Case Report Open Access
Menetrier Disease in a Five Year Old Girl - A Case Report and Review of Literature
Virtut Velmishi1*, Besnik Elezi2and Gentiana Cekodhima3
1Service of Pediatric nr 2, “Mother Teresa Hospital”-Tirana, Albania
2Service of Gastroenterology, Regional hospital of Gjilan –Kosovo, Albania
3Service of Histopathology, “Mother Teresa Hospital”-Tirana, Albania
- Corresponding Author:
- Virtut Velmishi
Service of Pediatric nr 2; “Mother Teresa Hospital”-Tirana, Albania
Tel: 00355672057335
E-mail: tutimodh@yahoo. com
Received Date: January 23, 2016 Accepted Date: February 29, 2016 Published Date: March 04, 2016
Citation:Velmishi V, Elezi B, Cekodhima G (2016) Menetrier Disease in a Five Year Old Girl - A Case Report and Review of Literature. J Gastrointest Dig Syst 6:395. doi:10.4172/2161-069X.1000395
Copyright: © 2016 Velmishi V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Introduction: Menetrier`s disease is one of the rarest protein losing gastropathies in childhood characterized by hypertrophy of gastric folds. Children with Menetrier disease tend to follow a self-limited course with symptoms typically completely resolving within 2 to 10 weeks.
Case report: A five year old girl presented fever for two days, abdominal pain and vomiting. After two other days she presented periorbital swelling and skin rash. Laboratory findings on admission showed hypoalbuminemia and eosinophilia. Screening for Helicobacter pylori and cytomegalovirus resulted negative. Abdominal ultrasonography showed moderate ascitis and in chest X ray revealed effusion in both lungs. Gastroscopy showed severe erosions in fundus and in upper part of stomach body. The lower part of stomach and antrum was normal. Histopathology showed data compatible with Menetrier disease. She was treated with several albumin infusions and diuretics and her symptoms improved after 4 weeks of treatment.
Conclusion: This is the first case of pediatric MD in our experience. Endoscopic images and histological data are very important to support
Keywords
Menetrier disease; Cytomegalovirus; Hypertophic folds; Hypoalbuminemia
Introduction
Menetrier disease (MD), consisting of hypertophic gastric folds complicated by extravasation of serum proteins and consequent hypoproteinemia secondary to a protein- losing gastropathy , is an unusual condition, first described by french physician Menetrier in 1888 [1]. In recent years, cases with similar clinical presentation and pathological features have been reported in children [2]. The etiology of this disorder remains unclear, although several exogenous agents as chemical irritans and toxins are known to cause gastric mucosal hyperplasia. The pathogenesis of pediatric Menetrier disease has been associated with viral infections, autoimmune disease and allergic process. Cytomegaloirus infection is accused in many of these pediatric cases in the past few decades [3]. The disorder is associated with excessive secretion of transforming growth factor alpha (TGF –α) [4]. Symptoms and pathological features of Menetrier disease in children are similar to those in adults, but disease in children is usually self-limited and often follows respiratory infection [5].
Case Presentation
A five - year - old girl was admitted in our service for recurrent vomiting and abdominal pain. She was the first child of an albanian couple born from a normal pregnancy. Birth weight was 3600 g. She was breast fed and was vaccinated according to Albanian schedule. Her parents deny any other disease except thalassemia trait. Four days before hospitalisation she presented fever 39°C which is normalized after two days. The next day she presented vomiting and abdominal pain. She was rehidrated by intravenous fluids in emergency department. She was discharged but the next day she presented again vomiting. Emergency physician started IV rehidration and Ceftriaxone IV in the context of urinary infection (white blood cells in the urine over the normal range). After therapy she presented periorbital edema and for this reason she was hospitalised. On admission she was afebrile but pale and tired. Oral mucosa was hiperemic, neck was clear and rib cage symmetrical. In her face was visualisated a skin rash. Heart rate had normal rhythm 100/min; lung auscultation showed a weaknees of respiration sounds in both lung bases. Abdomen was soft and palpable. Liver was large 2 cm and spleen is normal under the costal margin. Weight=20 kg; Blood Pressure=90/50 mm/hg; SAT O2>93%.
