Mesenchymal Stem Cells Reverse the Pathophysiology of Cerebral Malaria Induced by Plasmodium berghei ANKA
Received: 04-Nov-2022 / Manuscript No. JCEP-22-79037 / Editor assigned: 07-Nov-2022 / PreQC No. JCEP-22-79037 (PQ) / Reviewed: 23-Nov-2022 / QC No. JCEP-22-79037 / Revised: 30-Nov-2022 / Manuscript No. JCEP-22-79037 (R) / Published Date: 07-Dec-2022
Abstract
Cerebral malaria-associated over expression of pro-inflammatory cytokines and chemokines ultimately results in the up-regulation of adhesion molecules in the brain endothelium leading to sequestration of mature parasitized RBCs in the brain. The high-parasitic load subsequently results in increased mortality or development of neurological symptoms within a week of infection. Studies in the human and experimental cerebral malaria have implicated the breakdown of the integrity of blood-brain barrier during the lethal course of infection, cerebral dysfunction, and fatal organ pathologies that result in multi-organ failure. In the present study, using Plasmodium berghei ANKA (PbANKA) as a mouse model and in vitro conditions, we have investigated the effect of MSCs to attenuate Cerebral malaria pathogenesis by diminishing the effect of inflammation altered organ morphology, reduced parasitemia and increased survival of the mice. MSCs are also validated for their role in preventing BBB dysfunction and reducing malarial toxins. It was observed that administration of MSCs significantly reduced parasitemia and increased survival in PbANKA infected mice. It was further demonstrated that MSCs play a significant role in reversing neurological complexities associated with cerebral malaria. Infusion of MSCs in infected mice decreased hemozoin deposition, oedema and heamorrhagic lesions in vascular organs. MSCs administration also preserved the integrity of the blood-brain barrier and reduced neural inflammation. Taken together, our results demonstrate the potential of MSCs as an emerging anti- malarial candidate.
Keywords: Cerebral malaria; Leukocytes; Cytokines
Introduction
Malaria is one of the most fatal parasitic diseases and serious world health concern. It results from the infection of parasites belonging to the genus Plasmodium. Severe malaria caused by P. falciparum is responsible for approximately a third of the disease- associated deaths [1,2]. According to the recent world malaria report, an estimated 241 million cases of malaria were estimated in 2020. The primary neurological complication arises in cerebral malaria infection, associated with multiple organ dysfunctions triggered by circulating parasitized red blood cells [3,4]. The clinical implications of cerebral malaria include disruption of the Blood-Brain-Barrier (BBB) and systemic inflammatory responses, including the production of cytokines and activation of inflammatory cells [5]. Disruption of the blood- brain barrier facilitates the movement of leukocytes, cytokines, inflammatory cells, chemokines, and phagocytosed parasite products across the brain parenchyma and wherein they activate astrocytes and microglia of the brain, ultimately resulting in neuronal tissue degeneration and subsequent inflammation [6-8]. In humans and rodent malaria models, insufficient erythropoiesis is a significant factor contributing to malarial anaemia [2,9-11]. However, the exact molecular mechanisms underlying malarial anaemia are mainly unknown. One of the significant factors contributing to malarial anaemia is the “malaria toxin”, hemozoin. During malaria infection, the free heme or hematin produced by the proteases as result of degradation of host haemoglobin is further metabolized by the parasite and converted into insoluble toxic biocrystal hemozoin. The total amount of hemozoin in the host indicates parasite load that induces undesirable consequences such as activation of macrophages and dendritic cells to induce inflammation, dyserythropoiesis and impaired erythrocytic cells generation [12]. Another major hallmark of malaria pathogenesis is the modulation of the immune response [13,14]. Cerebral malaria has been shown to exhibit accumulation of leukocytes and iRBCs in the capillaries of vascular organs such as the brain, lungs, liver, intestine, etc. These leukocytes enhance the production of cytokines and chemokines inducing local inflammation and challenges the integrity of the BBB. The infiltrating T-cells induce apoptosis of ECs through granzyme B and perforin-mediated cytotoxicity. Although a substantial progress has been made over the past few years to reduce the high level of suffering, the current anti-malarials are incapable of preventing the death of severe cerebral malaria and thus, the control of malaria remains the greatest challenge worldwide [15]. Nevertheless, the intensification of resistance to the available anti-malarial drugs highlights the threat for recurrence of epidemics in major parts of the world. Therefore, it is imperative to conduct clinically significant research to stay one step ahead. Novel drugs and drug combinations are needed, particularly those with innovative mechanisms that can impair the capability of parasite to emerge and multiply. Because of the intricacies involved, the study of severe malaria requires a “systematic approach” for appropriate and comprehensive understanding of defects in both erythropoietic and immune response associated with the disease. Over the past few years, therapeutic strategies of Mesenchymal Stem Cells (MSCs) have emerged as a major breakthrough against several diseases including cancer, autoimmune diseases and neurological disorders. The therapeutic potential of MSCs are attributed to their plasticity, self- renewal potential, ability to differentiate into various tissues, repair and regeneration of damaged tissue, and modulation of immune response.
