Mesenteric Panniculitis as a Manifestation of Giardiasis in Tropical Regions: A Case Report
Received: 21-Nov-2022 / Manuscript No. JGDS-22-80515 / Editor assigned: 23-Nov-2022 / PreQC No. JGDS-22-80515 (PQ) / Reviewed: 07-Dec-2022 / QC No. JGDS-22-80515 / Revised: 28-Feb-2023 / Manuscript No. JGDS-22-80515 (R) / Published Date: 08-Mar-2023
Abstract
Background: Mesenteric panniculitis is a very rare gastroenterological condition, especially in adults. This patient had a very unorthodox manifestation of a common protozoal intestinal parasite. From this case, we can learn that in cases of non-specific abdominal pain with mesenteric panniculitis, we should also look for common intestinal protozoal parasites such as Giardia, Entamoeba, etc. This can apply to residents of tropical countries and even people who have recently travelled to a tropical region and experienced symptoms consistent with these findings.
Case presentation: A gentleman in his mid-50’s of Indian origin presented with a pinching type of non-specific mild abdominal discomfort for 10 months. The pain was episodic and was not associated with the consumption of any food. There was a prior history of acute pancreatitis and a CT scan was performed to rule out a potential recurrence of pancreatitis.
The CT imaging revealed mesenteric panniculitis in the jejunal area, with enlarged mesenteric lymph nodes. A follow-up CT scan 10 months later showed progression of the panniculitis with further enlargement of the lymph nodes in the jejunal mesentery. There were no signs of pyrexia, weight loss, altered bowel habits, nocturnal hyperhidrosis or generalized lymphadenopathy. A negative tuberculosis quantiferon test, along with the patient’s history and examination, were sufficient to rule out tuberculosis as a cause most blood tests were within normal physiological limits apart from a slightly elevated serum lactate dehydrogenase.
In view of mesenteric panniculitis involving the jejunal mesentery, a spiral enteroscopy was performed, which showed multiple non-specific segmental polypoid lesions in the jejunum, which appear to be Peyer’s patches. Subsequently, a colonoscopy was also performed to explore the large intestine, which appeared normal.
Biopsy results from the jejunum confirmed a finding of giardiasis. The patient was prescribed appropriate antiprotozoal therapy to eradicate the organism.
Conclusion: Mesenteric panniculitis can be a rare manifestation of giardiasis. In patients presenting with chronic mild abdominal pain who have a history of travelling to or visiting from a tropical region or country, mesenteric panniculitis should be in the differential during the clinical work up and investigations.
Keywords
Mesenteric panniculitis; Giardiasis; Sclerosing mesenteritis; Case report; Anti-protozoal
Introduction
Mesenteric panniculitis (also known as chronic sclerosing mesenteritis) is a disease process characterized by degeneration, inflammation and scarring of the adipose tissue of the mesentery. Although mesenteric panniculitis is an incidental finding that’s usually asymptomatic, the clinical presentations include but aren’t limited to abdominal pain, weight loss, nausea and vomiting. CT scan findings are usually diagnostic [1].
Mesenteric panniculitis is a very rare disorder. In the literature, there is no definite information on the occurrence of mesenteric panniculitis. Mesenteric panniculitis can occur on its own or in conjunction with other illnesses. Vasculitis, granulomatous disease, autoimmune disorders, hypersensitivity reactions, malignancies, pancreatitis, bacterial infections and abdominal trauma or surgery are all associated with the disease. In over 90% of cases, mesenteric panniculitis involves the small bowel mesentery [2].
In this case, we see a potential etiology of mesenteric panniculitis in parasitic infections of the gastrointestinal tract, such as Giardia lamblia.
Case Presentation
A man in his 50’s was referred to a gastroenterologist with a presentation of non-specific abdominal pain. The pain was spasmodic and usually localized to the left flank area; it occurred intermittently and it was mild to moderate in intensity. There were no aggravating or relieving factors for the pain and it manifested at random intervals. Fatigue and occasional malaise were the other associated symptoms. There was no prior history of abdominal surgery.
