Research Article Open Access
Minimally Invasive Treatment Protocol for Closed Pilon Fractures
Sherif Mohamed Abdelgaid1*, Mohamed Abdulghany Ahmed2 and Emad Gaber Abdel-Mageed31Orthopedic Consultant, AL-Razi Orthopedic Hospital, Kuwait
2Senior Registrar, AL-Razi Orthopedic Hospital, Kuwait
3Registrar, AL-Razi Orthopedic Hospital, Kuwait
- *Corresponding Author:
- Sherif Mohamed Abdelgaid
Consultant (Orthop) AL-Razi orthopedic hospital, Kuwait
Tel: 0096599539270
E-mail: Sherifmaa@yahoo.com
Received Date: January 18, 2013; Accepted Date: May 18, 2013; Published Date: May 24, 2013
Citation: Abdelgaid SM, Ahmed MA, Abdel-Mageed EG (2013) Minimally Invasive Treatment Protocol for Closed Pilon Fractures. Clin Res Foot Ankle 1:108. doi: 10.4172/2329-910X.1000108
Copyright: © 2013 Abdelgaid SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Introduction: high-energy injuries of distal tibia are usually associated with serious bony and soft tissues complications. Surgical options include biologic or open, internal or external fixation and primary arthrodesis with a lot of available fixation tools with no one treatment method has demonstrated superiority over others.
Material & Methods: from January 2007 to December 2010, 72 patients with closed pilon fractures managed by minimally invasive techniques according to a suggested protocol in the Al-Razi orthopedic hospital in Kuwait. Protocol is designed to choose minimally invasive treatment option depends on: 1) regional classification of soft tissue injuries, 2) grade of soft tissue injury & 3) degree of bony comminution.
Results: the mean follow up period was 34 months (range: 24–48 months). According to Tornetta clinical scoring system 35 (48.5%) patients were assessed as excellent, 29 patients with good results (40.5%), 5 patients (7%) assumed fair results and 3 patients (4%) had poor results. Using Teeny & Wiss radiologic scoring system, 43 patients (59.5%) achieved excellent results, 24 patients (33.5%) achieved good results, 4 patients (5.5%) with fair results and only one patient (1.5%) with poor result.
Conclusion: The designed protocol of minimally invasive treatment for closed pilon fractures provides the treating surgeon a variety of treatment options aiming to decrease the high rate of soft tissues and bony complications reported with these complex injuries.The unfavorable results will be decreased more if this protocol is combined with soft tissues stretching rehabilitation program and weight bearing is postponed until bony union become evident both clinically and radiologically.
Keywords
Pilon fracture; OTA/AO; Tscherne; Minimal invasive
Introduction
Pilon fractures are usually associated with significant soft tissue injury caused by high energy trauma, which may result in a series of complications such as fixation failure, skin flap necrosis or deep infection [1]. The most important predictors that influence the outcome of these injuries are soft-tissue management, the type of fracture, and quality of reduction [2].
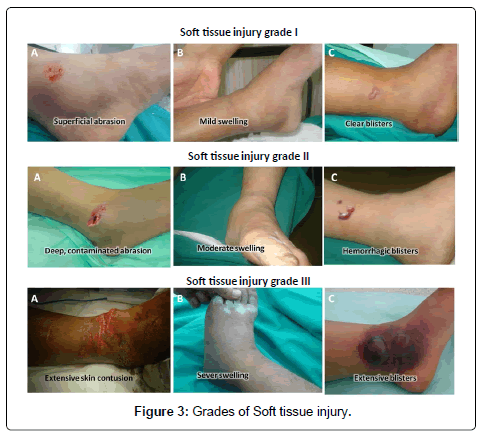
Recognizing and managing soft tissue injury is the most important aspect of treating closed fractures. Simple skin contusion over a closed fracture can pose more complex therapeutic and prognostic problems than skin which has been broken by a fractured bone [3]. Tscherne has proposed a classification of soft tissue damage based on the presence or absence of five lesions (abrasion, contusion, laceration, dissolving injury & compartment syndrome). Table 1 Swelling & fracture blisters are additional two important soft-tissue lesions not include in Tscherne classification. Swelling can be assessed and graded clinically, as loss of skin wrinkles and palpable landmarks (wrinkle sign) suggests moderate to severe swelling. Loss or delay of capillary refill and intraoperative blanching of the skin or loss of capillary refill with approximation of wound edges suggests severe swelling [4]. Fracture blisters are classified into: (1) Clear fluid–filled blisters which are probably not a reason to delay or alter surgical strategy and (2) Blood-filled blisters represent a deeper injury with a higher risk of poor healing and direct incision through them should be avoided. In the presence of blood-filled blisters and or severe swelling it is necessary to wait for the re-epithelialization of blisters and subsidence of skin swelling to avoid the significantly higher rate of complications. The disadvantage of delayed surgery is that a satisfactory reduction may become extremely difficult [4-10].