Materials and Methods
Malaria parasite
Cryopreserved P. berghei ANKA parasites were used for all experimental procedures. The plasmodia were retrieved from the parasite bank, and infection was initiated by intraperitoneal injection of the syngenic strain of mice.
Experimental animals and infection
All animal experiments performed were approved by the Institutional Animal Ethic Committee of National Institute of Malaria Research (IAEC-NIMR) with approval number IAEC/NIMR/2021-1/04. All methods were carried out in accordance with Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA) guidelines and regulations.
The experiments were carried out in Female C57BL/6NCrL mice of 6 to 8 weeks old weighing 22 ± 0.5 gm. The animals were purchased from HYLASCO Biotechnology (INDIA) Pvt. Ltd. and maintained in the animal facility of National Institute of Malaria Research (NIMR), New Delhi, India under the controlled conditions of temperature, humidity and light. Mice were infected with P. berghei ANKA intra-peritoneal injection with 5 × 105 syngenic parasitized erythrocytes (pRBCs).
Determination of parasitemia
Blood samples were collected from experimental mice by bleeding via the tail vein at times indicated to determine the course of infection. Duplicate thin blood smears were prepared and stained with Giemsa. Parasitemia was determined by counting the infected cells per 10000 RBC per slide. The parasitemia is generally expressed as the mean percentage of pRBC+Standard Error of the Mean (SEM) for each group of mice.
Isolation of MSC cells
Female C57BL/6 mice were euthanized by CO2 inhalation to isolate the MSCs. MSCs were sorted from splenocytes by positive selection after depleting lin+cells using the beads from MiltenyiBiotec. The (3-5 × 106) cells were used for adoptive transfer in the syngenic animals.
Histological examination and hemozoin quantification
Spleens from infected animals as well as animals infused with MSCs were taken out mice and processed for histopathological analysis and hemozoin quantification. For Histological examination, small part of each spleen was fixed in 4% paraformaldehyde and subsequently these formalin fixed tissues were embedded in paraffin followed by cutting into into 5 µm thin sections. These sections were examined using bright-field microscopy coupled with Hematoxylin and Eosin (H&E) staining according to standard protocols. The results were confirmed by observation of atleast ten fields per group in a double-blinded manner. Another small part of spleen was frozen for hemozoin quantification. Cryogenically stored spleen tissues were thawed and processed to detect and quantify Hemozoin content as described by Pisciotta et al. [17]. Briefly, spleen isolated from control and infected mice with or without MSC treatment were homogenized, suspended in lysis solution containing 5 ml of deionized H2O and pulse sonicated using sonicator. Lysed spleen tissue was centrifuged at 14000×g for 15 min. Following centrifugation, supernatant was removed and pellets containing hemozoin were resuspended in 1 ml solution containing 2% SDS, 100 mm sodium bicarbonate and again centrifuged at 14000×g for 15 min. Pellets were washed twice with 2% SDS and washed pellets were resuspended again and incubated overnight in 1 mg/ml proteinase K Buffer at 600 C. After incubation, pellets were washed with deionized H2O and the purified hemozoin pellets were solubilized in 1 ml solution of 2% SDS and 20 mm NaOH for 1 h. Finally, all samples were quantified spectrophotometrically at absorbance of 400 nm with molar extinction coefficient of 1 × 105.
