Moya Moya Disease in a 5 Year Child-presenting as Hemiparesis withMedullary Sponge Kidneys
Received: 16-May-2017 / Accepted Date: 29-May-2017 / Published Date: 07-Jun-2017 DOI: 10.4172/2572-4983.1000S1014
Abstract
Moya moya disease is a very rare cause of acute stroke in pediatrics age group. The disease was first described by Takeuchi and Shmuziin 1957.since the disease is common in japan and cases have been reported mostly in japan but cases have been reported rarely from non-Japanese regions including India. Moya moya disease is a progressive steno occlusive disease at terminal portion of internal carotid arteried with development of collateral channels of circulation.
We report a case of 5 years male child who presented with history of fall 1 day back followed by sudden loss of speech and weakness of right side of the body. Patient was diagnosed moya moya disease on basis of MRI angiography.
Keywords: Moya moya; Internal carotid artery stenosis; Hemiparesis
Introduction
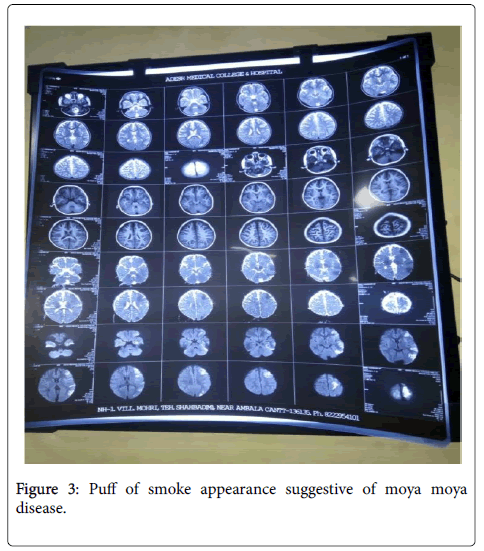
Moyamoya disease is a chronic, progressive occlusive disease of circle is arteries that lead to the development of collateral vessels inside the brain parenchyma. The vessels develop a characteristic pattern on imaging seen on cerebral angiography, giving a puff of smoke appearance. Puff of smoke in Japanese terminology means moyamoya after which the disease is named. The disease is a very under recognized cause of stroke and rarely reported in pediatrics age group. The disease has varying presentations like seizures, aphasia, dysarthria, hemiparesis, chronic headache, renal stenosis. It has been reported with other medical conditions like autoimmune disease, downs syndrome, head trauma, meningitis, neurofibromatosis etc.
Case Report
A five year old child brought by parents in emergency with complaints of difficulty in using right side of upper limb and weakness of right side of lower limb. The child is not able to speak since morning. History of fall from bed one day back suddenly while the child was playing on bed. Parents complaint of distinction of abdomen since last six months. On examination child had heart rate of 102 per minute, respiratory rate of 30 per minute, temperature afebrile, blood pressure of 100/70 mm hg, pulses all palpable, good volume. Child was conscious GCS 15/15, chest and cardiovascular examination normal. As Per abdomen distended, liver 2 cm brs, kidneys palpable B/L, spleen not palpable. CNS examination, gcs 15/15, pupils b/l equal reacting, right side upper limb and lower limb power 2/5. Tone increased, DTR +, plantar sup going. Child was investigated. Complete counts showed tlc 9600, p 65%, l 35%, e 4%, serum Na 145, s. calcium 8.2 mg%, RBS 94 mg%. USG abdomen showed bilateral medullary sponge kidneys size 10.1 cm left, and 10.2 cm right side. MRI showed acute infarction in left middle cerebral artery (MCA), left anterior cerebral artery and left posterior cerebral artery and left middle cerebral arteries watershed territories.
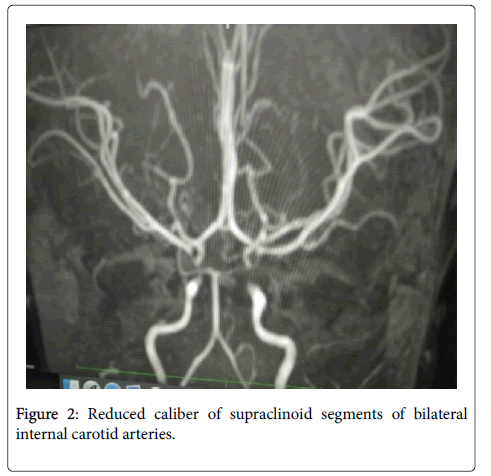
Chronic infarct in right ACA-MCA watershed territory and subacute infarcts in right MCA-PCA watershed territory… Bilateral ischemic changes noticed in b/l deep white matter (Figure 1). MR angiography showed reduced caliber of supraclinoid segments of bilateral Internal carotid arteries (left>right) (Figure 2) and circle of Willis collaterals giving puff of smoke appearance (Figure 3) suggestive of moyamoya disease. Child was referred for neurosurgical management and re-vascularization surgery.
