Research Article Open Access
Model for Assessing Disruptive Behavior in the Medical Setting: Pilot Study of Provider Satisfaction
Jennifer Piel*
Department of Psychiatry and Behavior Sciences, University of Washington, Seattle, Washington, USA
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
Background: Risk assessment of future disruptive and violent acts is of great importance to public protection and care in the medical setting. The VA Puget Sound, Seattle, is utilizing clinical forensic risk evaluations in its assessments of veterans with disruptive Patient Record Flags or at elevated risk for violent behavior. Aim: To assess and compare provider knowledge, experience, and satisfaction with the clinical forensic risk assessment through the facility's Disruptive Behavior Evaluation Clinic. Method: A pilot internet-based survey was constructed to evaluate provider characteristics, experience, and satisfaction with a new Disruptive Behavior Evaluation Clinic. Members of the hospital's Disruptive Behavior Committee and mental health service lines were asked about their familiarity and confidence in the consultative service. Results: Forty-four providers responded. Of these, 23 providers were familiar with the Disruptive Behavior Evaluation Clinic and its clinical forensic risk assessments. All members of the facility's Disruptive Behavior Committee were familiar with the risk assessments. Members of the Disruptive Behavior Committee as well as clinical providers from the mental health service lines ranked highly the utility of the detailed risk assessments and risk management recommendations. Conclusions: The provider satisfaction survey provided evidence for the overall satisfaction with the use of clinical forensic risk assessments in VA facilities for assessment and management of persons with Patient Record Flags and other indicators of elevated risk of disruptive or violent behavior at one VA hospital.
Keywords
Disruptive behavior, violence, hospital, risk assessment
Introduction
In the wake of highly publicized shootings at VA medical centers and other hospitals, concerns about patient-directed violence and disruptive behavior (such as harassment, stalking, and verbal aggression) are a focus of media and local attention. Although hospital shootings are rare, violence at medical centers is a common concern. More than 10% of hospital employees report at least one work-place assault per year. Patients are the most common assaulters (Hodgson et al., 2004).
It is policy of the Veteran’s Health Administration (VHA) that all of its hospitals create Disruptive Behavior Committees (DBC) to identify and assess patients who pose elevated risk for violence at their facilities (38 C.F.R section 17.106). Also required at VHA facilities are the use of Patient Record Flags. Patient Record Flags (PRFs) are patient behavioral alerts that are incorporated into the secure reporting system in patient electronic medical records. The PRFs are used to alert VHA employees to patients whose behavior or characteristics may pose an immediate threat to the safety of the patient or others.
At most VHA facilities, the DBC is tasked with identifying and reviewing patients that have evidenced disruptive behaviors. Typically, the DBC assesses risk and makes recommendations regarding the appropriateness of behavioral PRFs by reviewing the veterans' medical charts.
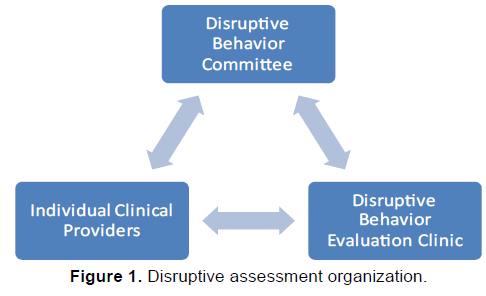
The VA Puget Sound, Seattle, has created a novel Disruptive Behavior Evaluation Clinic for complex referrals from the DBC and other providers. The VA Puget Sound established the Disruptive Behavior Evaluation Clinic to improve violence risk assessments for persons at elevated risk of disruptive behavior at the facility. There are two primary routes of referral to the Disruptive Behavior Evaluation Clinic: (1) direct consultation from the DBC and (2) requests from clinicians seeking detailed risk assessments for their patients who pose elevated risk of violence. Clinicians from any service, not just Mental Health or Addictions, may request a consult from the clinic. Although the primary referral source to the Disruptive Behavior Evaluation Clinic is through the hospital’s DBC, the DBC and Disruptive Behavior Evaluation Clinic are distinct and comprised of different staff members.