| Grade 0 | Minimal soft tissue damage Indirect injury to limb (torsion) Simple fracture pattern |
| Grade 1 | Superficial abrasion or contusion Mild fracture pattern |
| Grade 2 | Deep abrasion Skin or muscle contusion Severe fracture pattern Direct trauma to limb |
| Grade 3 | Extensive skin contusion or crush injury Severe damage to underlying muscle Compartment syndrome Subcutaneous avulsion |
Table 1: Tscherne classification system.
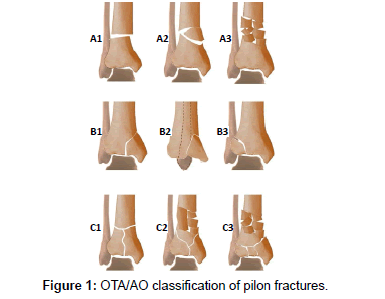
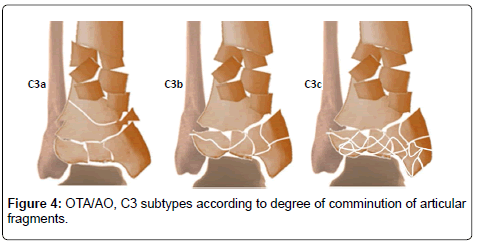
AO / OTA classified pilon fractures into three main subgroups: extra-articular, partial articular, and complete articular fractures (Figure 1) [11]. However, presence of small bone fragments without soft tissue attachment are responsible for the poor outcome with posttraumatic arthritis because of their insufficient reduction and high incidence of necrosis [12,13]. Fixation tool should be selected according to the degree and size of the fragments. Based on 3D CT, volumetric measurements of articular fragments categorized them into 3 sizes: major fragments (> 1000 mm3), minor fragments (500-1000 mm3) & small fragments (< 500 mm3) [14]. The treatment options include internal fixation, external fixation with or without limited internal fixation and primary arthrodesis which is reserved only for severe non-reconstructable articular comminution. To date, no one surgical treatment method has demonstrated superiority over others [15,16]. Open Reduction and Internal Fixation (ORIF) in high-energy distal tibia fractures, were associated with infection rates as high as 55%, wound sloughing rates as high as 36% and a few patients in multiple studies eventually required amputation [17]. Intramedullary Nailing (ILN) has the lowest infection rates but it is associated with other complications such as angular malunion, compartment syndrome and anterior knee pain [18,19]. For ILN, fractures should be > 2 cm from the articular surface with a minimum 2 and preferably 3 well distributed locking screws to provide sufficient stability [20]. External fixators (Ex. Fix) can be used in fractures with soft tissue damage that precludes plate and nail fixation. Its assembly should not jeopardize the attainment of an eventual coverage flap and avoid the course of a possible incision for future surgical treatment [12,21,22]. Hybrid fixator allows only a tibial assemblage with an inherent problem of cantilever bending which can be eliminated by the use of Ilizarov frame as cross-ankle circular Ex. Fix with the rate of fixation inefficiency is quite low [23-25]. Several authors combine an ankle-spanning Ex. Fix with percutaneous screws or wires fixation of articular fragments with good results and low complication rates [26-28]. Instead other authors suggested a staged treatment protocol consists of initial stage of fibular fixation and tibial Ex. Fix followed by a second stage of ORIF when soft tissue swelling has significantly diminished [29,30]. Recently, less invasive biological techniques were introduced in treatment of pilon fractures associated with expected fewer soft tissue complications and improve fracture healing. The emphasis lies on indirect reduction and stable fixation preserving most of the vascularisation and the osteogenic fracture haematoma which contains all growth factors necessary for bony healing [30].
Aim of work
Is to evaluate a protocol of minimally invasive treatment options for pilon fractures associated with soft tissues injuries. The protocol gives the surgeon a variety of appropriate treatment options based on the condition of soft tissue, type of bone fracture and the degree of comminution aiming to avoid soft tissue and bony union complications.
