Mode of Action of Shatavari Tail Matra Basti and Nasya in Asrigdara: A Critical Review
Received: 12-Feb-2022 / Manuscript No. jham-22-54297 / Editor assigned: 14-Feb-2022 / PreQC No. jham-22-54297 / Reviewed: 28-Feb-2022 / QC No. jham-22-54297 / Revised: 04-Mar-2022 / Manuscript No. jham-22-54297 (R) / Accepted Date: 08-Mar-2022 / Published Date: 10-Mar-2022 DOI: 10.4172/2573-4555.1000311
Abstract
Asrigdara is a gynecological condition defined as excessive bleeding during menstruation. Charka has described this condition due to vitiation of vata and pitta dosha along with rakta dosha. According to the modern science Abnormal Uterine Bleeding (Dysfunctional uterine bleeding) is irregular uterine bleeding that occurs in the absence of recognizable pelvic pathology, general medical disease or pregnancy. AUB is reported to occur in 9 to 14% women between menarche and menopause. The prevalence varies in each country. In India, the reported prevalence of Abnormal Uterine Bleeding is around 17.9%.
Abnormal Uterine Bleeding or Asrigdara is of more concern, because excessive or prolonged bleeding may cause undue disruption of women’s daily activities and affect woman’s health both physically and psychologically. The incidence rate of Asrigdara is increasing day by day so if treatment is delayed this can lead to a worsening of condition of patient due to excessive blood loss. Various treatments modalities like hormonal therapy, antiprostaglandins, antifibrinolytic agents and surgical interventions are available in modern medicine for the management of heavy menstrual bleeding. Taking in to account the side effect and adverse effects there is a great scope of research to find out safe, potent, cost effective remedy from ayurveda by addressing the root of the problem there by improving the quality of life of woman. Many formulations have been mentioned in our texts for the treatment of Asrigdara. Achaya Sharangadhar has described Shatavari Tail in the treatment of Asrigdara. Shatavari Tail is Vata-Pitta Shamak due to its properties like sheet virya, Madhura Vipaka and Guru Snigdha guna. It has anti-secretory, anti-ulcerogenic properties. It also works as astringent hence it can reduce menstrual flow by these properties.
Keywords: Asrigdara; Abnormal uterine bleeding; Shatavari tail; Nasya; Matra
Keywords
Asrigdara; Abnormal uterine bleeding; Shatavari tail; Nasya; Matra
Introduction
Artava denotes two meaning one of them is Antah pushpa i.e., ovum and other one is Bahir pushpa. Bahir pushpa i.e., Menstruation. Menstruation is a visible illustration of cyclic, physiological uterine bleeding. The menstrual rhythm is invisible interplay of hypothalamopituitary- ovarian axis. Whereas the amount of blood depends upon the uterine condition. The relationship between endometrium and it’s regulating factors is responsible for regular cyclic menstruation, change in either of these result in abnormal bleeding. Due to alteration of food habits and changing life styles complain of the excessive and irregular uterine bleeding is increasing day by day. It reflects a disruption in the normal cyclic pattern of ovulatory hormonal stimulation to the endometrial lining. Abnormal Uterine Bleeding is a common problem among women in the reproductive age. AUB may be accompanied by pain and discomfort cause significant social embarrassment and have a substantial effect on health- related quality of life. AUB lead to loss of productivity and may result in surgical interventions including hysterectomy. Management of such common condition in a population with wide healthcare diversity requires uniform clinical practice guideline [1].
The disease Asrigdara explained in Ayurveda may be co-related with condition heavy menstrual bleeding. According to Acharya Charak if the menstrual cycle turns to be abnormal due to pradirana of Raja, it is termed as pradara. According to Acharya Sushruta, excessive and prolonged bleeding during menstruation or even in intermenstrual period, different from the features of normal menstrual blood is called asrigdara. Asrigdara is described as separate disease in Yonivyapada Chikitsa and also described as shonitjanya vikara, in the symptoms of Pittavrata Apanvayu, Complication of Yonirogas and as Raktayoni. If the condition is not treated properly, it can cause further complications like Balahani, Dhatuksheenata, Daurbalaya, Pandu, Bhrama, Angamardya affecting her quality of life. Acharya Kashyap in Shatpushpashatavari kalpa adhyaya also indicates use of Shatavari in Atyartava. Most of the drugs in Shatavari Tail are Vata-Pitta Shamak due to Madhura, Tikta Ras, Sheet virya, Madhur Vipaka. They are Raktastambhak, Pittashamak and Dahaprashaman. So Shatavari Tail due to its astringent property it reduces the menstrual flow and it is also effective antiulcerogenic and anti- secretory agent has its role in healing of endometrium.