The patient initially presented 10 months ago with similar complaints and following radiological investigation, was diagnosed with mesenteric panniculitis and mesenteric lymphadenitis. It is also important to note that 5 months prior to the initial onset of these symptoms, the patient had an episode of acute pancreatitis, from which he made a complete recovery.
Initially suspecting an infectious etiology, a treatment protocol of a short term antibiotic course (combination of Ornidazole 500 mg and Ofloxacin 200 mg BD for 5 days) was prescribed and the patient felt relief from the symptoms for 2 weeks. Soon after, the original symptoms returned. The pain was not associated with consumption of food. There was no associated weight loss, no change in bowel habits and no history of tuberculosis. Also, there was no history of fever, nocturnal hyperhidrosis or evidence of enlarged cervical or axillary lymph nodes.
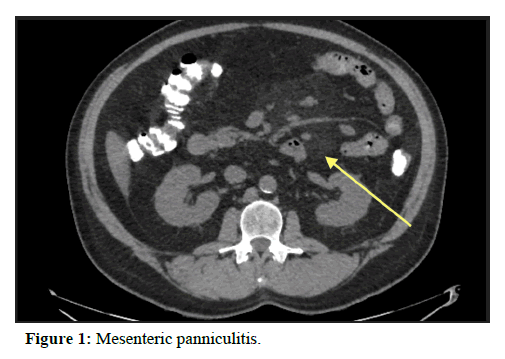
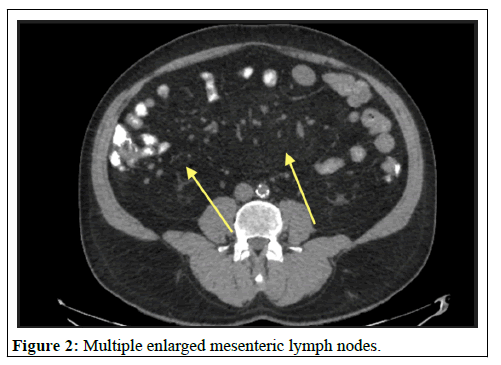
At the initial onset of symptoms, a CT scan of the abdomen revealed mesenteric panniculitis with prominent veins and multiple enlarged nodes measuring up to 10 mm.
A follow-up contrast enhanced CT scan performed 10 months after the initial onset of symptoms showed a further progression of mesenteric panniculitis (Figure 1), with further enlargement of lymph nodes in jejunal mesentery (largest nodes measuring 21 mm × 11 mm) (Figure 2).
Tuberculosis was negative (Gamma interferon quantiferon method). Blood tests revealed a mild increase in lactate dehydrogenase -258.8 IU/L (Reference interval: <248 IU/L). Liver and renal function tests were normal.
Serum autoimmune markers (Anti-phospholipid Abs, anticardiolipin Abs, anti-ANA Abs) were negative.
In view of the CT scan findings, an enteroscopy was performed. Multiple non-specific segmental polypoid lesions in the jejunum were seen, which appeared to be Peyer’s patches. Biopsies of the lesions were taken.
A colonoscopy was also performed. The entire large intestine and the terminal ileum appeared normal.
Microscopic examination of jejunal biopsies showed moderate lymphoplasmacytic infiltrates with prominent numerous lymphoid follicles. Surface of villi showed slender tear drop shaped organisms. Features were suggestive of giardiasis (Figure 3).
The examination was negative for atypical cells or malignancy. This patient was treated with Tinidazole 600 mg TDS for a duration of 2 weeks. The patient adhered to the treatment. The patient expressed a decrease in incidence of symptoms after the course of anti-protozoal treatment. Follow-up enteroscopy can be considered if symptoms recur. A follow-up CT scan was deemed unnecessary until a recurrence occurred. There were no unanticipated or adverse events during treatment and follow-up.