Materials and Methods
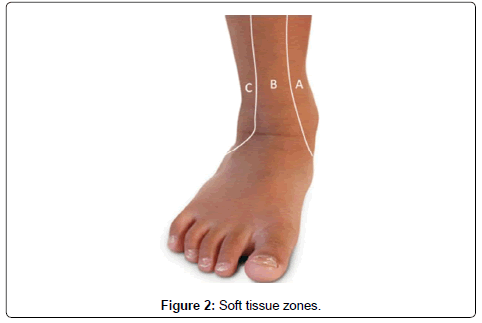
From January 2007 to December 2010, 72 patients (29 females & 43 males) with closed pilon fractures managed by minimally invasive techniques according to the suggested protocol in the Al-Razi orthopedic hospital in Kuwait. The mean age of the patients was 33 years (range, 19-66 years). The mechanism of injury was fall from height in 28 cases, motor vehicle accident in 25 cases, and simple fall 19 cases. Associated injuries were found in 17 patients. Our protocol depends on: 1) Regional classification of soft tissue injuries. 2) Grade of soft tissue injury. 3) Degree of bony affection. We classified the soft tissues around the ankle into three zones: zone one extends from anterior border of medial malleolus to anterior border of tendoachilles and covering the medial surface of tibia. Zone B is inter- malleolar covering the lateral surface of tibia. Zone C extends from anterior border of lateral malleolus to anterior border of tendoachilles covering the distal fibula. The aim of this classification is to use the appropriate fixation tool through healthy soft tissues decreasing its complications, e.g. using lateral distal tibia plate if blisters are present over the medial malleolus (Table 2 and Figure 2). We classified the soft tissue injuries into three grades including Tscherne criteria plus presence or absence of swelling and blisters. Grade I includes presence of one or more of superficial abrasion (Tscherne I), mild swelling or localized clear blisters. Grade II includes presence of one or more of deep contaminated abrasion (Tschene II), moderate swelling or localized hemorrhagic blisters. Grade III includes presence of one or more of extensive skin contusion, muscle destruction, compartment syndrome (Tscherne III), extensive blisters or severe swelling (Table 3a and Figure 3b). Using 3D-CT we further classified type OTA/AO type C3 into three subtypes. Type C3a; large fragments > 1 cubic cm, type C3b; intermediate fragments 0.5- 1 cubic cm & type C3c; small fragments < 0.5 cubic cm (Figure 4). Screw hole involves more than 30 % of the bone diameter concentrates the stress and makes the bone weaker under bending and torsional loading [33]. So, to prevent further comminution of fragments we fixed large fragments with 3.5 or 4.5 screws and fixed intermediate fragments with K wires. Small fragments either reduced by spanning Ex. Fix through ligamentotaxis or not. Unreduced small fragments were considered as indication for primary arthrodesis. All patients were positioned in supine position without use of tourniquet and under C-arm fluoroscopic control. If there was associated fracture of the distal fibula this was fixed.
| Associated fractures | Number of cases |
|---|---|
| Long bone (femur, humerus, B.B forearm or B.B leg) | 12 |
| Pelvis | 7 |
| Spine | 5 |
| Head injury (fracture skull bones) | 4 |
| Others | 2 cases fracture os calcis (one case bilateral) 2 cases fracture metatarsals 1 case patella + Bennett fractures |
Table 2: Associated skeletal injuries.
| Grade | Presence of one or more of the following: | ||
|---|---|---|---|
| Tscherne | Swelling | Blisters | |
| Soft tissue injury grade 0 | 0 | No | No |
| Soft tissue injury grade I: IA: localised to zone A IB: localised to zone B IC: localised to zone C |
I: Superficial abrasion |
Mild: Preservation of skin wrinkles and palpable landmarks |
Clear localized to one zone |
| Soft tissue injury grade II: IIA: localised to zone A IIB: localised to zone B IIC: localised to zone C |
II: Deep, contaminated abrasion with local contusion |
Moderate: Loss of skin wrinkles & palpable landmarks (wrinkle sign) |
Hemorrhagic localized to one zone |
| Soft tissue injury grade III : | III: Extensive skin contusion or crushing or muscle destruction |
Severe: loss or delay of capillary refill, either preoperatively or intraoperatively, with approximation of the wound edges |
Extensive Affecting two or more zone |
Table 3a: Grades of Soft tissue injury.
| Grade | Pain | Range of Motion | Angulation |
|---|---|---|---|
| Excellent | None | D > 5 | <3 |
| P > 40 | |||
| Good | Intermittent, relieved by NSAID | D = 0–5 | 3–5 valgus |
| P = 30–40 | <3 varus | ||
| Fair | Pain activities of DLA relieved by narcotics | D = −5–0 | 5–8 varus |
| P = 25–30 | 3–5 varus | ||
| Poor | Intractable | D < −5 | >8 valgus |
| P < 25 | >5 varus |
Table 3b: Criteria for Clinical Results (Tornetta) [28].