Etiological factors for Asrigdara
Acharya Charaka have described following causes of Asrigdara in Chikitsa Sthan
1. The woman who consume excessive sour, salty, heavy, katu, vidahi (producing burning sensation).
2. Curd.
3. Meat of domestic, aquatic, fatty animals.
4. Payasa.
5. Suktall (Vinegar).
6. Mastu (Curd water).
7. Adhyashan (Taking meals before digestion of meal already taken)
8. Virudhashan (Incompatible diet)
9. Abortion.
10. Excessive coitus.
11. Riding.
12. Weight-Lifting.
13. Trauma.
14. Day Sleeping.
Samprapti of Asrigdara
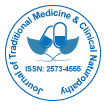
Acharya Charak explained asrigdara as a disease of vitiated Rakta and pittavrita apan vayu. In Charak Chikitsa Sthan, it is mentioned that due to hetusevana tridosha mainly Pitta, Vata and Rakta gets vitiated Rakta increases in amount and simultaneously raja gets increased in amount. Aggravated vayu with vitiated Rakta reaches raja carrying vessels (menstrual blood) of uterus [2]. Thus excessive raja comes out as heavy menses is known as asrigdara. Vyan vayu is responsible for alteration in the ratio of prostaglandins and disturbance in Hypothalamo-Pitutary axis. Disturbance in endometrial blood vessels and capillaries may occur due to vitiation of pitta dosha which is responsible for heavy menstrual bleeding (Figure 1).
Dosha - Vata(apan), Pitta (Pradhan)
Dushya - Rakta (Pradhan) and Artava, Rasa Agni- Jathragnimandya.
Adhishthana - Garbhashaya, Artavavahi srotas. Strotasa - Raktavahi, Artavavahi, Rasavahi.
Sroto-Dusti Prakara- Atipravritti. ROGA Marga - Aabhyantara.
Mode of action of drugs of Shatavari Tail
As research work is going on shatavari tail. The main content of the drug is shatavari so probable mode of action is Shatavari (Asparagus racemosus) is a source of phytoestrogens. These are weaker than natural estrogen in action. However, they compete with estrogen receptor. In the presence of an excess of estrogen in the body, phytoestrogen may have antiestrogenic effect by occupying the same estrogen receptor. In condition of low serum estrogen, phytoestrogen occupy the same estrogen receptor. In condition of low serum estrogen, Phyto estrogenic occupy vacant receptors and stimulate estrogenic action. Hence menorrhagia is due to an excess of estrogen or reduced estrogen (atrophy of endometrium) it can help in either case [3].
The roots are considered as an astringent hence they reduce menstrual flow by this property. Moreover, Asparagus was found to be effective antiulcerogenic and anti-secretory agent and thus has its role in healing of endometrium. It is also an adaptogen. It has significant antidepressants activity and this effect is probably medicated through the serotonergic and noradrenergic system and augmentation of antioxidant defenses. This help to reduce the stress level in the body thus normalizing the imbalance of hormones.
Tail with its Sneha and sukshma guna, may easily absorbed through mucous membrane, gland and vessels and by its steroidal action gives nutrition and potentiates the endometrial receptors (Tables 1-3).