Results
MSC infusion prolongs survival, reduce parasitaemia and maintains the body’s physiology in PbANKA infected mice
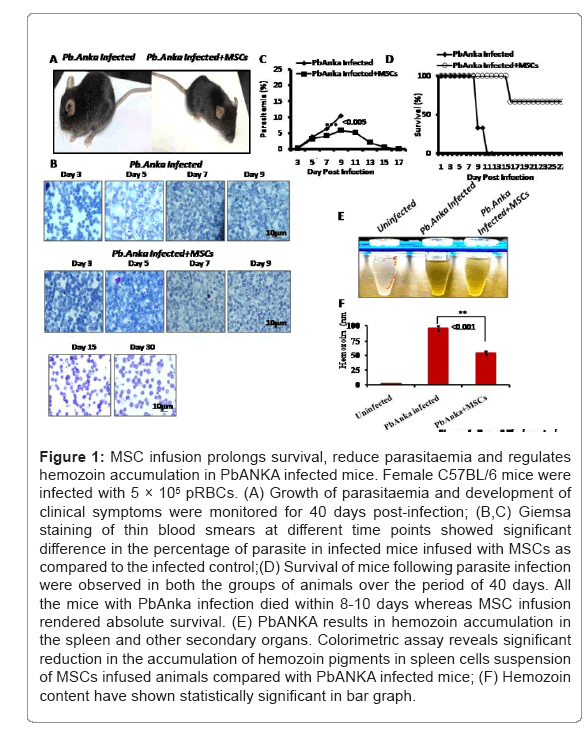
To determine the physiological role of MSCs in cerebral malaria pathogenesis, C57BL/6 mice were infused with MSCs and then challenged with the malaria parasite. The animals were then observed for their parasitemia and survival for 40 days after infection. The severity of the disease was determined by scoring various parameters such as appearance (normal, coat ruffled or coat staring, panting), behaviour (normal, hunched, mobility, convulsions etc.), food and water intake, body temperature (Figure 1A). It was observed that C57BL/6 mice were highly susceptible to PbANKA infection and displayed absolute mortality within 10 days of infection. On the other hand, with MSC infusion in infected animals, there was an initial rise in parasitemia till day 9-11. However, a progressive reduction in parasite content was observed post 11th day in thin blood smear (Figure 1B), and eventually, it gets cleared (Figure 1C). Moreover, the average survival rate of the mice was observed after MSC infusion in infected animals (Figure 1D). The surviving mice did not display any significant physiological and behavioral alterations. Colorimetric analysis have shown reduction of hemozoin contents in MSCs infused PbANKA infected animals (Figures 1E and 1F) (Figure 1 and Table 1).
| Clinical observation | Clinical score | ||
|---|---|---|---|
| No burden on animals, animals healthy | 0-3 | ||
| low burden on animals, low sickness, animals are observed | 04-Sep | ||
| moderate burden on animals, moderate sickness, animals are carefully observed | Oct-15 | ||
| moderate to severe burden on animals, moderate to severe sickness, | 16-20 | ||
| animals are carefully observed, abort of experiment if necessary, Isolation, lethargy, coordination disorders | |||
| severe burden on animals, Strongly accelerated breathing+50% | >20 | ||
| Clinical observation | Normal | Moderate | Severe |
| PbAnka Infection | - | - | >20 |
| Pb Anka infection + MSCs infusion | 3 | - | - |
Table 1: Disease severity assessment in cerebral malaria infection: Clinical score.
Figure 1: MSC infusion prolongs survival, reduce parasitaemia and regulates hemozoin accumulation in PbANKA infected mice. Female C57BL/6 mice were infected with 5 × 105 pRBCs. (A) Growth of parasitaemia and development of clinical symptoms were monitored for 40 days post-infection; (B,C) Giemsa staining of thin blood smears at different time points showed significant difference in the percentage of parasite in infected mice infused with MSCs as compared to the infected control;(D) Survival of mice following parasite infection were observed in both the groups of animals over the period of 40 days. All the mice with PbAnka infection died within 8-10 days whereas MSC infusion rendered absolute survival. (E) PbANKA results in hemozoin accumulation in the spleen and other secondary organs. Colorimetric assay reveals significant reduction in the accumulation of hemozoin pigments in spleen cells suspension of MSCs infused animals compared with PbANKA infected mice; (F) Hemozoin content have shown statistically significant in bar graph.
MSCs infusion restores morphology and reduces cytotoxic infiltration of Hemozoin in the Spleen of infected animals
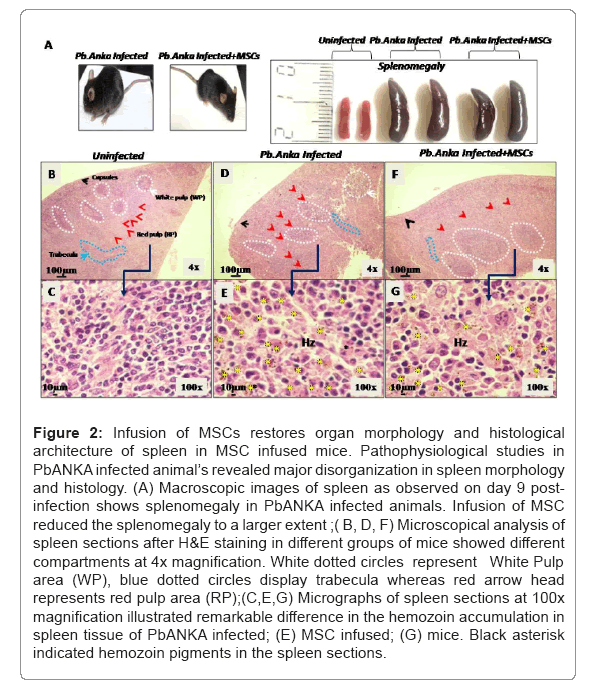
Spleen is the major secondary lymphoid organs where immune cells and RBCs get accumulated due to infection. Splenomegaly is the most evident changes in the disease progression that occur due to influx of damaged erythrocytes and lymphocytes. Malaria parasite uses RBCs for their growth and excretes in form of cytotoxic haem contents in the spleen. However, parasite distribution and parasite load are heterogeneous in the spleen. Disorganization of spleen compartments manifest disease severity. For this purpose, we have analyzed compartments morphology and their organization in the spleen sections. At day 9th, mice were sacrificed for morphological and histological analysis. It was observed that the size of spleen was noticeably enlarged in comparison to the uninfected control. Infusion of MSCs in infected animals resulted in suppression of malaria induced splenomegaly to a larger extent (Figure 2A). For histological analysis, spleen sections were stained with H&E stain and slides were analyzed on different magnifications. We noticed the accumulation of large number of brown hemozoin pigments around red pulp where infected RBCs get filtered and immune cells were found in the white pulp in infected mice (Figures 2B and 2C) compared with uninfected mice (Figures 2D and 2E). We further found that there was disorganization of splenic compartment with the infection. White pulp atrophies, secondary lymphoid follicles and marginal zones are dimorph in PbANKA infected animals and boundaries between white and red pulp are found blurred(Figures 2D and 2E).Conversely, there was significant reduction in the hemozoin granules as well as restoration of histological architecture in MSCs infused animals’ day post infection (Figures 2F and 2G) (Figure 2).
