Case Report Open Access
Mesenteric Lymphangioma with Small Intestinal Volvulus in an Adult
Hyun-Dong Chae1*, Chang-Ho Cho2 and In-Hwan Kim11Department of Surgery, School of Medicine, Daegu Catholic University Hospital, Daegu, Korea
2Department of Pathology, School of Medicine, Daegu Catholic University Hospital, Daegu, Korea
- *Corresponding Author:
- Hyun-dong Chae
Department of Surgery
School of Medicine, Daegu Catholic University Hospital
3056-6, Daemyung-4-Dong, Namgu
705-718, Daegu, Korea
Tel: 82536504429
Fax: 82536247185
E-mail: hdchae@cu.ac.kr
Received date: January 13, 2017; Accepted date: February 08, 2017; Published date: February 15, 2017
Citation: Chae H, Cho C, Kim I (2017) Mesenteric Lymphangioma with Small Intestinal Volvulus in an Adult. J Gastrointest Dig Syst 7:485. doi: 10.4172/2161-069X.1000485
Copyright: © 2017 Chae H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Lymphangioma occur commonly in the neck and axillae of pediatric patients, caused by an obstruction of the lymphatic flow because of congenital lymphatic malformation. However, mesenteric lmphangioma of the small intestine is a rare tumor that is seldom associated with small bowel volvulus, particularly in adult patients. Although rare, mesenteric lymphangioma can cause volvulus and intestinal obstruction by a torsion of mesentery. We report an unusual case of mesenteric lymphangioma with small bowel volvulus who was suffered from intermittent abdominal pain, treated with surgical resection.
Keywords
Lymphangioma; Small intestine; Volvulus; Mesentery
Introduction
Lymphangioma is a benign condition characterized by proliferation of the lymphatic space, resulting from blockage of regional lymph ducts. It is believed that lymphangioma is caused by a congenital malformation and obstruction of lymphatic system rather than a true neoplasm derived from lymphatic tissue [1]. It is usually found in the head and neck during childhood, with varying symptoms according to the location of development.
Intra-abdominal lymphangiomas can occur in various sites such as mesentery, mesocolon, omentum, and retroperitoneum. Although mesentery is the most common site of intra-abdominal lymphangiomas, mesenteric lymphangioma is rare among all lymphangiomas which has been reported in <1% [1].
The clinical presentation of mesenteric lymphangioma varies depending on its size and location. The most common symptoms are vague abdominal pain and distension, but most of mesenteric lymphangiomas are asymptomatic until they enlarge. Complications of mesenteric lymphangioma, such as secondary infection, rupture with hemorrhage, volvulus, or intestinal obstruction, have been reported [2].
Small bowel volvulus induced due to mesenteric traction by the mass is a rare manifestation of mesenteric lymphangioma [3]. The present case of mesenteric lymphangioma with small bowel volvulus in an adult patient is rare. Therefore, we report this successfully treated case with a brief review of the relevant literature.
Case Report
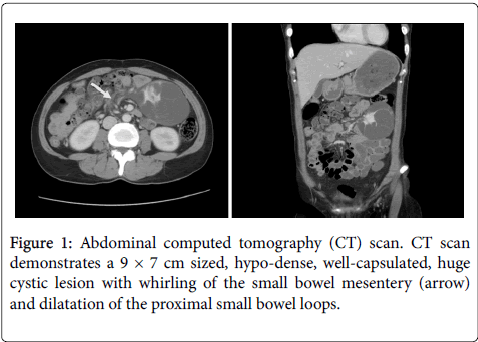
A 37-year-old woman was admitted to emergency services with abdominal pain. She had recently experienced epigastralgia and abdominal fullness for the several months. She was suffered from intermittent low abdominal squeezing pain for the past 2 weeks. The duration of pain was several minutes, and subsided spontaneously. At the day of visiting emergency room, she had felt severe abdominal pain for 2 hours, which was not subsided. She had no underlying medical disease, specific medication, trauma, or history of abdominal surgery. A physical examination revealed a mass in the left upper quadrant of the abdomen with tenderness, but no rebound tenderness. Laboratory data including tumor markers were within normal limits. A plain film of the abdomen showed several loops of the small intestine without dilatation or air-fluid level. Abdominal ultrasonography revealed a large, multilocular, cystic mass with an obscure margin. An abdominopelvic computed tomography (CT) scan was taken. CT scan showed a 9 × 7 cm, well-capsulated cystic mass located in the left upper side of abdominal cavity with whirling of the small bowel mesentery and dilatation of the proximal small bowel loops, which suggested volvulus of the small intestine (Figure 1). There were no signs of small intestinal ischemia, and the finding showed partial rather than complete obstruction.
