Mitral Valve Replacement in Infant-Should We Avoid?
Received: 19-Feb-2022 / Manuscript No. JCPR-22-54376 / Editor assigned: 21-Feb-2022 / PreQC No. JCPR-22-54376 (PQ) / Reviewed: 07-Mar-2022 / QC No. JCPR-22-54376 / Revised: 12-Mar-2022 / Manuscript No. JCPR-22-54376 (R) / Published Date: 19-Mar-2022 DOI: 10.4172/jcpr.1000160
Abstract
Mitral valve replacement is difficult due to small annulus size, non-availability of small valve, growth of the child, poor early and long term result and reoperation, side effect of anticoagulant. Mitral annulus can be enlarged and there are so many small size valve available like melody valve, cylindrical valve and ROSS procedure. Redo MVR is more common due to annular growth with functional stenosis.
Keywords
Mitral valve; Ventricle; Surgical Techniques
Introduction
Mitral valve replacement in infant is very challenging not only because of technical point of view but also poor short and long term outcome. It is done in case of dysplastic mitral valve and failed mitral valve repair. Technical difficulty is due to small annulus size, nonavailability of small prosthetic valve [1]. There are so many important structures around mitral annulus like left circumflex artery, coronary sinus, no coronary and left coronary sinus of aortic valve and bundle of his so annular enlargement like aortic annulus is difficult. Due to thin vascular system chances of anticoagulant induced bleeding is more. Reintervention is needed due to somatic growth [2].
Surgical Techniques and Challenges
Mitral valve replacement is needed in cardiomyopathy with severe mitral regurgitation and preserved ejection fraction, failed mitral valve repair, replacement of a mitral prosthesis, hemolysis following mitral valve repair, severe atrioventricular valve regurgitation in single ventricle.
Following standard sternototomy and Aorto-bicaval cannulation mitral valve can be approached trans septal or trans left atrium. Mitral valve should be inspected. In case of dysplastic or atrophic leaflet, small chordate, direct attachment between leaflet and papillary muscle primary mitral valve replacement is preferred. Though re-repair should be attempted some center prefers mitral valve replacement after single repair. Prosthesis can be placed in annular or supra-annular position. In case of supra-annular replacement valve may be tilted anteriorly or posteriorly for appropriate positioning. As annulus is small whole mitral valve leaflet, chordate and papillary muscle is excised to prevent postoperative gradient. Large prosthesis should be avoided to prevent complete heart block due to injury in bundle of his. Para valvular leak is prevented with pledgeted suture but there is more chance of pannus formation [3].
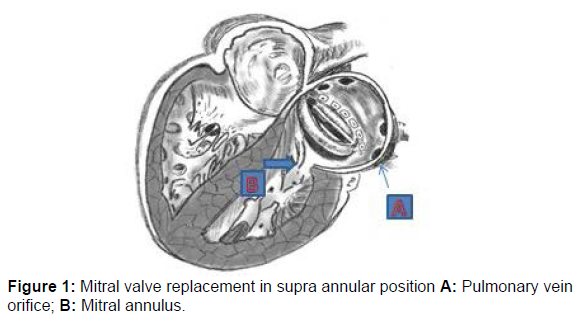
In case of supra-annular replacement valve is placed in ss between mitral annulus and inferior right and left pulmonary vein. Care should be taken to prevent pulmonary vein orifice obstruction and anteriorly suture is taken in atrial septum. Pledgeted everting horizontal suture is used. Position of the valve should be above coronary sinus level to prevent injury to bundle of his [4].
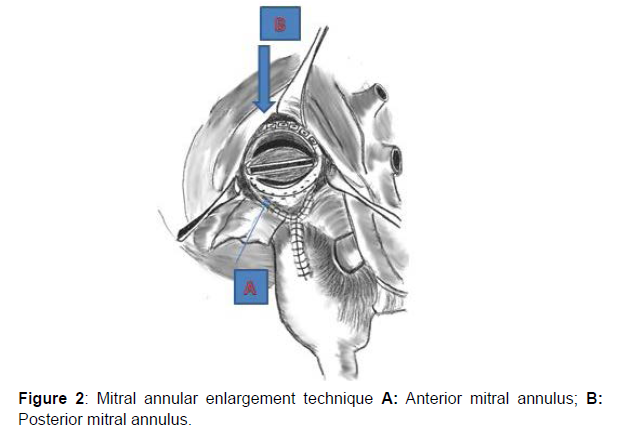
For enlargement of the annulus incision is given in aorta and incision is extended between non and right coronary cusp. Triangular pericardial patch is sutured to the valve and apex of the pericardium is sutured to commissure between none and right coronary cusp to prevent aortic regurgitation [5].
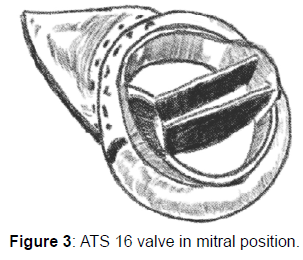
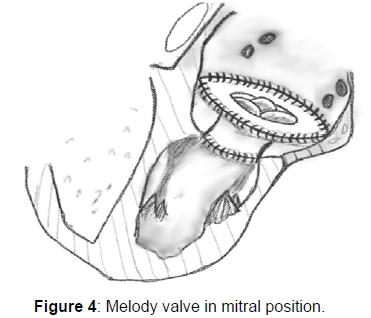
Melody valve is commonly used in pulmonary position but it can be used in mitral position in infant because of its small size. And after growing of the child it can be extracted percutaneously. In infant proximal and distal crown of the valve should be trimmed and pericardial strip is attached to stent which is fixed to the vein wall. Balloon catheter is inserted into compressed valve and size of the balloon is determined according to annulus size determined on preoperative echocardiography. Valve is fixed to posterior ventricular wall to prevent left ventricular outflow tract obstruction [6].