| Plant name | Botanica l name | Family | Varga |
|---|---|---|---|
| Shatavari | Asparagus racemosus | Liliaceae | Balya, Vayasthapana |
| Bala | Sida cordifolia |
Malvaceae | Brahniya, Vatasansamana |
| Atibala | Abutilon indicum | Malvaceae | Balya, brahniya, Vatasamsamana |
| Shalaparni | Desmodium gangeticum | Leguminosae | Angamardprashamana,shothahar |
| prasnaparni | Uraria picta | Leguminosae | Shothahar, Sandhaniya |
| Arand | Ricinus communis | Euphorbiacea e | Vatasansamana, Angamardaprashamana |
| Ashwagandha | Withania somnifera | Solanaceae | Balya, Brahniya |
| Gokshura | Tribulus terrestris | Zygophyllacea e | Shothahar |
| Bael | Aegle marmelos |
Rutaceae | Shothahar |
| Kasha | Saccharum spontaneum | Gramineae | Vata-pitta Shamak, Rakta-pitta Shamak, Dahaprashamanam |
| Kurantak | Barleria prionitis | Acanthaceae | Vedanasthapana, Samdhaniya, Raktasodhak |
| Til | Sesamum indicum |
Pedaliaceae | Vedanasthapana,sandhaniya,vranrop an, vranshodhan |
| Devdaru | Cedrus deodaru | Pinaceae | Vatasamshaman, Vednasthapana |
| Jatamansi | Nordostachy s jatamansi |
Valerianaceae | Vedanasthapana, Dahaprashamana |
| Tagar | Valeriana wallichii | Valerianaceae | Tiktaskandha |
| Chandan | Santalum album |
Santalaceae | Dahaprashamanam, Raktapitta shamak, angmardprashamnum |
| Satpushpa | Foenieulum vulgare | Umbelliferae | Vatta-Pitta Shamak |
| Kushtha | Saussurea lappa | Compositae | Vedanasthapana, Raktasodhak |
| Ala | Elettaria cardamomu m | Zingiberaceae | Angmardprashamanam, Vatta-Pitta Shamak |
| Meda | Listea glutinosa | Lauraceae | |
| Madhuk | Glycyrrhiza glabra |
Leguminocae | Shonotsthapana, Vedanasthapana, Shonithara |
| Vidari | Purraria tuberosa | Leguminosae | Balya, Brahniya, Vedanasthapana, Shonithara |
| Varahi | Dioscorea bulbifera | Dioscoreaceae | Raktavikara |
Table 1: Shows description of Shatavari tail.
| Plant | Guna | Rasa | Vipaka | Virya |
|---|---|---|---|---|
| Shatavari | Guru, Snigdha | Madhur, Tikta | Madhura | Sheeta |
| Shalparni | Guru, Snigdha | Madhur, Tikta | Madhura | Ushna |
| Prasnparni | Laghu,Snigdha | Madhur,Tikta | Madhura | Ushna |
| Arand | Snigdha, Tikshna,Sukshm | Madhur Anurasa-Katu,Kashaya |
Madhura | Ushna |
| Ashwagandha | Laghu, Snigdha | Tikta, Katu, Madhua | Madhura | Ushna |
| Gokhura | Guru, Snigdha | Madhura | Madhura | Sheeta |
| Bael | Laghu,Ruksha | Kashaya,Tikta | Katu | Ushna |
| Kasha | Laghu,Snigdha | Madhura, kashaya | Madhura | Sheeta |
| Jatamansi | Laghu, Snigdha | Tikta,Kashaya,Madhura | Katu | Sheeta |
| Chandan | Laghu,Rukha | Tikta, Madhura | Katu | Sheeta |
| Mishreya | Laghu, Snigdha | Madhura,Katu,Tikta | Madhura | Sheeta |
| Ala | Laghu,Ruksha | Katu, Madhura | Madhura | Sheeta |
| Shaileya | Laghu, Snigdha | Tikta, Kashaya | Katu | Sheeta |
| Kumud | Laghu,Snigdha,Pichhila | Kashaya, Madhura, Tikta | Madhura | Sheeta |
| Madhuka | Guru, Snigdha | Katu, Tikta, Kashaya | Madhura | Sheeta |
| Vidari | Guru, Snigdha | Madhura | Madhura | Sheeta |
Table 2: Showing pharmacological activities of shatavari tail contents.
| 1 | Ras | Madhura, Tikta, Kashaya |
|---|---|---|
| 2 | Guna | Laghu, Ruksa |
| 3 | Virya | Sheeta |
| 4 | Vipaka | Madhura |
| 5 | Karma | Mainly pitta Shamak also vata shamak |
Table 3: Showing predominant rasa panchaka of shatavari tails.
By Rasa Panchaka
Rasa: Shatavari Tail has Madhura, Tikta and Kashaya Rasa.