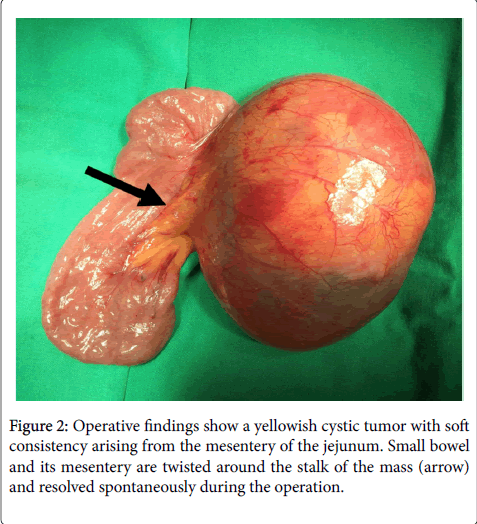
Although there was don evidence of small intestinal ischemia, we decided to perform emergent surgery because of intestinal obstruction due to mass lesion, and possibility of malignant disease. A median incision was made in the upper abdominal region under general anesthesia. At laparotomy, small bowel and its mesentery were twisted around the stalk of the mass and resolved spontaneously during the operation. A soft cystic mass was located in the mesentery of the jejunum, about 30 cm distal to Treitz’s ligament (Figure 2). The tumor was not adhered to the intestinal wall or adjacent organs. No ascites was seen in the peritoneal cavity. The tumor was resected completely by carefully dissecting the mesenteric vessels but without resecting the intestine.
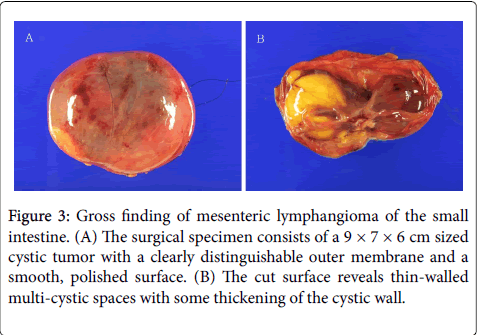
The specimen consisted of a 9 × 7 × 6 cm cystic tumor in the mesentery of the small intestine. The mass had a clearly distinguishable outer membrane, a smooth, polished surface, and signs of swelling due to the liquid it contained. The sectioned specimen contained serous liquid and a large swollen cyst. Small multi-septated cystic masses of various sizes were also situated along some of the thicker portions of the cystic wall (Figure 3).
Figure 3: Gross finding of mesenteric lymphangioma of the small intestine. (A) The surgical specimen consists of a 9 × 7 × 6 cm sized cystic tumor with a clearly distinguishable outer membrane and a smooth, polished surface. (B) The cut surface reveals thin-walled multi-cystic spaces with some thickening of the cystic wall.
Pathological findings showed that the mass was comprised of a number of multi-septated cystic masses of varying sizes that were wrapped with flat lymphatic endothelial cells. Some lymphatic infiltration was found in the mass.