Figure 2: Infusion of MSCs restores organ morphology and histological architecture of spleen in MSC infused mice. Pathophysiological studies in PbANKA infected animal’s revealed major disorganization in spleen morphology and histology. (A) Macroscopic images of spleen as observed on day 9 post- infection shows splenomegaly in PbANKA infected animals. Infusion of MSC reduced the splenomegaly to a larger extent ;( B, D, F) Microscopical analysis of spleen sections after H&E staining in different groups of mice showed different compartments at 4x magnification. White dotted circles represent White Pulp area (WP), blue dotted circles display trabecula whereas red arrow head represents red pulp area (RP);(C,E,G) Micrographs of spleen sections at 100x magnification illustrated remarkable difference in the hemozoin accumulation in spleen tissue of PbANKA infected; (E) MSC infused; (G) mice. Black asterisk indicated hemozoin pigments in the spleen sections.
MSC infusion attenuates neuro-degeneration and hemorrhage in PbANKA infected mice
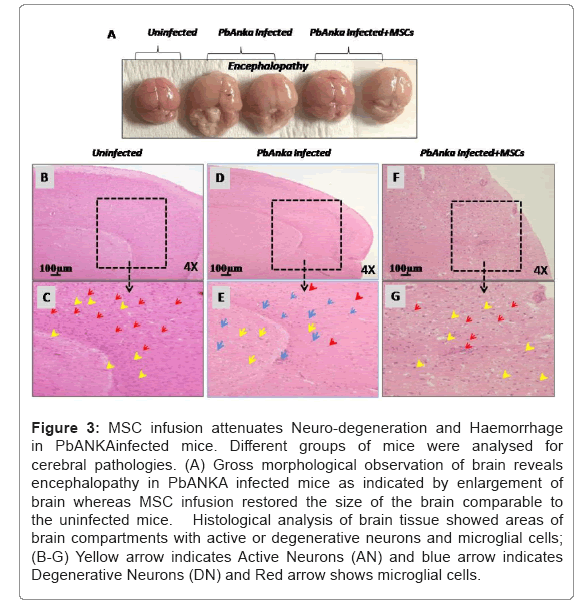
To get an insight into the cerebral pathology, all PbANKA infected animals were sacrificed for histological and cellular analysis post-infection. As reported, brain integrity was disrupted following cerebral infection accompanied by inflammation and oedema. Immune cells and infected red blood cells infiltrated into blood vessels and interrupted the blood flow, resulting in oedema and neuropathological consequences. To analyze the congestion of infected cells into blood capillaries and blood flow, we used Evans blue staining to demonstrate the blood circulation. Following the appearance of neurological symptoms, intact brain was taken out from both groups of animals for morphological evaluation. Macroscopic analysis has shown the irregular distribution of Evans blue stain in PbANKA infected animals compared with MSCs infused animals (Data not shown). PbANKA infected control mice also developed symptoms of encephalopathy concurrent to parasite sequestration in brain tissue whereas it has been observed that MSC infusion restored the morphological architecture to a larger extent (Figure 3A). Furthermore, experimentally it has been observed that the MSCs infused animals were resistant against cerebral impairment due to cerebral malaria. Our results highlight the increased number of microglial cells in MSCs infused infected animals as compared to the infected control (Figures 3B-3G). Microglial cells are the part of immune cells in the central nervous system and first to respond whenever there is any infection. These cells as reported to encounter the infected cells to maintain the brain integrity and cellular homeostasis in the brain. MSCs supports microglial cells to reduce brain pathology. Microscopical analysis at higher magnification reveals the areas of degenerative neurons in PbANKA infected animals. There was substantial reduction in degenerative neuron cells in MSCs infused animals eventually increasing the number of active neurons (Figures 3G and 3H) (Figure 3).