Laboratory tests showed: WBC=14000/mm3; RBC=6500000/mm3; HgB-11.9 g/dl; HCT-39.6%; MCV-61 fL; MCH-18.1 pg; MCHC-29.3 g/dl; PLT=367000/mm3; lym=36%; mon=7%; neut=43.7%; eos=11.8%; Bas=1.2%.
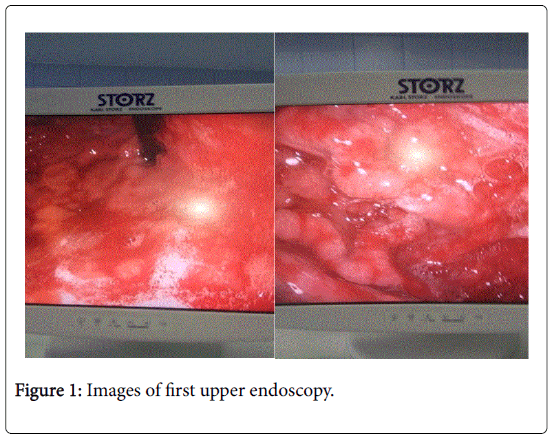
Biochemical examinations showed a normal PCR. Level of glucose in blood and electrolytes was normal. Liver and kidney function was uneventful. We noted a total protein 3, 7 g/dl and albuminemia was 2 g/dl. Lipidogram was also normal. ANCA, ANA, Fibrinogen, C3, C4, rheumatoid factor and ASO were all in normal range. Blood gas showed PH=7. 36; HCO3=21. 1; PO2=67 mm/hg; pCO2=34. Heart sonography was normal. Chest X ray showed pleural effusion in both base of lungs. Several urine analyses didn`t show proteinuria or hematuria despite a persistent ketonuria. Ultrasonography of thorax and abdomen showed mild pleural efusion in both bases of lungs. Minimal subhepatic liquide was visualized in abdomen. Throat culture was normal. A protein electrophoresis was also normal. Stool analyses for parasite, viruses and H. pylori antigen resulted negative. Stool for occult blood was positive. IgM CMV=0.647 (negative) IgG CMV=42.34 (positive). Serology for Mycoplasma resulted negative. Stool Alfa 1 antitripsine was performed in Italy and resulted positive confirming digestive losing of proteins. Initially we suspected interstitial nephritis because she has shown a skin rash and periphery eosinophilia. But we decided to perform also an upper digestive endoscopy which revealed a hyperemic mucosa, thickened folds with lots of erosions without active hemorrhage (Figure 1). We obtained biopsies in stomach, esophagus and duodenum.
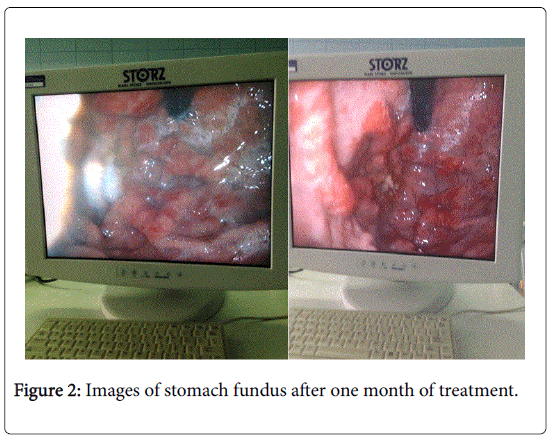
Our patient was treated initially with frequent albumin infusions (every two or three days) for three weeks. She was treated also with lasix and esomeprasole (1 mg/kg/day). We have started a high protein diet. She continues to have abdominal pain and vomiting but all symptoms are resolved within a month. A month later the last laboratory data showed a normal level of albumin in blood and the control of upper endoscopy showed an important amelioration (Figure 2).