Discussion
In this case, ruling out other differential diagnoses was crucial. Often, mesenteric panniculitis can be secondary to autoimmune disease. This includes the fact that biopsies show chronic and progressive inflammation. Patients with mesenteric panniculitis may also experience systemic symptoms such as fever and fatigue, which are also seen in other autoimmune disorders like rheumatoid arthritis and Crohn's disease. Additionally, patients with mesenteric panniculitis tend to have a strong family history of autoimmune disorders. Notably serum inflammatory indicators such as the Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) are frequently elevated in these patients. But, in this case, these inflammatory markers were within normal range. Moreover, in this case, other serum autoimmune markers (Anti phospholipid Abs, anticardiolipin Abs, anti-ANA Abs) tested negative.
Case studies have suggested that mesenteric panniculitis is a paraneoplastic process. A significant number of patients with mesenteric anomalies associated with mesenteric panniculitis may have an underlying malignancy. Progressively enlarging abdominal lymph nodes (especially >1 cm) are associated with lymphomas. Mesenteric lymphomas represent a localized process, or they may be a sign of more disseminated disease. Although mesenteric lymphomas are uncommon (1 case per 200,000-350,000 population) given the symptomatology and elevated serum LDH levels, this was a wellfounded differential diagnosis. It was ruled out after finding substantial evidence of giardiasis [3].
Multiple case reports of mesenteric panniculitis indicate a history of chronic infections such as intestinal tuberculosis. Enlarged abdominal lymph nodes, chronic fatigue and malaise indicated a possible diagnosis of tuberculosis. However, a negative TB quantiferon test ruled out the diagnosis during investigations [4-6].
Conclusions
By eliminating the other possible etiologies, it was concluded that giardiasis was most likely. From this case, they key takeaways and potential implications are:
• Mesenteric panniculitis is a very rare gastroenterology condition. Clinical awareness of this condition will help diagnose more cases and improve treatment protocols.
• Mesenteric panniculitis can clinically mimic other chronic conditions.
• Mesenteric panniculitis can be a rare manifestation of chronic giardiasis.
• In adult patients with mesenteric panniculitis, we need to look for potential protozoan infections such as amoebiasis, giardiasis, especially in patients residing in or returning from tropical regions the Indian subcontinent, Africa and South-East Asia, etc.
• Treating the underlying cause, in this case, a protozoal infection can relieve symptoms.
• The cause of mesenteric panniculitis can be narrowed down by taking biopsies from the small bowel during an enteroscopy.
Because this is a one of a kind case report, more cases like it need to be independently reported and published for the conclusions of this manuscript to be proven scientifically.
Consent for Publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor in chief of this journal.
References
- Hussein MRA, Abdelwahed SR (2015) Mesenteric panniculitis: An update. Expert Rev Gastroenterol Hepatol 9: 67-78. [Crossref] [Google Scholar] [PubMed]
- Gunduz Y, Tatli L, Kara RO (2021) Mesenteric panniculitis: A case report and review of the literature. Maedica (Bucur) 7: 344-347. [Google Scholar] [PubMed]
- Ciortan E, Carra L (2010) Abdominal mass as the first sign of follicular lymphoma B of mesentery: Case report. J Ultrasound 13: 123-125. [Crossref] [Google Scholar] [PubMed]
- Nicholson JA, Smith D, Diab M, Scott MH (2010) Mesenteric panniculitis in Merseyside: A case series and a review of the literature. Ann R Coll Surg Engl 92: e31-e34. [Crossref] [Google Scholar] [PubMed]
- Ginsburg PM, Ehrenpreis ED (2002) A pilot study of thalidomide for patients with symptomatic mesenteric panniculitis. Aliment Pharmacol Ther 16: 2115-2122. [Crossref] [Google Scholar] [PubMed]
- Adachi Y, Mori M, Enjoji M, Ueo H, Sugimachi K (1987) Mesenteric panniculitis of the colon: Review of the literature and report of two cases. Dis Colon Rectum 30: 962-696. [Crossref] [Google Scholar] [PubMed]
Citation: Puli CS, Godavarthy PK (2023) Mesenteric Panniculitis as a Manifestation of Giardiasis in Tropical Regions: A Case Report. J Gastrointest Dig Syst 13:726
Copyright: © 2023 Puli CS, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1973
- [From(publication date): 0-2023 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 1643
- PDF downloads: 330