Surgical techniques were one of the following:
Intra-medullary nail fixation (ILN)
The standard entry point was identified at the proximal tibia and a guide pin was inserted and bridged the fracture. Correct guide pin position was confirmed with anteroposterior and lateral image intensification. The intramedullary canal was then reamed incrementally over a beaded-tip guide wire and an appropriately sized nail was inserted over ordinary tip guide wire. The nail was then locked proximally and distally with at least two screws.
Minimally Invasive Percutaneous Plate Osteosynthesis (MIPPO)
Articular fragments were reduced percutaneously & fixed by 3.5 mm lag screws. According to soft tissue condition a medial or anterolateral distal tibial plate of appropriate length was inserted in a sub-muscular retrograde way through 3cm incision. The limb length, rotation and angulation were adjusted. Plate was temporary fixed with K wires then approximated to the bone using conventional screws and finally locked in its site using locking screws.
Spanning external fixator with CRPS
Closed Reduction and Percutaneous Screws or CRPP (Closed Reduction & Percutaneous Screws): simple articular fragments (C1,2) and (C3a) were reduced by traction, direct pressure or manipulation with K.wires as a joystick and holding the fragments temporary with K wire or pointed reduction forceps. Fragments were then fixed percutaneously with cannulated 3.5 cannulated screws. In cases with complex articular fragments (C3b), fragments were reduced by ligament-taxis through calcanean traction and fixed with K. wires. Two Schanz screws were inserted through proximal tibial shaft and one transfixing pin through the calcaneus. Two tubular bars (one on each side of the leg) were connected to the tibial Schanz and calcanean pin. Fracture and limb rotation, length and angulation were adjusted before tightening the connectors.
Staged CRPP-CRPS Strategy (in cases with severe soft tissue injury)
Like spanning external fixator but the reduced articular fragments were fixed with K wires and after the soft tissue condition improved fragments were fixed with percutaneous cannulated screws.
Hybrid fixator
Articular fragments were manipulated and fixed as mentioned before. At least two transfix wires were applied with (60-90 ° angle in between) through the epiphyseal fragment. Then the wires were tensed and the ring was applied. Then two Schanz screws were inserted through proximal tibia and fixed to the ring using tubular bars and connectors after adjustment of limb and fracture alignment.
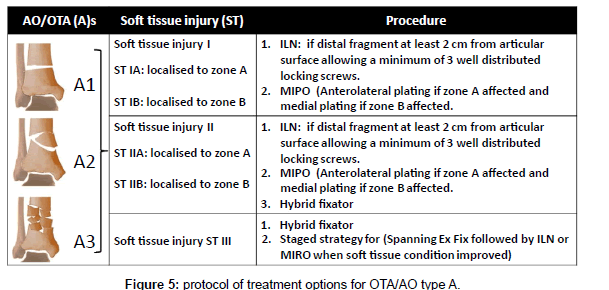
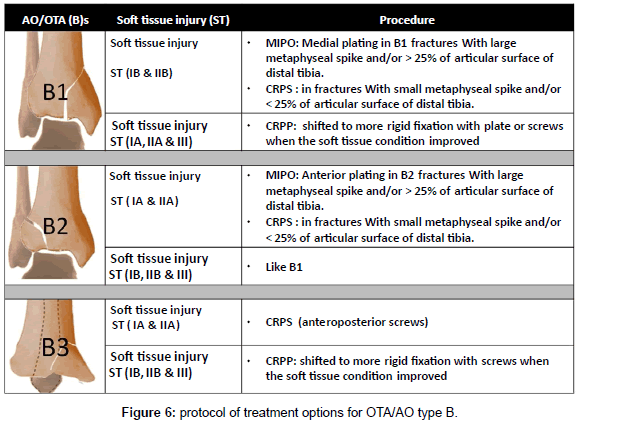
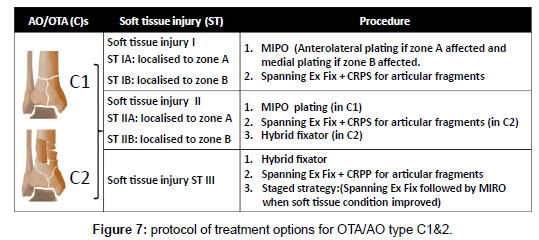
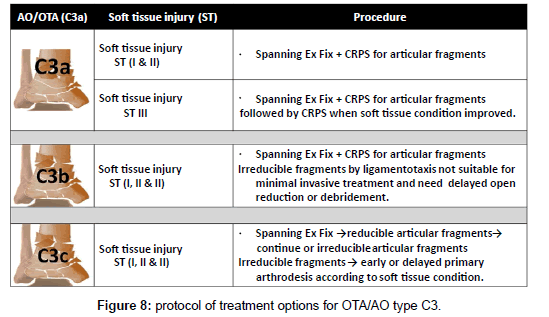
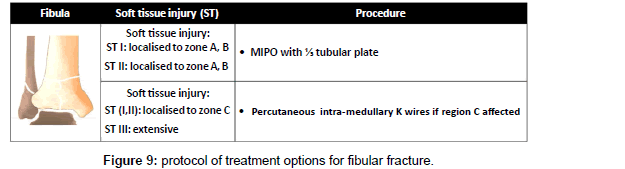
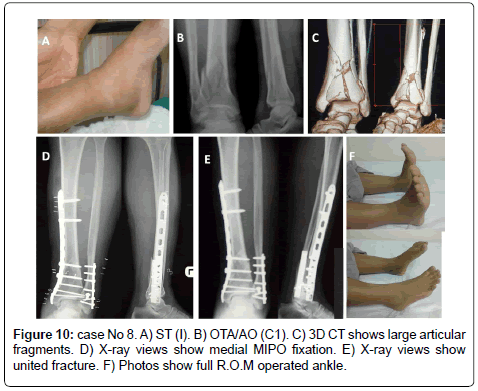
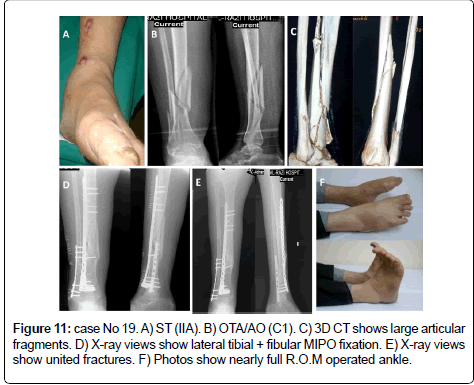
