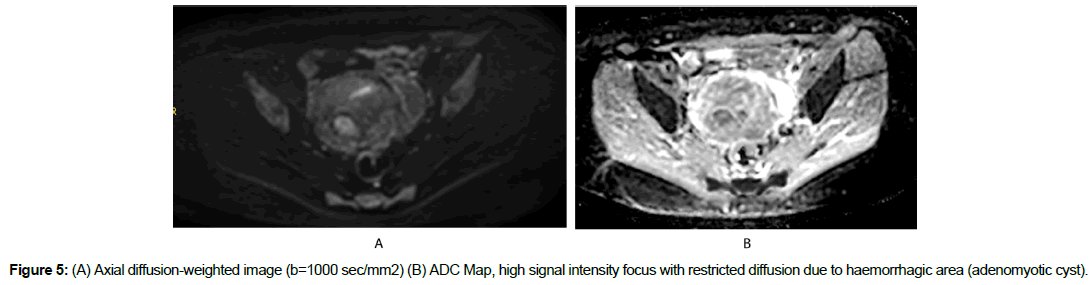
Axial diffusion-weighted image showed high-signal-intensity focus within the mass like with restricted diffusion which corresponds to haemorrhagic area described above (Figure 5).
It was not identified vascular malformation. These findings correspond to focal adenomyosis. The surgical team decided to perform hystectomy and submit it for histopathological examination. A definitive diagnosis of focal adenomyosis was made.
Discussion
Adenomyosis is a common benign uterine disease characterized by the presence of ectopic endometrial glands and stroma within the myometrium. This happens when the normal boundary between the endometrial basal layer and the myometrium is disrupted. It proposed that it may be due to uterine trauma, pregnancy, postpartum endometritis, or caesarean delivery. The preoperative prevalence rates of adenomyosis vary between 2.6% to 26% and in specimens of hystectomy vary widely from 5% to 70% [1].
With regard to etiology, it has been described that there is a disruption of normal boundary between the endometrial basal layer and the myometrium, may be due to several causes including uterine trauma, pregnancy, postpartum endometritis, or caesarean delivery [2]. The patients usually refer vaginal bleeding, dyspareunia and chronic pelvic pain. The cross-sectional imaging techniques have an important role in the preoperative diagnosis. Early assessment by transvaginal sonography has a sensibility and specify of 87% and 98% respectively according with the literature [3]. However sometimes the diagnosis by ultrasound it is difficult since adenomyosis usually coexist with leiomyomas and a myomatous uterus often makes difficult the assessment.
On MRI the interface between endometrium and myometrium (junctional zone) can be observed and it has been demonstrated by several authors. This junctional zone is identified like a low signal band on T2-weighted images separating endometrium from outer myometrium and limit values have been defined between 5 to 8 mm and when is greater than 12 mm it is a sign of adenomyosis [4]. Thus on MRI has been described direct and indirect signs to define the presence of ectopic endometrial glands within myometrium. The direct signs are micro cysts which are the main direct sign and this translates into ectopic endometrial glands with cystic changes. Another sign is adenomyoma which is a endometrial glands grouped in the myometrium and it is identified like a low signal intensity mass on T2-weighted images with cystic changes inside and without peripheral vessels which allows to distinguish to leiomyoma. The main indirect sign of adenomyosis is the enlargement of the junctional zone greater than 12 mm that if it involves whole zone is considered as diffuse form and if it involves a part of the zone is considered focal form. It has been described another signs like the junctional zone differential and the ratio of junctional zone thickness and myometrium thickness establishing when is greater than 40% a sensibility and specificity of 65% and 92% respectively [5].
There is rare form of adenomyosis and it is the adenomyotic cyst. This involves in the presence of a haemorrhagic cystic lesion subserosal, submucosal or like in our case within myometrium. These patients generally experience menorrhagia and dysmenorrhea [6]. On T1-weighted images this lesion is high signal intensity and on diffusion-weighted image the lesion shows restricted diffusion due to proteinaceous content of haemoglobin.
We need to consider that the differential diagnoses of adenomyosis are the leiomyoma, adenomatous tumor of the uterus and the metastasis to the uterine corpus.
Currently the definitive treatment of adenomyosis is the hysterectomy however it has been described the uterine artery embolization like alternative treatment but not always with satisfactory results [7].
Conclusion
Adenomyosis can become a debilitating disease in women. For the preoperative diagnosis we have the cross-sectional imaging techniques.
Sometimes with transvaginal sonography is difficult to make a diagnosis. MRI is a useful tool, does not irradiates and it allows a better visualization of complete uterine morphology and when we identified some specific signs we can make the diagnosis of adenomyosis.
References
- Atri M, Reinhold C, Mehio AR, Chapman WB, Bret PM (2000) Adenomyosis: US features with histologic correlation in an in vitro study. Radiology 215: 783-790.
- Hulka CA, Hall DA, McCarthy K, Simeone J (2002) Sonographic findings in patients with adenomyosis: Can sonography assist in predicting extent of disease? Am J Roentol 179: 379-383.
- Fedele L, Bianchi S, Dorta M, Zanotti F, Brioschi D, et al. (1992) Transvaginal ultrasonography in the differential diagnosis of adenomyoma versus leiomyoma. Am J Obs Gyn 167: 603-606.
- Hricak H, Alpers C, Crooks LE, Sheldon PE (1983) Magnetic resonance imaging of the female pelvis: Initial experience. Am J Roentgenol 141: 1119-1128.
- Novellas S, Chassang M, Delotte J, Toullalan O, Chevallier A, et al. (2011) MRI characteristics of the uterine junctional zone: From normal to the diagnosis of adenomyosis. Am J Roentgenol 196: 1206-1213.
- Tamai K, Togashi K, Ito T, Morisawa N, Fujiwara T, et al. (2005) MR imaging findings of adenomyosis: Correlation with histopathologic features and diagnostic pitfalls. Radiographics 25: 21-40.
- Kitamura Y, Allison SJ, Jha RC, Spies JB, Flick PA, et al. (2006) MRI of adenomyosis: Changes with uterine artery embolization. Am J Roentgenol 186: 855-864.
Citation: Guarín JMP, Río JV, Benítez GM, Cordón FD (2018) MRI Imaging of Focal Adenomyosis and Adenomyotic Cyst: Case Report. OMICS J Radiol 7: 292. DOI: 10.4172/2167-7964.1000292
Copyright: ©2018 Guarín JMP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 6958
- [From(publication date): 0-2018 - Apr 16, 2025]
- Breakdown by view type
- HTML page views: 6071
- PDF downloads: 887