Figure 3: MSC infusion attenuates Neuro-degeneration and Haemorrhage in PbANKAinfected mice. Different groups of mice were analysed for cerebral pathologies. (A) Gross morphological observation of brain reveals encephalopathy in PbANKA infected mice as indicated by enlargement of brain whereas MSC infusion restored the size of the brain comparable to the uninfected mice. Histological analysis of brain tissue showed areas of brain compartments with active or degenerative neurons and microglial cells; (B-G) Yellow arrow indicates Active Neurons (AN) and blue arrow indicates Degenerative Neurons (DN) and Red arrow shows microglial cells.
Alteration of liver pathology in MSCs infused animals
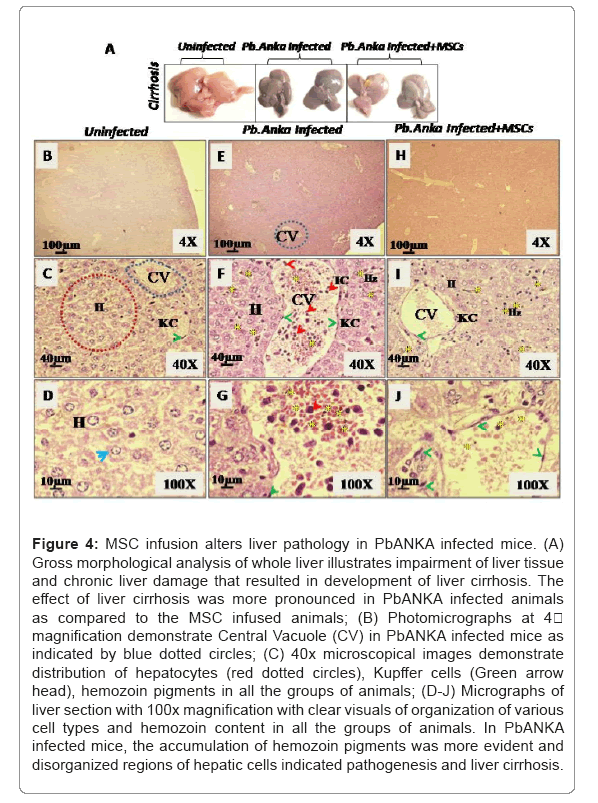
Evaluation of gross morphological structure of intact liver indicates liver dysfunction and development of cirrhosis in PbANKA infected mice (Figure 4A). Morphologically, hepatocytes and Endothelial Cells (ECs) in the liver were found affected in PbANKA infection. On the other hand, MSC infusion significantly restored the morphological architecture of the liver comparable to uninfected one (Figure 4A). H&E staining revealed hexagonal lobules and acini in normal histological analysis. Liver sections were used from PbANKA infected and MSCs infused animals for histological analysis and evaluation of liver cirrhosis (Figures 4B-4D). Detailed histological analysis revealed histopathological changes in the liver during severe PbANKA infection. Liver cirrhosis were characterized by vascularized fibrotic septa, congestion in
Sinusoids, presence of abnormal nodules inflammation in the portal tract and disorganised architecture of liver in PbANKA infected animals (Figures 4E-4G). Central veins exhibit significant increase in the accumulation of pRBCs (Figures 4F and 4G). In contrast, MSCs treated mice reveals the significant restoration of normal architecture of the liver with partially normal portal tract, hepatic artery as well as considerably less inflammatory cells (Figures 4H-4J).We also observed significant reduction in fatty deposition in infused mice. Moreover, the accumulation of hemozoin pigments were predominantly higher in PbANKA infected animals (Figures 4F and 4G) compared to MSCs treated mice (Figures 4I and 4J) and uninfected mice (Figures 4B-4D) (Figure 4).
Figure 4: MSC infusion alters liver pathology in PbANKA infected mice. (A) Gross morphological analysis of whole liver illustrates impairment of liver tissue and chronic liver damage that resulted in development of liver cirrhosis. The effect of liver cirrhosis was more pronounced in PbANKA infected animals as compared to the MSC infused animals; (B) Photomicrographs at 4 magnification demonstrate Central Vacuole (CV) in PbANKA infected mice as indicated by blue dotted circles; (C) 40x microscopical images demonstrate distribution of hepatocytes (red dotted circles), Kupffer cells (Green arrow head), hemozoin pigments in all the groups of animals; (D-J) Micrographs of liver section with 100x magnification with clear visuals of organization of various cell types and hemozoin content in all the groups of animals. In PbANKA infected mice, the accumulation of hemozoin pigments was more evident and disorganized regions of hepatic cells indicated pathogenesis and liver cirrhosis.