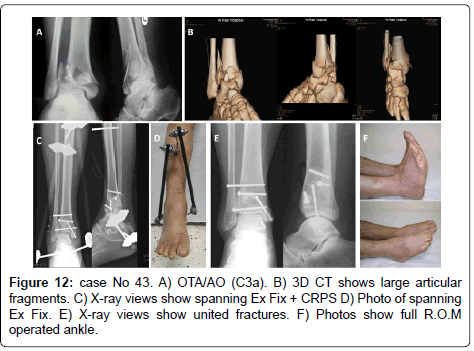
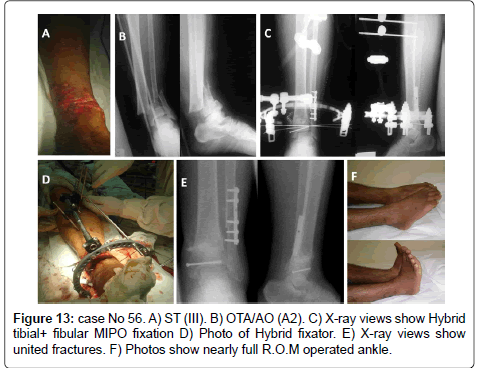
The method of treatment was selected according to the following protocol; in OTA types (A): in ST (I &II) ILN or medial or lateral MIPPO are preferred depending on the size of distal fragment and the zone of soft tissue injury. In ST (III) Hybrid fixator is preferred (Figure 5). In OTA types (B): ST (IB & IIB) in OTA type (B1) or ST (IA & IIA) in OTA type (B2) with large metaphyseal spike and/or involvement > 25% of articular surface of distal tibia is fixed by medial MIPPO type (B1) or lateral MIPPO in type (B2) fractures. Fractures with small metaphyseal spike and/or < 25% of articular surface of distal tibia are fixed by CRPS. ST (IA, IIA) in OTA type (B2) or ST (IB, IIB) in OTA type (B1) or ST (III) in OTA type (B1and 2) are fixed by staged CRPPCRPS strategy. OTA types (B3) are fixed anteroposterior CRPS if skin condition allowed otherwise are fixed by staged CRPP-CRPS strategy (Figure 6). In OTA types (C1 and C2): in ST (I) articular components are fixed first with CRPS & epiphyseal-diaphyseal components are fixed with MIPPO. While in ST (II & III) articular components are fixed first with CRPS or staged CRPP-CRPS strategy and epiphyseal-diaphyseal components are fixed with Ex Fix either hybrid or spanning tubular (Figure 7). In OTA types (C3): spanning external fixator is the treatment of choice with reduction of articular fragments depends mainly on ligamentotaxis. The percutaneous fixation method of articular fragment varies according to degree of comminution and soft tissue condition. Types C3A and C3b with reduced fragments are fixed by CRPS in ST (I& II), and by staged CRPP-CRPS strategy in ST (III). Types C3c and irreducible fragments in type C3b are not suitable for minimal invasive treatment and need early or delayed open reduction, debridement or arthrodesis depending on soft tissue condition (Figure 8). Associated fibular fractures: are fixed with ⅓ tubular plate using MIPO technique in ST (I) otherwise percutaneous intra-medullary K wires ST (CII & III), shifted later to plate fixation if reduction is not accepted when soft tissue condition is improved (Figure 9). Postoperatively in comminuted articular or metaphyseal fractures AFO brace was worn fulltime during 4 weeks. Patients were seen at the outpatient clinic weekly for the first month, biweekly until the end of the 3rd month and then at 4 weeks intervals until clinical and radiological union occurred. Full weight bearing was allowed after radiological consolidation of fractures when mature bridging callus was identified on two views without pain on full weight bearing. At follow-up, clinical assessment was carried out using Tornetta scoring system [28] & radiologic assessment using Teeny and Wiss scoring system [21] Osteoarthritis of the ankle was graded on the basis of radiological evidence as grade 0 (no change), grade 1 (small spurs, cysts or osteophytes without narrowing of the joint space), grade 2 (plus mild narrowing of the joint space and irregularity of the subchondral bone with some sclerosis) or grade 3 (large osteophytes, severe narrowing of the joint space and subchondral collapse) [13] (Figures 10-13).