The Disruptive Behavior Evaluation Clinic is staffed by a psychiatrist with fellowship training and experience in the field of forensic psychiatry. Although psychiatrists and other clinicians are often called upon to assess the risk of violence posed by their patients, many patient histories and presentations are complex, and there are occasions that warrant a more detailed assessment of a person’s violence risk than can be provided in a routine appointment visit or by review of specific incidents. Psychiatrists and psychologists with specialty training in forensics have skills in performing detailed violence risk assessments, using screening tools related to violence assessment, and in creating risk management plans.
The Disruptive Behavior Evaluation Clinic evaluator performs detailed clinical forensic violence risk evaluations to aid the DBC in its determinations and provide risk reduction recommendations. Some medical facilities hire forensic-trained mental health providers to perform forensic violence risk assessments on a case-by-case basis or when, due to liability concerns, a second opinion about a person’s risk for violence is warranted. The VA Puget Sound is unique in establishing a novel clinic dedicated to these detailed violence risk assessments.
The evaluations performed by the Disruptive Behavior Evaluation Clinic include a psychiatric interview with the referred veteran. The interview is typically several hours in duration, includes the mental status examination, and makes use of relevant assessment tools. The Historical, Clinical, and Risk Management Scales (HCR-20) (Webster, Douglas, Eaves, & Hart, 1997), a violence assessment tool, is performed for all veterans referred to the clinic. Additional screening tools, such as the Partner Violence Screen (PVS) for interpersonal violence, are used when relevant. Occasionally, personality or intellectual testing is obtained to assist with the evaluation. The evaluator obtains collateral information from the evaluee’s treating providers, and also obtains records from hospitalizations at outside facilities and legal records. The evaluator also contacts persons outside the hospitalsetting familiar with the veteran for additional collateral information. Participation by the veterans is voluntary and informed consent is obtained.
The Disruptive Behavior Evaluation Clinic evaluator prepares a clinical forensic risk assessment report that is entered in the veteran’s medical chart. The report summarizes the clinical interview, prior treatment records, collateral records, and documents the results of any screening tools. The reports include a detailed opinion about the evaluee’s risk for violence and basis for the opinion; an opinion as to the appropriateness and level of a PRF; and recommendations to reduce risk. The forensic evaluator communicates his/her risk assessment and risk modification recommendations to the DBC and clinical providers, when applicable (Figure 1).
The primary objective of this pilot feasibility study was to assess satisfaction with the newly established Disruptive Behavior Evaluation Clinic. Secondary objectives were to gather preliminary information on how the Disruptive Behavior Evaluation Clinic was being used and whether differences exist depending on the type of provider reviewing the assessments (members of DBC versus other clinical providers). What follows are results from a provider satisfaction survey after the first year of the utilizing the Disruptive Behavior Evaluation Clinic and its forensic risk assessments.
Method
The pilot feasibility study was an internet-based satisfaction survey of providers in the mental health service lines at VA Puget Sound, Seattle division. Included among eligible respondents were members of the hospital’s DBC. Surveys were distributed to 86 staff providers identified by listserve in mental health services lines within the VA Puget Sound. The VA Puget Sound has two divisions, Seattle and American Lake. Because the Disruptive Behavior Evaluation Clinic had not been introduced to the American Lake division, any response from an American Lake provider was excluded.
The internet-based survey was constructed to evaluate provider characteristics, experience, and satisfaction with the Disruptive Behavior Evaluation Clinic after its first year of practice. The survey consisted of 15 questions, which included four questions on respondent characteristics; one question on awareness of the clinic; nine questions regarding the utility of the assessment service and provider satisfaction with the clinic and assessments; and one free-form question for individual respondent feedback. The survey questions are included here in Addendum A. Descriptive labels were used to report the provider responses based on Likert scales. The responses were anonymous and confidential.