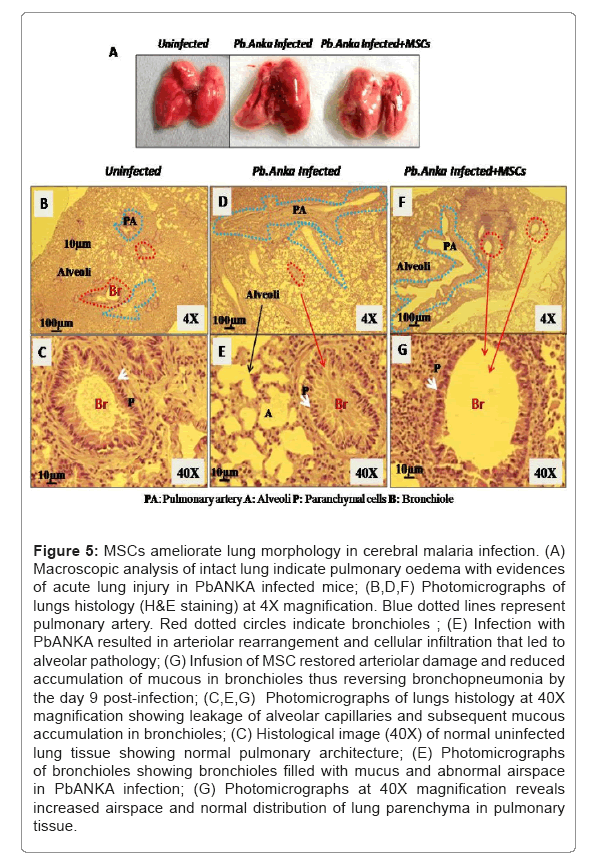
MSCs infusion ameliorate lung morphology in cerebral malaria infection
Malaria infection exhibited manifestation of cellular pathology and organ dysfunction as diseases progress. Gross morphological analysis of lungs of PbANKA infected animals revealed signs of lung injury and parasite sequestration resulting in oedema. MSCs infusion successfully restored the tissue inflammation induced as a result of PbANKA infection (Figure 5A). In lung histology, PbANKA infected animals have shown that the leakage of alveolar septa leading to the increased alveolar capillary permeability and loss of intravascular fluid into the lungs compared to MSCs infused animals (Figures 5B-5G). Further, we have observed bronchiolar morphology in PbANKA infected animals when cerebral pathology occurred. In contrast to the MSC infused mice, the bronchioles of PbANKA infected mice were filled with excess of mucus causing bronchopneumonia. The abnormal and enlarged airspace in lung tissue of PbANKA infected mice resulted in diffused emphysema as compared to the MSC infused mice (Figure 5).
Figure 5: MSCs ameliorate lung morphology in cerebral malaria infection. (A) Macroscopic analysis of intact lung indicate pulmonary oedema with evidences of acute lung injury in PbANKA infected mice; (B,D,F) Photomicrographs of lungs histology (H&E staining) at 4X magnification. Blue dotted lines represent pulmonary artery. Red dotted circles indicate bronchioles ; (E) Infection with PbANKA resulted in arteriolar rearrangement and cellular infiltration that led to alveolar pathology; (G) Infusion of MSC restored arteriolar damage and reduced accumulation of mucous in bronchioles thus reversing bronchopneumonia by the day 9 post-infection; (C,E,G) Photomicrographs of lungs histology at 40X magnification showing leakage of alveolar capillaries and subsequent mucous accumulation in bronchioles; (C) Histological image (40X) of normal uninfected lung tissue showing normal pulmonary architecture; (E) Photomicrographs of bronchioles showing bronchioles filled with mucus and abnormal airspace in PbANKA infection; (G) Photomicrographs at 40X magnification reveals increased airspace and normal distribution of lung parenchyma in pulmonary tissue.
Discussion
Pathogenesis of severe malaria accompanies cerebral and multi-organ impairment due to
dysregulated excessive inflammatory immune response. The plasticity and immunomodulatory properties of MSCs have encouraged the tremendous advancements in their experimental and clinical applications such as those of autoimmune diseases and chronic inflammatory diseases [18,19]. Multipotent mesenchymal stem cells displayed excellent efficacy by enhancing host immune responses and increasing haematopoietic recovery [20]. Our recent studies have reported the accumulation of unique subsets MSCs in the secondary lymphoid organs in response to malaria pathogenesis. These induced MSCs have the potential to activate co-stimulatory molecules and regulate the expression of negative co- stimulatory molecules on T-lymphocytes thus modulating the immune response against parasite [21]. Interestingly, these MSCs show immunomodulatory plasticity that is greatly influenced by their microenvironment. Our previous work witnessed the MSCs induced restoration of the functions of CD34+ haematopoietic cells and CD4+ and CD8+ T cells during malaria infection. Besides, we also observed that MSCs render protection against malaria disease by reprogramming erythropoiesis as a consequence of the prolifertaion of erythropoietic colonies, Colony- Forming-Units-Erythroid (CFU-E) in the bone marrow [20].