Results
After a mean follow up period of 34 months (range: 24-48 months), 89 % of the patients were satisfied with the treatment and resumed their preoperative activities. According to Tornetta clinical scoring system 35 (48.5%) patients were assessed as excellent, 29 patients with good results (40.5%), 5 patients (7%) assumed fair results and 3 patients (4%) had poor results. Table 3b using Teeny and Wiss radiologic scoring system, 43 patients (59.5%) achieved anatomical reduction, 24 patients (33.5%) achieved good results, 4 patients (5.5%) with fair results and only one patient (1.5%) with poor result. Two patients showed wound dehiscence necessitated skin grafting. One case showed Ex. Fix and screws loosening. No patient suffered from deep infection, nerve entrapment or reflex sympathetic dystrophy. Three patients although their radiologic score were good, their clinical score were fair with pain during their daily living activities. These patients are heavy workers (laborers) and had grade III soft tissue injuries. Postoperatively they suffered painful swelling at the end of their working days. The two cases with fair clinical and radiologic scores had painful limited R.O.M of injured ankle with radiologic ankle and syndesmosis incongruities. One of these two cases, was 68 yrs old female severely osteoporotic and diabetic sustained C1 fracture pattern and grade III soft tissue injury treated by closed reduction + spanning Ex. Fix + CRPS for articular fragments. Due to osteoporosis loosening of the fixator & screws was occurred with resultant joint incongruities. The second case was drug addicted patient sustained C3b fracture with grade II soft tissue injury treated by spanning Ex. Fix + CRPP. He put early weight bearing and refused postoperative physiotherapy. Two of the three cases with poor clinical results, their radiologic results were fair and one case showed poor both radiologic and clinical scores. All of cases with poor clinical results gained these scores due to joint incongruities, painful limitations of ankle movements and angular deformity of the heel. The three cases sustained type C fractures (C2, C3a and C3b) respectively and soft tissue injury grade III plus concomitant fractures. The first case had bilateral fracture os calcis, the 2nd case was obese patient had contralateral fracture femur and the 3rd case had contralateral fractures femur and tibial plateau. All of these patients put early weight on the pilon side.