• Madhura rasa result in Rakta prasadana and relieves complication of asrigdara i.e. Trishna, Daha and Murchha. Madhura rasa is also having Vata-Pitta prashamana, Balya, Prahaladana, jeevanaya, tarpana, Shandhankara guna leading to improvement of physiological as well as psychological strength of body and organs (Uterus).
• Kashaya Rasa result in kleda Shoshana, Raktapitta prashamana and Lekhana.Samgrahi and stambhaka action of Kashaya Rasa help in Raktasamgrahana and Raktastambhana. Prithvi mahabhuta present in Kashaya rasa is responsible for samghata i.e. compactness in the endometrium thereby reduces the fragility of the endometrium.
• Here Tikta Rasa have Agni Deepana and Pachana properties which help to cure Agnimandhya condition. Tikta rasa is having pitta-shaleshma upshoshan guna helping to reduce extra congestion in uterus.
Guna: Shatavari has raktashodhan, shravashoshan, sangrahi and vata-pitta shamak properties.
Veerya: Shatavari Tail has sheet virya. Sheeta virya result in Pittashamana, Stambhana and Rakta Pitta Prasadhana. Sheeta virya does Pittashamana, Raktasangrahana, Raktastambhana and Dahaprasamana that corrects burning sensation and excessive blood loss.
Ipaka: Shatavari Tail has madhura vipaka. It does Vata-Pitta Shamana and formulation of proper Rasa dhatu takes place.
Doshaghnata: Shatavari tail having Vata-Pitta shaman property.
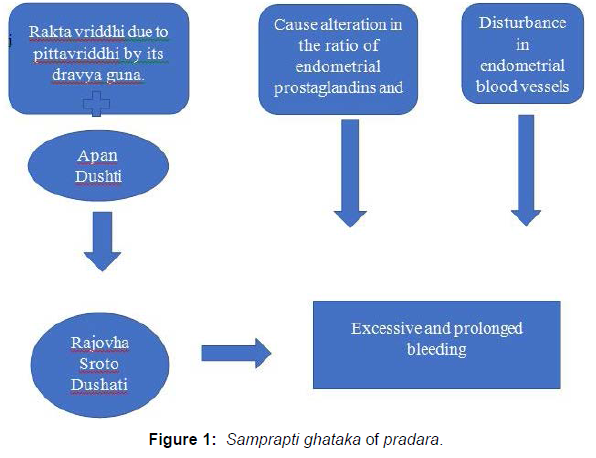
Samprapti Bhang of Asrugdar
In the pathogenesis of asrigdar Chala guna of Vata dosha, Sara and dravya guna of pitta dosha increase in amount of blood. Properties of shatavari tail like madhura, Kashaya and tikta rasa help in pitta shamana and srotoshodhan and sheeta virya help in raktastambhana and pittashamana and madhura vipaka help in Vata- Pitta shaman (Figure 2).
Mode of action of basti
Basti is said in Ayurveda as half of the whole treatment schedules.
It is said to control almost all the disease, all the Dosha and it is very acute on its onset of action, though it is typically scheduled to eliminate and pacify vayu. The main abode of vayu is said in ayurvedic classics as Pakvashaya and Basti pacifies this vayu by its potency lodging in the pakvashaya. With the advancement of modern science, a new nervous system of abdomen has been discovered which is named as Enteric Nervous system and simpily it is called as mini brain. The Enteric nervous system (ENS) , an independent part of the nervous system, comprising of a number of neural circuits set in networks of enteric ganglia connected by inter ganglionic strands controls local blood flow, mucosal transport and secretion , motor functions and modulates immune and endocrine functions in synchronized manner and functionally it is interlinked with each other [4].
The gastrointestinal tract communicates with the CNS in two ways. Afferent neurons convey signal of consciousness, including pain, discomfort, feeling of hunger and satiety, and other states of the gastrointestinal tract. Other afferent signals for the nutrient load in the small intestine, or the acidity of the stomach, do not normally reach higher brain. CNS provides signals to control the intestine, which are, in most cases relayed through the ENS. Communication between the enteric nervous system and the immune system of the gastrointestinal tract is maintained through ENS terminals released transmitters on the mucosa influencing immune related cells like mast cells and vice versa , like by that very mucosa released active substances, including cytokines and mast cell tryptase, on enteric neurons [5].