Discussion
Moyamoya disease was first described in Japan by Takeuchi and Shimizu in 1963. Moyamoya disease is a chronic, progressive occlusion of the circle of Willis arteries that leads to the development of characteristic collateral vessels seen on imaging, particularly cerebral angiography. The appearance of these small, multiple vessels at the base of the brain angiography was originally described by the Japanese term moyamoya, which translates “ puff of smoke.” Moyamoya disease occurs predominantly in Japanese individuals but has been found in all races [1] with varying age distributions and clinical manifestations. As a result, moyamoya disease has been under recognized as a cause of ischemic and hemorrhagic strokes in children, the most common presents with recurrent episodes of cerebral ischemia manifesting as seizures, focal deficits, paresthesia [2]. The process of narrowing of cerebral vessels seems to be a reaction of brain blood vessels to a wide variety of external stimuli, injuries, or genetic defects. Conditions such as sickle cell anemia, neurofibromatosis-1, Down’s syndrome, congenital heart defects, antiphospholipid syndrome, renal artery stenosis, and thyroiditis have been found to be with moyamoya disease [3]. The process of blockage, once it begins, tends to continue despite any known medical management unless treated with surgery. Typical symptoms are monoparesis, hemi paresis, aphasia, and dysarthria. Headache, seizures, and involuntary movements, such as hemichorea, can be serious symptoms associated with pediatric moyamoya disease. Some children give history of fall may be due to hyperpnea or excitement, such as playing, blowing on hot noodles, playing a trumpet or crying, may trigger TIA due to hyperventilation-induced reduction of cerebral blood flow. When a precise diagnosis is delayed, slowly progressive mental impairment has also been observed. MRI not only reveals are as of infarctions, but also allows direct visualization of these collateral vessels as multiple small flow voids at the base of brain and basal ganglia. MR angiography is used to confirm the diagnosis and to see the anatomy of the vessels involved. It typically reveals the narrowing and occlusion of proximal cerebral vessels and extensive collateral flow through the perforating vessels demonstrating the classic puff of smoke appearance [4].
Acute management is mainly symptomatic and directed towards reducing elevated intracranial pressure, improving cerebral blood flow, and controlling seizures. There are no effective medical therapies for moyamoya disease. Surgical revascularization [5] is thought to improve cerebral perfusion, and to reduce the risk of subsequent stroke in both pediatric and adult patients. In pediatric patient, the incidence of TIA rapidly decreases after surgery.
References
- Natori Y, Kjezaki K, Matsushima T, Fukui M (1997) “Angiography moya moya its definition, classification and therapy. Clin Neurol Neurosurg. 99: S168-S172.
- Vernet O, Montes JL, O'Gorman AM, Baruchel S, Farmer JP (1996) “Encephaloduroarterio-synangiosis in a child with sickle cell anemia and moyamoya disease,†Pediatric Neurology 14: 226-230.
- Lutterman, Scott M, Naes R, Geva T (1998) “Moya moya syndrome associated with congenital heart disease.†Paediatrics 101: 57-60.
- Lippincott, Williams, Wilkins (2002) MR Angiography: Techniques and Clinical Applications MRI of the Brain and Spine. SW Atlas. Philadelphia. USA.
- Khan N, Schuknecht B, Boltshauser E (2003) Moya moya disease and moya moya syndrome: experience in Europe; choice of revascularisation procedures. Acta Neurochirurgica 145: 1061-1071.
Citation: Gandhi R, Jitender, Anand V (2017) Moya Moya Disease in a 5 Year Child-presenting as Hemiparesis with Medullary Sponge Kidneys. Neonat Pediatr Med 3: S1014. DOI: 10.4172/2572-4983.1000S1014
Copyright: © 2017 Gandhi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4061
- [From(publication date): 0-2015 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 3245
- PDF downloads: 816