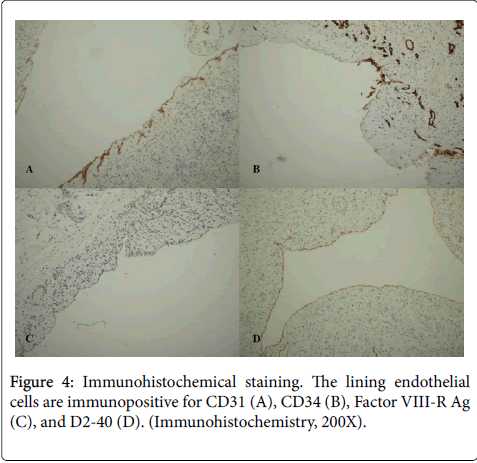
Immunohistochemical stain showed that the cells at the cystic wall reacted strongly to CD31, CD34, Factor VIII-R Ag, and D2-40 (Figure 4). Diagnosis of mesenteric lymphangioma of the small intestine was made according to the pathologic finding including immunohistochemistry. There was no postoperative problem without any complication. She recovered well and started to have soft meal at 3days after surgery. She was discharged uneventfully on postoperative day 9. She was doing well at the 3-month follow-up examination.
Discussion
Lymphangioma is a mass-forming lesion characterized by numerous thin-walled lymphatic spaces. The most common sites are the head, neck, and axillary regions. Other locations, such as the abdominal or mediastinal cavity, are rare, accounting for approximately 5% of lymphangiomas. Among these, lymphangioma of the small-bowel mesentery has been described in <1% of lymphangiomas [1].
Mesenteric lymphangiomas are usually asymptomatic until they enlarge. The most common symptoms are a palpable abdominal mass and abdominal distension. Mesenteric lymphangioma can cause intestinal obstruction by compression of large mass to small intestine, or traction of mass leading to small intestinal volvulus [4]. In this case, a large-sized (9 × 7 cm) mesenteric lymphangioma lead to a partial intestinal obstruction by a small bowel volvulus induced due to mesenteric traction by the mass without compression due to chronic development.
The pathogenesis of lymphangioma remains unclear. Aberrant sequestration of certain lymphatic vessels during development has been suggested as a cause. Two hypotheses have been proposed for the etiopathogenesis of mesenteric lymphangioma. First, it is probably a congenital malformation that causes sequestration of lymphatic tissue during embryological development. This hypothesis explains why lymphangiomas occur primarily in children. Second, it has been suggested that abdominal trauma, lymphatic obstruction, inflammation, surgery, or radiation therapy can lead to secondary formation of a lymphangioma in adults. A mesenteric lymphangioma generally forms as a unilocular cystic mass without internal septa [5] and chronic intermittent volvulus may lead to venous and lymphatic congestion of the mesentery. Then, lymphatic drainage is compromised and intestinal obstruction may arise from a unilocular cystic lymphangioma.
Lymphangiomas are traditionally classified into capillary (simple), cavernous, and cystic types [6]. Findings of cystic lymphangioma are similar to those of cavernous lymphangioma in that dilated lymphatic spaces of various sizes are seen in both [5]. However, cystic lymphangioma is not always clearly differentiated from the cavernous type because the cystic type may also contain cavernous areas [6]. Lymphangioma can also be classified as microcystic, macrocystic, and mixed based on cyst size. Microcystic lymphangiomas consist of cysts <2 cm, whereas macrocystic lymphangioma are >2 cm. The mixed type has variable-sized cysts, containing both microcysts and macrocysts [7]. According to these classifications, our case would be classified as a macrocytic, cystic, mesenteric lymphangioma of the small intestine.
Due to the nonspecific and varying presentation, preoperatively diagnosing a mesenteric lymphangioma can be challenging. Abdominal sonography shows a well-confined uni or multiloculated liquid-filled tumor with thin septations. The cystic content is usually sonolucent, but may be echogenic when intracystic bleeding or calcifications are present. An abdominal CT scan allows evaluation of the water density of the tumor, its relationship with neighboring organs, and definitions the mass effect on the intestines [8].