Discussion
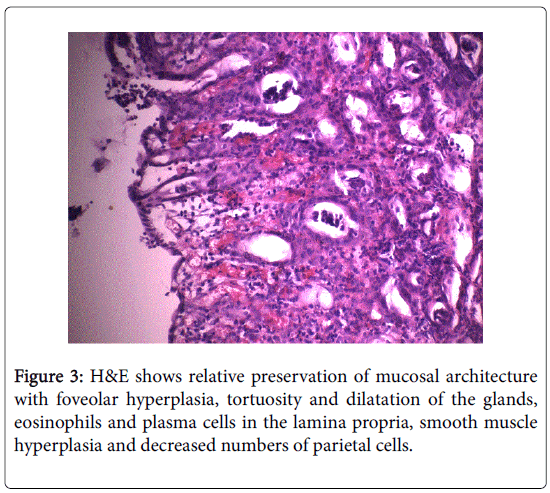
Pediatric Menetrier disease is a rare entity that can lead in misdiagnosis. We have emphasised some points where the diagnostic is clear and some others where are controversies. Clinical symptoms like abdominal pain, vomiting, periorbital swelling and olyguria make us to think about a renal disorder. Consultation by our nephrologist highlights some other clinical signs such as face rash and laboratory data as peripheric eosinophilia and hypoalbuminemia casting the doubt about intersticial nephritis. But in several urine analyses we didn`t find albumin or red blood cells in urine, only some white blood cells and persistence of ketonuria Upper digestive endoscopy remains the corner stone of diagnostic because endoscopic image was characteristic. We have seen thickened folds and erosions in fundus, cardia and the upper part of stomach while antrum and duodenum were normal. Taking into account hypoalbuminemia and this typical image we thought about protein loosing enteropathy (gastropathy in our case) and Menetrier disease was one of the first causes. Other causes of protein-loosing enteropathy include celiac disease, gastric lymphoma, eosinophilic gastroenteritis, hypertrophic gastropahty associated with H pylori infection and Crohn`s disease [6-9]. Eosinophilic gastroenteritis may involve gastric antrum and small intestine but there is often family history of allergic disease. Gastric lymphoma is very rare in children and not related with edema and hypoproteinemia. Crohn disease and Peutz- Jeghers syndrome have different signs and symptoms. Very rare diseases which have similar radiological signs with MD include Zollinger-Ellisosn syndrome, hypertrophic secretory gastritis, gastric varices and lymphangiectasia. Histological examination is the best method to differentiate all suspected cases Histopathology of Menetrier disease is also characteristic with hyperthrophy of gastric glands, cystic dilatation of glands deep in the mucosa, inflammatory cells infiltration, and thickened hyperplastic mucosa. In our case you may see foveolar hyperplasia, tortuosity and dilatation of the glands, eosinophils and plasma cells in the lamina propria, smooth muscle hyperplasia and decreased numbers of parietal cells (Figure 3).
The hard part of our case was the etiological cause. A definitive cause of MD is widely debated [8,10]. There are a lot of etiological factors in this debate such as chemical irritants, toxins, dietary factors, allergy, immunologic and autoimmune disorders. The most important etiological factor found in children was CMV infection. One study reported that CMV infection was associated in 19 of 27 children with MD2. Another review of children with MD found an association with CMV infection in 25 of 56 cases. Gastric biopsy showed characteristic CMV inclusion bodies in 16 of those 10. In our case neither serology nor histology didn’t show signs of CMV infection. H pylori were accused also as a potential etiological factor but H pylori infection is more prevalent in MD in adults than children [11-13]. We have excluded H pylori infection in our case by histological data, urease rapid test and negative stool test for H pylori antigen. We have excluded also some other etiological factors such as mycoplasma, herpes virus, ebstein barr virus, adenovirus and giardia lamblia [14,15]. Recent studies indicate that PCR may be sensitive for early diagnosis of active CMV infection in immumocompetent patients [1,16]. The direct detection of CMV in nucleic acids by in situ hybridization or of viral antigens by immunocytochemistry using monoclonal antibodies is more sensitive and specific, and is as sensitive as viral culture [17]. We had not possibility to perform protein chain reaction for CMV in our patient.