Eligible providers were sent a brief email introduction to the study, request for participation, and a link to the internet-based survey. Eligible providers were notified that they had two weeks to complete the survey. After one week, a reminder message went out to all eligible respondents.
Results
A total of 58 providers met the pilot study’s initial inclusion criteria from the VA Puget Sound, Seattle Division. Forty-four providers responded from the VA Puget Sound VA, Seattle division (76%).
Survey Findings
Respondents by primary discipline were as follows: 28% physician, 23% social work, 22% nursing, 16% psychologist, 3% research, and 8% other. In addition to holding clinical positions, 8 respondents were also members of the hospital’s DBC. Respondents self-identified their primary clinical site within the hospital as follows: 27% Mental Health Clinic; 18% Addictions Treatment Center; 11 % Primary Care Mental Health; 9% Inpatient Psychiatry; 5% Emergency Department; 5% Intensive Outpatient Mental Health Program; 5% Personal Recovery/Chronic Mentally Ill; 5% PTSD Outpatient Clinic; 2% Community Housing and Outreach; 2% Suicide Prevention; 2% Women’s Trauma and Recovery; and 9% Other.
If respondents indicated that they had no familiarity with the clinic, then the assessment was not considered for further analysis regarding the utility of the clinic or respondent satisfaction. In all, 23 providers had direct knowledge and familiarity with the Disruptive Behavior Evaluation Clinic and its risk assessments. As the primary referral source for the clinical forensic risk evaluations is the hospital’s DBC, responses from DBC members were separately analyzed from the pool of general mental health providers.
Familiarity
Twenty-three survey respondents had direct knowledge and familiarity with the Disruptive Behavior Evaluation Clinic and its risk assessments and their responses were analyzed for satisfaction and utility of the clinic. Included among respondents, all members (n=8) of the hospital’s DBC were familiar with the clinic and clinical forensic risk assessments. Table 1 identifies how various providers had made use of the service. The DBC members are distinguished from the remainder of the providers (n=15) in Table 1. All DBC respondents had previously been involved in requesting consultation from the Disruptive Behavior Evaluation Clinic, had reviewed a final clinical forensic risk assessmentreport produced by the Disruptive Behavior Evaluation Clinic, had utilized the service in making recommendations whether to continue or modify a PRF in a veteran’s medical chart, and utilized an assessment for clinical management. In contrast, the cohort of other mental health providers familiar with the service had more variable experience with the clinic. The majority of these providers became familiar with the clinic after having reviewed a risk assessment report.
| Resource Utilized | Percent of Respondents (n=8) | Percent of all Mental Health Providers (n=15) |
|---|---|---|
| Requested Clinical Violence Risk Assessment | 100 | 35 |
| Reviewed Risk Assessment Report | 100 | 80 |
| Determining Behavioral Flag | 100 | 24 |
| Support of Involuntary Hospitalization | 0 | 5 |
| Clinical Management of Veteran | 100 | 60 |
| Making Housing Decisions | 33 | 10 |
| Making Decisions about Duties to Warn Third Parties | 66 | 20 |
Table 1: Assessment Utilization by the DBC and Mental Health Providers Familiar with Clinic (VA Puget Sound—Seattle).
Assessment Utility
Table 2 summarizes provider responses regarding the utility (or anticipated utility) of the assessments. Members of the DBC and general mental health providers both ranked Detailed Risk Assessment and Risk Management Recommendations as highest utility. Where a number rank is shown more than once, it indicates a tie in number of responses for these categories.
| Resource | DBC Respondents (n=8) | Mental Health Providers (n=15) |
|---|---|---|
| Detailed Risk Assessment | 1 | 1 |
| Diagnostic Impression | 2 | 3 |
| Risk Management Recommendations | 1 | 1 |
| Second Opinion for Clinical Judgment | 1 | 2 |
| Duties to Third Parties | 3 | 6 |
| Behavioral Flag | 1 | 4 |
| Comprehensive Mental Health Assessment in One Document | 2 | 5 |
Table 2: Utility Rating of Risk Assessment by DBC and Mental Health Providers Familiar with Clinic (VA Puget Sound – Seattle).