In the present investigation, the foremost insight obtained is that the infusion of induced MSCs in cerebral malaria-infected mice showed prolonged survival and reduced parasitemia. Here, we observed a remarkable decline in parasitemia levels during the first 8 days of infection with PbANKA infected mice treated with MSCs compared to the infected control. In accordance with the notable difference in parasitemia, the mice showed enhanced survival with MSCs infusion. Presumably, these novel iMSCs exhibit the potential of regulating parasite growth that eventually confers protection against fatal cerebral malaria illness. Another remarkable difference was observed in phenotypic alterations of infected control and infected animals infused with MSCs. The impact of MSCs in restoring the phenotypic alterations was studied in organs such as the brain, liver, spleen and lungs. In cerebral malaria pathology, the gross morphology of the vital peripheral organs is impaired due to parasite sequestration and leukocyte infiltration resulting in organ damage and dysfunction. Oedema in the peripheral organs is the most prominent cytopathological shreds of evidence of inflammation in fatal murine malaria [22]. The present investigation demonstrates the role of MSCs in restoring the morphological alterations in various organs during cerebral malaria pathology. Here, we observed that MSC treatment in PbANKA infected mice sustained minor organs impairment and pronounced improvement in the morphological architecture and functions of the peripheral organs. This morphological evidence indicates that MSC administration attenuates tissue inflammation and stimulates organs to repair in ECM. Moreover, the restoration of the gross morphological architecture of vital organs in MSC treated mice is an indicative parasite clearance and reduced infiltration of immune cells such as leukocytes that rendered pronounced improvement in the survival of the mice. Our results highlight the significance of MSCs in reducing the risk of developing severe cerebral malaria pathology. There is a critical concurrence between the disruption of blood- brain barrier integrity and cerebral malaria pathology. The migration and accumulation of iRBCs and the immune cells to the inflamed brain are the significant contributors of brain dysfunction [7]. Nevertheless, our results further confirm the reduced infiltration of iRBCs in the brain of PbANKA infectedanimals infused with MSCs. In the present investigation, it was observed that there were few evident cerebral lesions, and oedema in MSC treated PbANKA infected mice. Histopathological examination of the peripheral organs shows the accumulation of malarial pigment, hemozoin formed because of digestion of heamoglobin by the plasmodium parasite. The accumulation of hemozoin triggers local inflammation that further contributes to oedema [23,24]. Our observations strongly suggest the significant role of MSCs in diminishing the deposition of hemozoin in PbANKA infected animals’ peripheral organs, subsequently bringing down the local inflammation in the organs. Histological analysis reveals the microvascular lesions and hemorrhage resulting from rupture of vessels wall and endothelial degeneration in the organs of infected mice. Infiltration and adherence of infected RBCs in the perivascular membrane results in the enlargement of the perivascular spaces in the infected mice [25]. Consistent with our results, the histological analysis further reveals the protective nature of MSCs as indicated by diminished production of hemozoin, microvascular lesions, and tissue injury after MSC infusion in infected mice. Taken together, our findings demonstrate the significance of MSCs in reducing tissue inflammation, restoration of organs morphology and histoarchitectural damage that ultimately prolongs the survival in experimental cerebral malaria (Figure 6).
Conclusion
Critical understanding of the fate of MSCs following their infusion into the host enabled us to determine the biological properties and efficacies of MSCs in cerebral malaria pathologies. During the constant search of new anti-malarials, this study has provided new opportunities to extend the work better to understand the immunomodulatory aspects of cerebral malaria pathogenesis. By optimizing the strategies to improve the control of cerebral encephalopathy and complexities of cerebral malaria, the intervene may advance towards prognosis and clinical outcome.
Acknowledgement
The research was supported by ICMR-NIMR intramural grant and thankful to Mr. Naipal Singh, Ms. Manpreet Saini and Mr. Sanjay Shahi, all technical staffs who assist during experimental procedures.
References
- Dondorp AM, Lee SJ, Faiz MA, Mishra S, Price R, et al. (2008) The relationship between age and the manifestations of and mortality associated with severe malaria. Clin Infect Dis 47(2):151-157.
- Perkins DJ, Were T, Davenport GC, Kempaiah P, Hittner JB, et al. (2011) Severe malarial anemia: Innate immunity and pathogenesis. Int J Biol Sci 7(9):1427.
- Ghazanfari N, Mueller SN, Heath WR (2018) Cerebral malaria in mouse and man. Front Immunol 9:2016.
- Hora R, Kapoor P, Thind KK, Mishra PC (2016) Cerebral malaria-clinical manifestations and pathogenesis. Metabo Brain Dis 31(2):225-237.