Diagnostic confirmation of a mesenteric lymphangioma is pathologically possible. A microscopic examination reveals flat endothelial cells bordering the cystic membrane and diversified lymph cells in the cystic membrane or lymphatic ducts. Immunohistochemistry can be used to increase the accuracy of diagnosis. Staining with Factor VIII-R Ag, CD31, CD34, and D2-40 produces a response to mesenteric lymphangioma [9]. In our case, the endothelial cells responded to immunochemical staining, which allowed the diagnosis of mesenteric lymphangioma (Figure 4).
Although generally considered benign, Mesenteric lymphangiomas somtimes have poor prognosis because of rupture, leakage, or infiltration to adjacent organ, when their sizes are increasing continuously. Complete resection is the first-choice treatment for suspicion of a mesenteric lymphangioma. Some researchers have proposed intracystic injections of sclerosing agents for non-resectable lesions, when radical resection might be technically impossible [8]. Rarely, mesenteric lymphangioma can cause fatal complications, such as volvulus or involvement of the main branch of the mesenteric arteries requiring emergency surgery, particularly in adults [6]. In the present case, small bowel and its mesentery are twisted around the stalk of the mass, but resolved spontaneously during the operation. The tumor had not adhered to the wall of the intestine or adjacent organs. No ascites was seen in the peritoneal cavity and inflammatory changes were detected in the intestines or mesentery. The tumor was resected completely without resecting the intestine. No complications, such as leakage of lymphatic liquid, were seen after the procedure.
We report this case to remind that mesenteric lymphangioma can cause volvulus of small intestine, and emphasize the importance of surgical resection when patients have symptoms of intestinal obstruction or volvulus due to mesenteric lymphangiomas.
Conflicts of Interest
We have no conflicts of interest to disclose and received no funding from the manufacturer of any drug, treatment, or device for conducting this study.
References
- Jang JH, Lee SL, Ku YM, An CH, Chang ED (2009) Small bowel volvulus induced by mesenteric lymphangioma in an adult: a case report. Korean J Radiol10:319-322.
- Yoon HK, Han BK (1998) Chronic midgut volvulus with mesenteric lymphangioma: a case report. PediatrRadiol 28:611.
- Campbell WJ, Irwin ST, Biggart JD (1991) Benign lymphangioma of the jejunal mesentery: an unusual cause of small bowel obstruction. Gut 32:1568.
- Mar CR, Pushpanathan C, Price D, Cramer B (2003) Best cases fromthe AFIP: omentallymphangioma with small-bowel volvulus.Radiographics23:847-851.
- Traubici J, Daneman A, Wales P, Gibbs D, Fecteau A, et al. (2002) Mesenteric lymphatic malformation associated with small bowelvolvulus-two cases and a review of literature. PediatrRadiol32:362-365.
- Chen CW, Hsu SD, Lin CH, Cheng MF, Yu JC (2005) Cysticlymphangioma of the jejunal mesentery in an adult: a casereport. World J Gastroenterol 11:5084-5086.
- Prabhu SM, Anand R, Narula MK, Shetty GS, Udiya AK, Chauhan U, et al. (2012) Mesenteric cysts associated with recurrent small-bowel volvulus: cause or effect? Jpn J Radiol 30: 858-862.
- Tsukada H, Takaori K, Ishiguro S, et al (2002) Giant cystic lymphangiomaof the small bowel mesentery: report of a case. Surg Today32:734-737.
- Colovic RB, Grubor NM, Micev MT, Atkinson HD, Rankovic VI, et al. (2008) Cystic lymphangioma of thepancreas. World J Gastroenterol14:6873-6875.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 6132
- [From(publication date):
February-2017 - Jul 15, 2025] - Breakdown by view type
- HTML page views : 5180
- PDF downloads : 952