In Ayurveda, pakvashaya has been mentioned as the special abode of vayu and said to be treated first for vataja disease by Basti. The special abode in Ayurveda is considered only for the shodhana purpose as the shodhana therapies eliminates the respective Dosha from these abodes, e.g. Vamana eliminates Kapha from its specific abodes (Amashaya), Virechana from Pittashaya. In connection to Shodhana, Basti can control the total vayu located all over the body by controlling the vayu phenomenon in Pakvashaya. By the discovery of ENS, this fact may be established in modern perspective. From the description of ENS, it is clear that ENS may control all the CNS function. The controlling center is definitely the head which is regulated by prana, but for treatment purpose, the Basti may take control over the entire system by means of regulating the ENS in either manner.
Overall functions of the enteric System
1. Control of Motility.
2. Regulation of fluid exchange and local blood flow.
3. Regulation of gastric and pancreatic secretion.
4. Regulation of gastrointestinal endocrine cells.
5. Defense reactions.
6. Entero-enteric reflexes.
7. ENS-CNS interactions.
The Basti is containing several drugs and inserted in warm condition in fairly good amount. These factors are quite enough to influence the primary afferent neurons and here by ENS. Basti fluid by its direct action over nerve endings can control the whole body by influencing hormonal secretions and CNS. Moreover, abhyanga and svedana prior to Basti therapy may have some role in influencing the ENS. The drugs may also be transported to the circulation by local veins and lymphatics and thus mitigates the disease elsewhere in the body [6].
Absorption of Basti
Rectal administration provides rapid absorption of many drugs and may be an easy alternative to the intravenous route, having the advantage of being relatively painless. The rate of rectal transmucosal absorption is affected by the following factors like formulation, volume of liquid, Concentration of drug, pH of rectal contents etc. Drugs administered high in the rectum (drained by the superior rectal vein) as usually carried directly to the liver and thus are subject to metabolism. Drugs administered low in the rectum are delivered systemically by the inferior and middle rectal vein before passing through the liver. The formulation of Basti is a major factor for absorption and distribution of the drugs. The Anuvasana Basti retains inside for a long time. Volume mostly controls the retention of Basti inside the lumen. Sneha and Anuvasana basti are to be given in a lesser amount as because it is intended to stay inside at least up to three ‘yama’ i. e 9 hours. Presence of stool in the rectal vault inhibits the recipe to enter or come out smoothly. Rectal pH may also influence drug uptake by altering the amount of drug that is ionized. The greater lipid solubility of nonionized drugs enhances their movement across biological membranes [7].
Absorption of Sneha
Oil, ghee and vasa are used in both the Niruha and Anuvasana but as the Basti material does not go beyond ileo-cecal junction in normal condition, it can be thought that how these fatty substances are absorbed and comes in account. For absorption and digestion of Sneha generally bile, gastric lipase, pancreatic lipase etc. are necessary. Chakrapani has also arouse the same doubt but also has solved the same by stating that the fat adhered to the colon is acted upon by the Agni located above the colon while its exudates to the exterior. If the Agni does not come into the direct contact with Sneha even then, parts of Jatharagni which gets mixed up with Sneha may digest that. This is specially inkling about presence of some factors of digestion there which is not yet discovered. The Sneha used in Basti is mainly composed of triglycerides, fatty acids, phospholipids etc. The type and character of fatty acids depends on the length of carbon chain in it. Short chain and Medium chain fatty acids are presents in ghee, milk and other natural oils which are used in Basti.
These two fatty acids are absorbed through the wall of the colon as they do not require bile salt or pancreatic lipase or micelle formation for absorption. SCFA is rapidly absorbed and stimulates colonic NaCl and fluid absorption. It lowers the colonic pH which protect the colonic mucosal layer from formation of polyps, inhibits inflammation and adhesion of irritant and increase the mineral absorption. It also influences the immune function of body by production of T helper cell, leukocytes, cytokines and modulates lymph mechanism. Moreover, it controls blood sugar and cholesterol level.
Mode of action of Nasya
Nasya karma simply means nasal administration of drugs or a means of delivering drugs preferentially to the brain to avail an overall effect on the body. While some substrates appear to be delivered directly to the brain via this route, the mechanism governing overall uptake and exposure remain unclear. Some substrates use olfactory nerve tract and gain direct access to the brain thus bypassing the blood-brain- barrier. However, most of the drugs gain access to the brain via the olfactory epithelium, which represents a more direct route of uptake. Some drugs use traditional blood and lymphatic route to get access to the circulation [8].