Pediatric MD typically follows a benign and self-limited course, with recovery time ranging from weeks to month. Our patients were treated initially with frequent albumin infusions (every two or three days) for three weeks. She was treated also with lasix and esomeprasole (1 mg/kg/day). She continue to have abdominal pain and vomiting but all symptoms are resolved within a month
Conclusion
This is the first case of pediatric MD in our experience. Endoscopic images and histological data are very important to support clinical and laboratory findings for an accurate diagnosis. In our case the etiological factor of Menetrier disease remains unclear and disputable.
References
- Menetrier P (1888) Des polyadenomesgastriques et de leur rapports avec le cancer de l`estomac. Arch Physiol Norm Pathol (Paris) 32: 236-262.
- Occena RO, Taylor SF, Robinson CC, Sokol RJ (1993) Association of cytomegalovirus with Ménétrier's disease in childhood: report of two new cases with a review of literature.J PediatrGastroenterolNutr 17: 217-224.
- Xiao SY, Hart J (2001) Marked gastric foveolar hyperplasia associated with active cytomegalovirus infection.Am J Gastroenterol 96: 223-226.
- Coffey RJ, Washington MK, Corless CL, Heinrich MC (2007) Ménétrier disease and gastrointestinal stromal tumors: hyperproliferative disorders of the stomach.J Clin Invest 117: 70-80.
- Robbins C (2014) Pathological Basis of Disease 8e:782.
- Blackstone MM, Mittal MK (2008) The edematous toddler: a case of pediatric Ménétrier disease.PediatrEmerg Care 24: 682-684.
- Cieslak TJ, Mullett CT, Puntel RA, Latimer JS (1993) Menetrier's disease associated with cytomegalovirus infection in children: report of two cases and review of the literature.Pediatr Infect Dis J 12: 340-343.
- Gandhi M, Nagashree S, Murthy V, Hegde R, Viswanath D (2001) Menetrier's disease.Indian J Pediatr 68: 685-686.
- Rai F, Votava A, Tambi L, Manojlovi S (1988) Hypertrophic gastritis in association with sepsis and death in a two-month-old infant.J PediatrGastroenterolNutr 7: 461-465.
- Canan O,Ozcay F, Bilezikci B (2008) “Menetrier `s disease and severe gastric ulcers associated with cytomegalovirus infection in an immunocompetent child: A case report “ Turkish Journal of Pediatrics” 50: 291-295.
- Konstantinidou AE, Morphopoulos G, Korkolopoulou P, Eftychiadis C, Stamokosta E, et al. (2004) Menetrier disease of early infancy: a separate entity?J PediatrGastroenterolNutr 39: 177-182.
- Bayerdörffer E, Ritter MM, Hatz R, Brooks W, Ruckdeschel G, et al. (1994) Healing of protein losing hypertrophic gastropathy by eradication of Helicobacter pylori--is Helicobacter pylori a pathogenic factor in Ménétrier's disease?Gut 35: 701-704.
- Yamada M, Sumazaki R, Adachi H(1997) “Resolution of protein loosing hyperthrophicgastropathy by eradication of Helicobacter pillory. ” Europian Journal of Pediatrics 156: 182-185.
- Fenoglio-Preiser CM,Noffsinger AE,Stemmermann GN (1999) Hypertrophic hyperplastic gastropathies. In: Gastrointestinal Pathology. An Atlas and Text. 2nd edn Philadelphia:Lippincott Raven; 1999: 209-213.
- Eisenstat DD, Griffiths AM, Cutz E, Petric M, Drumm B (1995) Acute cytomegalovirus infection in a child with Ménétrier's disease.Gastroenterology 109: 592-595.
- Scharschmidt BF (1977) The natural history of hypertrophic gastrophy (Menetrier's disease). Report of a case with 16 year follow-up and review of 120 cases from the literature.Am J Med 63: 644-652.
- Hochman JA, Witte DP, Cohen MB (1996) Diagnosis of cytomegalovirus infection in pediatric Menetrier's disease by in situ hybridization.J ClinMicrobiol 34: 2588-2589.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12803
- [From(publication date):
April-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11933
- PDF downloads : 870