Discussion
High-energy injuries of distal tibia can cause serious damage to both soft tissues and bone in this area with an insufficient vascular structure. Failing to appreciate the soft tissue condition will invariably complicate the injury with infection, wound dehiscence or non union. Minor complications in the soft tissues increase the rate of major complications therefore delicate handling of the soft tissues by using minimally invasive techniques has been advocated for this type of fracture [33,34].
Relying on available treatment options we suggest a treatment protocol of minimally invasive techniques for closed pilon fractures aiming to decrease soft tissues and bony complications. The protocol depends on soft tissue condition, type & degree of comminution of bone. We extend Tscherne soft tissues injury classification to include two important criteria (swelling & blisters) due to their role in changing the type and time of treatment and altering the clinical results. Also we introduced regional classification of the soft tissues around the ankle as localized soft tissue injury to one zone can interfere with certain treatment options but not with others. We further classified the comminuted intraarticular fractures (OTA/AO type C3) according to the size of fragments on 3D CT evident based. The aim of this classification is to give a guide for treating surgeon for the suitable fixation method e.g. K.wire or screw fixation, or primary arthrodesis.
Our results highlights certain points: 1) Respecting the soft tissues in management of distal tibial fractures decrease the devastating complications since there were only two cases with wound dehiscence (<3%) and there was no cases with superficial or deep infections. 2) Increasing severity of soft tissues injury is proportional to increased bad prognosis; 0% in ST grade I, 8% in ST grade II & 20.5% in ST grade III. 3) Treatment journey does not ends with union of anatomical or accepted fractures but should extends to use physiotherapy to stretch the contracted soft tissues included in affected the zone(s). 4) Quality of bone (osteoporosis) is added problem in treatment of these cases and enhancement of bone quality by using adjuvant therapy like bone graft, bone healing enhancers and antiosteoprotic drugs should be incorporated in such treatment. 5) Spanning external fixator can be used as permanent treatment option without fair of postoperative stiffness (used in 36 patients of our study with only 6 cases16.5% developed mild to moderate permanent stiffness). This is matched with what was reported by Borelli et al in 2002. They found that early movement is only one of many major factors influence the final range of movement and determine the clinical results with intra-articular fractures [35]. 6) Weight bearing should be avoided until bony union become evident both clinically and radiologically. Patient susceptible to inevitable early weight bearing like those with concomitant contralateral lower limb fractures, the pilon fractured limb, should be protected in weight bearing brace.
Conclusion
The suggested protocol of minimally invasive treatment for closed pilon fractures associated with soft tissue injury provides the treating surgeon a variety of treatment options according to the soft tissue condition and the degree of articular comminution. The protocol is being designed to decrease the unwanted high rate of soft tissues and bony complications reported with these complex injuries. To optimize the clinical and radiologic results, the protocol should be combined with postoperative soft tissue stretching program prevents contracture of injured tissues and weight bearing should be started only when radiologic and clinical union was achieved.
References
- Tang X, Tang PF, Wang MY, Lü DC, Liu MZ, et al. (2012) Pilon fractures: a new classification and therapeutic strategies. Chin Med J (Engl) 125: 2487-2492.
- Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr (1999) A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 13: 78-84.
- Robinson CM, McLauchlan GJ, McLean IP, Court-Brown CM (1995) Distal metaphyseal fractures of the tibia with minimal involvement of the ankle. Classification and treatment by locked intramedullary nailing. J Bone Joint Surg Br 77: 781-787.
- Tscherne H, Lobenhoffer P (1993) Tibial plateau fractures. Management and expected results. Clin Orthop Relat Res : 87-100.
- Tull F, Borrelli J Jr (2003) Soft-tissue injury associated with closed fractures: evaluation and management. J Am Acad Orthop Surg 11: 431-438.
- Giordano CP, Koval KJ (1995) Treatment of fracture blisters: a prospective study of 53 cases. J Orthop Trauma 9: 171-176.
- Thordarson DB (2000) Complications after treatment of tibial pilon fractures: prevention and management strategies. J Am Acad Orthop Surg 8: 253-265.
- Tarkin IS, Clare MP, Marcantonio A, Pape HC (2008) An update on the management of high-energy pilon fractures. Injury 39: 142-154.
- Brumback RJ, McGarvey WC (1995) Fractures of the tibial plafond. Evolving treatment concepts for the pilon fracture. Orthop Clin North Am 26: 273-285.