Effect of Purva Karma of Nasya on neurovascular Junction
The pre-operative measures adopted in nasya therapy like lowering of the head, elevation of the lower extremities and fomentation of the face have some role on enhancement of blood circulation in head. Efferent vasodilator nerves are spread out on the superficial surface of face. These receptors may receive stimulation from above said actions and results in an increase in blood circulation in head i.e. momentary hyperemia. By means of these facial stimulations, the cerebral capillaries dilated up to 22% which ultimately results in 150% blood inflow [9].
Mode of action of nasya karma in ayurveda
According to charak, ‘Nasa is the gateway of Shira’. The drug administered through nose as nasya reaches the brain and then either it eliminates the morbid. Dosha responsible for producing the disease or nourishes the area. Appropriate drug for particular disease may also pacify the disease by reaching the site. It may be used as a potential drug route for treating systemic diseases also. In Ashtanga Samgraha, it is explained that Nasa is the door way to Shira (head), and it communicates with eyes, ears, throat etc. by minute channels. The drug administered through nostrils, reaches Shringataka Marma (a shira marma) and spread into the Murdha (Brain), Netra(eyes), Shrota (Ears), Kantha (throat), Siramukhas (opening of the vessels) etc. and snatches the morbid doshas from these regions and expels them from Uttamanga.
Effect of nasya in neuro-endocrinal and neuro-psychological level
The limbic system is concerned with multifunctional capabilities including behavioral aspect of human beings and control over endocrine secretions. The olfactory nerves and other adjacent nerves named as terminal nerves which run along the olfactory nerves are connected with limbic system of brain including hypothalamus. The experimental stimulation of olfactory nerve caused stimulation of certain cell of hypothalamus and amygdaloidal complex. The most probable way of action of drug should be through olfactory pathways influencing hypothalamus, which in turn causes the inhibition effect through the pituitary.
Absorption of drugs using traditional routes
The drugs when administered nasally will normally be cleared rapidly from the nasal cavity into the gastro intestinal tract by the mucocilliary clearance system. A quality of drug will be absorbed across the nasal mucosa and reach the systemic circulation from where it will be eliminated via normal clearance mechanism. It is although dependent on the lipophilicity and molecular weight of the drug. Some of the drugs which are capable to cross the blood brain barrier also follow the systemic pathway to reach the brain. The drug used in nasya is transported by nasal venous blood to the facial vein. There is no valve in between the facial and ophthalmic veins so that blood may flow in either side. It can be said that blood from the facial vein can enter cavernous venous sinus of the brain in reverse direction. More over the head lowered position during nasya enhances this phenomenon. Infective thrombosis of facial vein may lead to meningitis using this path. Drug transportation by lymphatic path, can reach direct in to the C.S.F. The probable way for this is through cribriform plate. The arachnoid matter sleeve is extended to the sub-mucosal area of the nose along with olfactory nerve. It is experiment that, dye injected into arachnoid matter colors the nasal mucosa within seconds and vise-versa. It is found that steroids enter into the C.S.F. more rapidly followed by nasal spray as compared with systemic injection.
The inhaled drugs used in nasya are primarily deposited in the tissue of the upper air way. Accessto the distal airways is a function of particle size. In human large particles (>4micrometer) and small particles (0.5 to 0.1 micrometer) tend to deposit in the nasopharyngeal structure whereas intermediate particle (1 to 4) reaches distal airway. Water soluble drugs tend to remain on the tissues of upper airways and fat-soluble drugs are more likely to reach distal airways. The instilled drugs over olfactory mucosa are rapidly absorbed by three routes (1) by olfactory neurons. (2) by supporting cells and the surrounding capillary bed and (3) into the cerebrospinal fluid (CSF). Transneuroneal absorption is generally slow, whereas absorption by supporting cell and the capillary bed is rapid (Figure 3).