Satisfaction
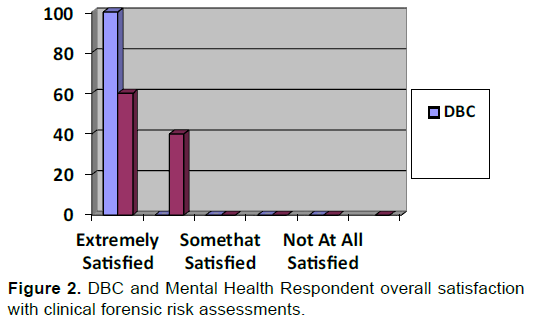
Figure 2 summarizes respondent satisfaction with the risk assessment service by class of provider. All DBC member respondents recorded that they were “extremely” satisfied with the risk assessments. Mental health providers, generally, rated their interaction with the Disruptive Behavior Assessment Clinic as positive with 60% of respondents “extremely” satisfied and 40% “pretty” satisfied. No respondent selected an alternative lower category. Additionally, one hundred percent of respondents familiar with the assessment service (n=23) indicated that they would recommend the service to a colleague.
Providers were asked, in their perception, how helpful the risk assessments had been for individual clinical decision-making and how helpful the assessments had been, generally, for the VA Puget Sound Health Care Center (hospital), rated “not at all, “mildly,” “somewhat,” “very,” or “extremely”. Figure 3 shows the respondents’ perceptions of usefulness for the hospital in general. Both the DBC respondents and other mental health provider respondents had the same percentage breakdown for individual decision-making. Of DBC respondents, 100% of respondents rated that the assessments as “extremely” useful to the hospital; 66% rated assessments as “extremely” useful and 33% “very” useful for individual decisionmaking, respectively. For other mental health providers, generally, 66% rated the assessments as “extremely” useful and 33% rated them as “very” useful for individual decision-making, but for the hospital they responded 55% “extremely,” 36% “very” and 9% “somewhat” useful.
Recommendations
Survey respondents were asked to identify recommendations to improve the usefulness of the Disruptive Behavior Evaluation Clinic. The most common responses among all surveyed were to create a clinical consult request for the service through the facility's electronic record management system and to expand the clinic to provide assessments for veterans at other local-area VHA facilities. Table 3 lists recommendations for improvement. Where a number rank is shown more than once, it indicates a tie in number of responses for these categories.
| Recommendation | Rank |
|---|---|
| Consult request through electronic record management system | 1 |
| Expand to local campus (VA Puget Sound, American Lake division) | 2 |
| Provider education about appropriate referrals | 3 |
| Clearly identify the risk assessment reports within the electronic medical record | 4 |
| Link violence assessment reports to appropriate PRFs | 4 |
| Provider education about utility of clinical forensic risk assessments | 5 |
| More availability | 6 |
Table 3: Recommendations to improve the Disruptive Behavior Evaluation Clinic.
Discussion
Although this is a pilot study of a new clinic, survey results show general provider satisfaction with the Disruptive Behavior Evaluation Clinic and its clinical forensic risk assessments in assessing veterans with disruptive PRFs and disruptive behaviors at one VHA facility, the VA Puget Sound, Seattle division. Prior to the development of the Disruptive Behavior Evaluation Clinic, veterans with disruptive PRFs were assessed and monitored by the hospital’s DBC primarily through chart review. The VA Puget Sound, Seattle, is unique in maintaining a Disruptive Behavior Evaluation Clinic to assist with this process. It also serves as a consulting clinic to clinical providers requesting further violence risk assessment for patients. As far as this writer is aware, this initial provider survey study is the first to look at clinical provider satisfaction with dedicated forensic violence risk assessment resources for evaluating veterans with disruptive PRFs or evidence of other disruptive or violent behavior at VHA facilities.