As per case report by Bellaing et al pulmonary autograft was used in mitral position. Pulmonary end of the autograft was sutured to the mitral annulus and infundibular end of the autograft was sutured to left atrial wall after reinforcement with pericardium [7].
Cylindrical valve is made of 2 layer extracellular matrix. After echocardiographic assessment of the mitral annulus valve is made with size approximately 4 mm larger than annular size to reduce purse string effect and annulus is strengthened with second layer and other end is sutured with the papillary muscle with CV 5 PTFE suture [8].
Outcome
Poor outcome after mitral valve replacement is due to small annulus, bleeding due to anticoagulation. As per study by Mater K et al out of the 12 patients in the cohort in hospital mortality was 0%.In mean follow up duration(6.2+-4.4 years) survival rates was 100% and 27.3 % patient underwent redo MVR and 18.2% patients underwent surgical intervention due to left ventricular outflow obstruction and 13.6% patients needed permanent pacemaker placement [2]. Redo MVR is more common due to somatic growth followed by functional stenosis and left ventricular outflow tract obstruction and complete heart block is due to large prosthesis. In the study by Geoffrion TR et al. in hospital mortality was 66.66% (2 out of the 3 patients) and one survived patient underwent redo MVR after 6 years [9]. Eltayeb OM et al. described no operative mortality in their cohort of 7 patients. Permanent pacemaker implantation was done in 2 (28.57%) patients and 57.14% of the patients underwent redo MVR [3]. In the series of 2 patients by Pollock JC et al in hospital and late mortality were 0%, 50% consecutively [10]. In supra annular position of the mitral valve left atrial volume and compliance is decreased and ventricularised left atrial volume increased and this condition is associated with low cardiac output and pulmonary venous hypertension [11].
Conclusion
Infant MVR can be done with accepted in hospital mortality and there are so many new small size valves are available. Though long term outcome is not good due to more incidence of redo MVR due to somatic growth of the child.
References
- Beierlein W, Becker V, Yates R, Tsang V, Elliott M, et al. (2007) Long-term follow-up after mitral valve replacement in childhood: poor event-free survival in the young child. Eur J Cardiothorac Surg 31:860-865.
- Ibezim C, Sarvestani AL, Knight JH, Qayum O, Alshami N, et al. (2019) Outcomes of mechanical mitral valve replacement in children. Ann Thorac Surg 107: 143-150.
- Eltayeb OM, Readdy WJ, Mongé MC, Forbess JM, Sarwark AE, et al. (2019) Mitral Valve Replacement in Infants Using a 15-mm Mechanical Valve. Ann Thorac Surg 108: 552-557.
- Mater K, Ayer J, Nicholson I, Winlaw D, Chard R, et al. (2019) Patient-Specific Approach to Mitral Valve Replacement in Infants Weighing 10 kilograms or less. World J Pediatr Congenit Heart Surg 10: 304-312.
- Jonas RA, Keane JF, Lock JE (1998) Aortic valve-preserving procedure for enlargement of the left ventricular outflow tract and mitral anulus. J Thorac Cardiovasc Surg 115: 1219-1222.
- Freud LR, Marx GR, Marshall AC, Tworetzky W, Emani SM (2017) Assessment of the Melody valve in the mitral position in young children by echocardiography. J Thorac Cardiovasc Surg 153: 153-160.
- Bellaing AMd, Mathiron A, Lecompte Y, Vouhe P (2019) Mitral valve replacement with a pulmonary autograft: long-term follow-up in an infant. Interact Cardiovasc Thorac Surg 28: 828-829.
- Kiper C, Cua CL, Baker P 3rd, McConnell P (2020) Mitral Valve Replacement in Pediatrics Using an Extracellular Matrix Cylinder Valve: A Case Series. Pediatr Cardiol 41: 1458-1465.
- Geoffrion TR, Pirolli TJ, Pruszynski J, Dyer AK, Davies RR (2020). Mitral Valve Surgery in the First Year of Life. Pediatr Cardiol 41: 334-340.
- Pollock JC, Shawkat S, Houston A (1984) Mitral valve replacement in the first three months of life. Br Heart J. 52: 549-51.
- Barker CL, Daubeney PEF, Shinebourne EA (2005) Complications of supra-annular mitral valve placement in infants. Heart 91: e48.
Indexed at , Google Scholar, Crossref
Indexed at , Google Scholar, Crossref
Indexed at , Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Kumar R, Rawat S, Halder V, Ghosh S, Dutta ARS, et al. (2022) A study on Morphology of Rupture of Sinus of Valsalva, Clinical Presentation, Surgical Techniques and Postoperative outcome-A single Centre Experience. J Card Pulm Rehabi 6: 160. DOI: 10.4172/jcpr.1000160
Copyright: © 2022 Kumar R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2317
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1823
- PDF downloads: 494