- Bhattacharyya T, Crichlow R, Gobezie R, Kim E, Vrahas MS (2006) Complications associated with the posterolateral approach for pilon fractures. J Orthop Trauma 20: 104-107.
- Zelle BA, Bhandari M, Espiritu M, Koval KJ, Zlowodzki M; Evidence-Based Orthopaedic Trauma Working Group (2006) Treatment of distal tibia fractures without articular involvement: a systematic review of 1125 fractures. J Orthop Trauma 20: 76-79.
- Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, et al. (2011) Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg 77: 432-440.
- Okcu G, Aktuglu K (2004) Intra-articular fractures of the tibial plafond. A comparison of the results using articulated and ring external fixators. J Bone Joint Surg Br 86: 868-875.
- Guitton TG, Ring D (2010) Three-dimensional computed tomographic imaging and modeling in the upper extremity. Hand Clin 26: 447-453, viii.
- Hulscher JB, te Velde EA, Schuurman AH, Hoogendoorn JM, Kon M, et al. (2001) Arthrodesis after osteosynthesis and infection of the ankle joint. Injury 32: 145-152.
- Mauffrey C, Vasario G, Battiston B, Lewis C, Beazley J, et al. (2011) Tibial pilon fractures: a review of incidence, diagnosis, treatment, and complications. Acta Orthop Belg 77: 432-440.
- Bone L, Stegemann P, McNamara K, Seibel R (1993) External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res : 101-107.
- Im GI, Tae SK (2005) Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma 59: 1219-1223.
- Cheng W, Li Y, Manyi W (2011) Comparison study of two surgical options for distal tibia fracture-minimally invasive plate osteosynthesis vs. open reduction and internal fixation. Int Orthop 35: 737-742.
- https://www2.aofoundation.org/wps/portal/surgery
- Teeny SM, Wiss DA (1993) Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res : 108-117.
- Yildiz C, Atesalp AS, Demiralp B, Gur E (2003) High-velocity gunshot wounds of the tibial plafond managed with Ilizarov external fixation: a report of 13 cases. J Orthop Trauma 17: 421-429.
- Fischer MD, Gustilo RB, Varecka TF (1991) The timing of flap coverage, bone-grafting, and intramedullary nailing in patients who have a fracture of the tibial shaft with extensive soft-tissue injury. J Bone Joint Surg Am 73: 1316-1322.
- Laughlin RT, Calhoun JH (1995) Ring fixators for reconstruction of traumatic disorders of the foot and ankle. Orthop Clin North Am 26: 287-294.
- Watson JT, Moed BR, Karges DE, Cramer KE (2000) Pilon fractures. Treatment protocol based on severity of soft tissue injury. Clin Orthop Relat Res : 78-90.
- Marsh JL, Bonar S, Nepola JV, Decoster TA, Hurwitz SR (1995) Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am 77: 1498-1509.
- Helfet DL, Suk M (2004) Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect 53: 471-475.
- Tornetta P 3rd, Weiner L, Bergman M, Watnik N, Steuer J, et al. (1993) Pilon fractures: treatment with combined internal and external fixation. J Orthop Trauma 7: 489-496.
- Calori GM, Tagliabue L, Mazza E, de Bellis U, Pierannunzii L, et al. (2010) Tibial pilon fractures: which method of treatment? Injury 41: 1183-1190.
- Papadokostakis G, Kontakis G, Giannoudis P, Hadjipavlou A (2008) External fixation devices in the treatment of fractures of the tibial plafond: a systematic review of the literature. J Bone Joint Surg Br 90: 1-6.
- Fan CY, Chiang CC, Chuang TY, Chiu FY, Chen TH (2005) Interlocking nails for displaced metaphyseal fractures of the distal tibia. Injury 36: 669-674.
- Burstein AH, Currey J, Frankel VH, Heiple KG, Lunseth P, et al. (1972) Bone strength. The effect of screw holes. J Bone Joint Surg Am 54: 1143-1156.
- Mast JW, Spiegel PG, Pappas JN (1988) Fractures of the tibial pilon. Clin Orthop Relat Res : 68-82.
- Rammelt S, Endres T, Grass R, Zwipp H (2004) The role of external fixation in acute ankle trauma. Foot Ankle Clin 9: 455-474, vii-viii.
- Borrelli J Jr, Ellis E (2002) Pilon fractures: assessment and treatment. Orthop Clin North Am 33: 231-245, x.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 20505
- [From(publication date):
July-2013 - Jul 18, 2025] - Breakdown by view type
- HTML page views : 15649
- PDF downloads : 4856