Providers at the VA Puget Sound have come into contact with the Disruptive Behavior Evaluation Clinic and its forensic risk assessments by varying routes. Although any provider can request a consult from the Disruptive Behavior Evaluation Clinic, the initial focus has been to assist the DBC in evaluating veterans with PRFs and evidence of violence at the health care facility, against providers, or other veteran patrons. It is not surprising, then, that 100% of the DBC respondents had familiarity with the clinic. All DBC respondents had been involved in consulting the Disruptive Behavior Evaluation Clinic and reviewing its clinical forensic risk assessment reports.
In contrast, other mental health providers have had more varied contact with the clinic. Consistent with the consultation aspect of the clinic, some mental health providers will have directly consulted the clinic for a detailed risk assessment. Other providers may have become aware of the clinic and assessments after, for example, a colleague requested an evaluation for one of their mutual patients. Or, perhaps one of their patients had a disruptive PRF. Emergency Department and consultation providers may, similarly, identify a risk assessment report in the patient’s chart when assessing the veteran for an urgent issue. The manner in which the assessment reports are utilized are likewise varied and likely reflect the specific clinical relationship that any given provider has with a veteran. For example, as illustrated in Table 1, mental health providers may utilize the assessment for care needs, such as to support an involuntary commitment petition, which is less likely to be relevant to members of the DBC. Table 2 reflects anticipated use of the clinic and its assessments, and reflects how the service could be used by different referring providers.
Although the sample size is small, the responses indicate overall provider satisfaction with the clinic to date. Members of the DBC are most familiar with the Disruptive Behavior Evaluation Clinic and universally rate their experience as “extremely” satisfied. The DBC’s role of responding to disruptive behavior on a systems (hospital) basis is reflected in their uniform response that the service is “extremely” useful to the hospital. Other general mental health providers, who likely view the assessments through their capacity as an individual provider, are likely to focus more on utility of the assessment for individual practice than on a systems basis.
Of note, in the electronic medical record for the VA Puget Sound, Seattle, is a note template that can be used by all providers called the Violence Risk Comprehensive Assessment Note. This is a one-page template useful in routine clinical practice to document violence risk factors. The chart note for the Disruptive Behavior Evaluation clinic is entitled the Disruptive Behavior Evaluation Clinic Consult Risk Assessment Report; the assessments average 10 pages of report-style documentation. As this study did not explicitly distinguish the Disruptive Behavior Evaluation Clinic Consult Risk Assessment Reports from this other note template, certain mental health providers (with less familiarity with the clinic) may have responded to the survey with the general note template in mind.
In addition to the small sample size, this project was limited by the sampling procedure (survey instrument). Although all eligible providers received the study and questions allowed for persons with no familiarity with the service, participation in the survey was nonetheless voluntary; respondents may have differed from nonrespondents. Moreover, the results cannot be generalized to any hospital-based violence risk assessment consultation service.
Finally, this study does not assess the effectiveness of Disruptive Behavior Evaluation Clinic or the clinical violence risk assessments. Although I anticipate that use of the forensic assessment (which utilizes interview, scales, and collateral information) is more effective than chart review alone in evaluating risk for future violence, such measures are the subject for another study and have not been evaluated here.
Conclusion
The survey results provide evidence of provider satisfaction with the Disruptive Behavior Evaluation Clinic and its risk assessment after its first year of service. As the clinic evaluates more veterans and more providers have interactions with the clinic, additional information on provider satisfaction should be obtained. As eluded to above, further research on the effectiveness of the service warrants additional attention.
References
- Hodgson, M.J., et al. (2004). Violence in Healthcare Facilities: Lessons from CHA. Journal of Occupational and Environmental Medicine, 46, 1158-1165.
- 38 C.F.R section 17.106 – VA response to disruptive behavior of patients.
- Webster, C.D., Douglas, K.S., Eaves, D., &Hart, S.D. (1997). HCR–20: Assessing Risk for Violence (Version 2). Simon Fraser University.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14062
- [From(publication date):
June-2015 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9443
- PDF downloads : 4619