Discussion
Pradara, Artavadushti, artavavraddhi can be grouped under Abnormal Uterine Bleeding. The abovesaid condition are indicative of an abnormal or deranged underlying pathology. The underlying pathology can be summarized as increase in the level of pitta dosha, Rasa and Rakta dhatu vaigunyam affecting the sira/dhamanis of uterus, Apan vayu vaigunyam (Pitta vaisamyam or avarana dosha) and samprapti vighatana should be done by use of shatavari tail which has Madhura, Kashaya rasa, sheeta virya and Madhura vipaka help in shravashosan, srotoshodhan, vata-pitta shaman and raktastambhan. AUB occur in paittiki artava dusti as dosha lakshan in pradara, parripluta, raktaja rajodushti, Raktarbuda, Yoni arsas, Adhoga raktapitta, Asrja as vyadhi lakshana as upadrava in pittaja jwara and as an arista lakshan in Raktagulma.
Vitiation of Pitta Dosha and Rakta Dosha with apan vayu vaigunya can lead to the pathogenetic changes leading to Asrigdara. Function of Agni is also impaired. Asrigdar due to impairment of Agni, Rasa dhatu didn’t formed properly and improper Rasa Dhatu formation leads to improper Rakta Dhatu formation [10].
Effect on doshas
Vata dosha
Vyan vayu is responsible for alteration in the ratio of endometrial prostaglandin and disturbance in hypothalamopitutary ovarian axis to counteract above pathology. Katu rasa helps to normalize vayu and normalize the ratio of endometrial prostaglandins.
Pitta dosha
Disturbance in endometrial blood vessels and capillaries may occurs due to vitiation of pitta dosha, Rajovaha srotas and it normalize the disturbance in endometrial blood vessels and capillaries.
In the pathogenesis of the asrigdar Chala guna of Vata dosha and Sara and Dravya guna of pitta dosha increase the amount of blood. Hence Shatavari Tail might affect the sara and dravya guna of pitta dosha with the help of the madhura and Kashaya rasa so this could be the reason in reducing the amount of bleeding. Vata-Pitta shamak, Raktasthambhan, sandhaniya and srotoshodhan properties help in proper management of asrigdara.
Conclusion
Excessive and/or prolonged bleeding during menstrual or intermentrual period is known as Asrigdara. It can be co-related with the Abnormal Uterine Bleeding. Various treatments modalities like hormonal therapy, antiprostaglandins, antifibrinolytic agents and surgical interventions are available in modern medicine for the management of Abnormal Uterine Bleeding. Taking into account the side effects and adverse effects, Use of shatavari tail can be recommended as a safer and effective therapy for the management of asrigdara due to its properties like raktashodhan, shravashoshan, sangrahi and Vata-pitta shamak properties.
References
- Vijay L (2017) Ayurvedic approach of menorrhagia: Asrigdara. Int J Ayurveda Pharma Res 5: 1.
- Khushboo , Bharathi K, Jha K, Anu MS (2021) Compilation of management of asrigdara from various ayurvedic classic text books. Int J Ayurveda Integr Med 2:43.
- Raturi S, Kapil S, Shukla S (2020) A comparative study to evaluate the efficacy of herbomineral compounds in asrigdara w.s.r to dysfunctional uterine bleeding. J Res Educ Indian Med 1:1
- Jadhav AN, Bhutani KK (2005) Ayurveda and gynecological disorders. J Ethnopharmacol 97: 151-159.
- Chuneka KC, Pandey GS (1998) The Bhavprakash nighantu with elaborated hindi commentary 216:128-130.
- Himangi VB, Rajani M, Purani D, Purani R, Raut K (2017) Probable mode of action of darvyadi kwath on asrigdara - A review. Pharma Sci Monit 8: 200-207.
- http://www.healthywomen.orgexternal./.
- http://www.hemophilia.caexternal/.
- Vasantbhai BH, Meera R, Dipti P, Krupali R (2017) Probable mode of action of darvyadi kwath on asrigdara - A review. Int J Pharm Sci 8: 200-207.
- Sharma S, Pandey M (2020)Concept of asrigdara with its principles of management - A review article. World J Pharm Res 9: 458 - 474.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Gautam S, Singh S (2022) Mode of Action of Shatavari Tail Matra Basti and Nasya in Asrigdara: A Critical Review. J Tradit Med Clin Natur, 11: 311. DOI: 10.4172/2573-4555.1000311
Copyright: © 2022 Gautam S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2876
- [From(publication date): 0-2022 - Feb 22, 2025]
- Breakdown by view type
- HTML page views: 2473
- PDF downloads: 403