- Hunt NH, Golenser J, Chan-Ling T, Parekh S, Rae C, et al. (2006) Immunopathogenesis of cerebral malaria. Int J Parasitol 36(5):569-582.
- Idro R, Marsh K, John CC, Newton CR (2010) Cerebral malaria: Mechanisms of brain injury and strategies for improved neurocognitive outcome. Pediatr Res 68(4):267-274.
- Nishanth G, Schluter D (2019) Blood-Brain Barrier in cerebral malaria: Pathogenesis and therapeutic intervention. Trends parasitol35 7):516-528.
- Storm J, Craig AG (2014) Pathogenesis of cerebral malaria-inflammation and cytoadherence. Front Cel Infect Microbiol 4:100.
- Mandala WL, Msefula CL, Gondwe EN, Drayson MT, Molyneux ME (2017) Cytokine profiles in malawian children presenting with uncomplicated malaria, severe malarial anemia, and cerebral malaria. Clin Vaccine Immunol 24(4):e00533-16.
- Thuma PE, VanDijk J, Bucala R, Debebe Z, Nekhai S, et al. (2011) Distinct clinical and immunologic profiles in severe malarial anemia and cerebral malaria in Zambia. J Infect Dis 203(2):211-219.
- Safeukui I, Gomez ND, Adelani AA, Burte F, Afolabi NK, et al. (2015) Malaria induces anemia through CD8+T cell-dependent parasite clearance and erythrocyte removal in the spleen. MBio 6(1):e02493-14.
- Haldar K, Mohandas N (2009) Malaria, erythrocytic infection, and anemia. Hematology Am Soc Hematol Educ Program 2009(1):87-93.
- Keswani T, Sarkar S, Sengupta A, Bhattacharyya A (2016) Role of TGF-β and IL-6 in dendritic cells, Treg and Th17 mediated immune response during experimental cerebral malaria. Cytokine 88:154-166.
- Scholzen A, Sauerwein RW (2013) How malaria modulates memory: Activation and dysregulation of B cells in Plasmodium infection. Trends Parasitol 29(5):252-262.
- Stanisic DI, Barry AE, Good MF (2013) Escaping the immune system: How the malaria parasite makes vaccine development a challenge. Trends Parasitol 29(12):612-622.
- Belyaev NN, Brown DE, Diaz AIG, Rae A, Jarra W, et al. (2010) Induction of an IL7-R+ c-Kithi myelolymphoid progenitor critically dependent on IFN-γ signaling during acute malaria. Nature Immunol 11(6):477-485.
- Pisciotta JM, Scholl PF, Shuman JL, Shualev V, Sullivan DJ (2017) Quantitative characterization of hemozoin in Plasmodium berghei and vivax. Int J Parasitol Drugs Drug Resist 7(1):110-119.
- Herbas MS, Okazaki M, Terao E, Xuan X, Arai H, et al. (2010) α-Tocopherol transfer protein inhibition is effective in the prevention of cerebral malaria in mice. The Am J clin nutr 91(1):200-207.
- Wang Y, Chen X, Cao W, Shi Y (2014) Plasticity of mesenchymal stem cells in immunomodulation: Pathological and therapeutic implications. Nature Immunol 15(11):1009-1016.
- Thakur RS, Awasthi V, Sanyal A, Chatterjee S, Rani S, et al. (2020) Mesenchymal stem cells protect against malaria pathogenesis by reprogramming erythropoiesis in the bone marrow. Cell Death Dis 6(1):1-10.
- Thakur RS, Tousif S, Awasthi V, Sanyal A, Atul PK, et al. (2013) Mesenchymal stem cells play an important role in host protective immune responses against malaria by modulating regulatory T cells. Eur J Immunol 43(8):2070-2077.
- Autino B, Corbett Y, Castelli F, Taramelli, D (2012) Pathogenesis of malaria in tissues and blood. Mediterr J Hematol Infect Dis 4(1).
- Chauhan R, Awasthi V, Thakur RS, Pande V, Chattopadhyay D, et al. (2022) CD4+ ICOS+ Foxp3+: A sub-population of regulatory T cells contribute to malaria pathogenesis. Malar J 21(1):1-10.
- Pham TT, Lamb TJ, Deroost K, Opdenakker G, van den Steen PE (2021) Hemozoin in malarial complications: More questions than answers. Trends Parasitol 37(3):226-239.
- Pais TF, Penha-Gonçalves C (2019) Brain endothelium: The “innate immunity response hypothesis” in cerebral malaria pathogenesis. Front Immunol 9:3100.
Citation: Thakur RS, Tiwari M, Chauhan R, Kalkal M, Chaudhary A, et al. (2022) Mesenchymal Stem Cells Reverse the Pathophysiology of Cerebral Malaria Induced by Plasmodium berghei ANKA. J Clin Exp Pathol 12: 421.
Copyright: © 2022 Thakur RS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3019
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2636
- PDF downloads: 383