Case Report Open Access
Melanosis “Coli” in Anal Heterotopic Gastric Mucosa: A Case Report and Review of the Literature
Debbie R Walley*, Robert Greer, Maria F Gonzalez and Charu Subramony
Department of Pathology, University of Mississippi Medical Center, Hospital in Jackson, Mississippi, USA
- *Corresponding Author:
- Debbie R Walley
Department of Pathology
University of Mississippi Medical Center
Hospital in Jackson, Mississippi, USA
Tel: 601-410-2982
E-mail: darigney@umc.edu
Received date: September 7, 2016; Accepted date: September 24, 2016; Published date: September 29, 2016
Citation: Walley DR, Greer R, Gonzalez MF, Subramony C (2016) Melanosis “Coli” in Anal Heterotopic Gastric Mucosa: A Case Report and Review of the Literature. J Gastrointest Dig Syst 6:471. doi: 10.4172/2161-069X.1000471
Copyright: © 2016 Walley DR et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Gastric heterotopia is the presence of gastric mucosa in a foreign anatomic location. It can occur anywhere in the gastrointestinal tract and has been well documented in the esophagus. Gastric heterotopia of the anorectum is a rare occurrence.
Case Report: We present a case of an asymptomatic adult male who underwent a colonoscopy during which an anal nodule was biopsied. Microscopic examination revealed oxyntic gastric mucosa with chronic active gastritis and melanosis coli. During a subsequent colonoscopy six years later, an abnormally pigmented area of anus was biopsied. Microscopic examination revealed antral gastric mucosa with chronic active gastritis.
A literature review showed that there have been 72 reported cases of gastric heterotopia of the anorectum. Only four of those case occurred in the anus.
Conclusion: To our knowledge, this is the first report of melanosis coli associated with gastric heterotopia of the anorectum as well as a shift in gastric mucosal type on repeat biopsy. We propose the term "outlet patch" for gastric heterotopia of the anorectum.
Keywords
Heterotopic gastric mucosa; Anus; Rectum; Melanosis coli
Introduction
Heterotopic mucosa is the presence of normal tissue in a foreign anatomical site. Gastric heterotopia is the most common reported epithelial heterotopia and can be present in any part of the GI tract [1]. The most commonly reported gastric heterotopias occur in the esophagus, duodenum, and Meckel’s diverticula [2].
Gastric heterotopia of the anus is rare. Symptoms of gastric heterotopia of the anorectum range from asymptomatic to life threatening hemorrhage [1]. The most common complaint of patients with gastric heterotopia of the anorectum is bright red blood per rectum. Treatments include excision and conservative management with a proton pump inhibitor [1].
Case Report
A 58 year old male with a past medical history of iron deficiency anemia, hypertension, peripheral arterial disease, coronary artery disease, and remote history of tobacco use and alcohol abuse presented for routine colonoscopy. No complaints such as rectal bleeding were documented in the electronic medical record.
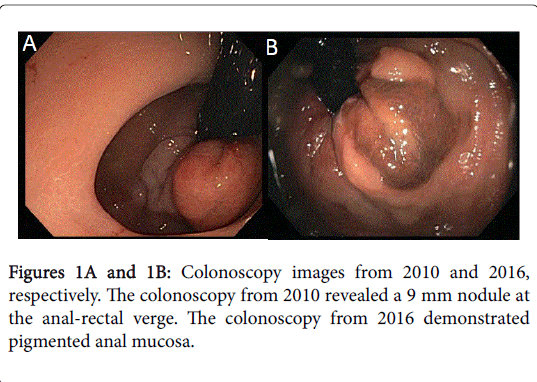
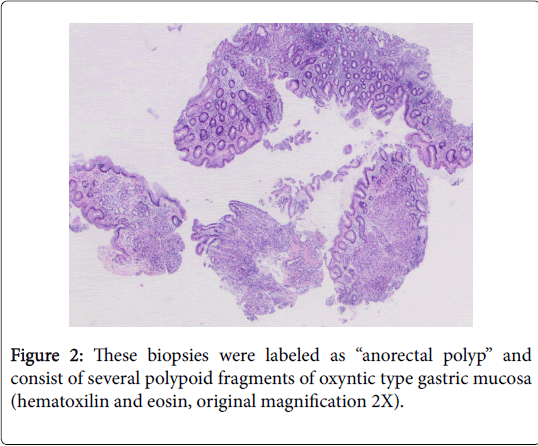
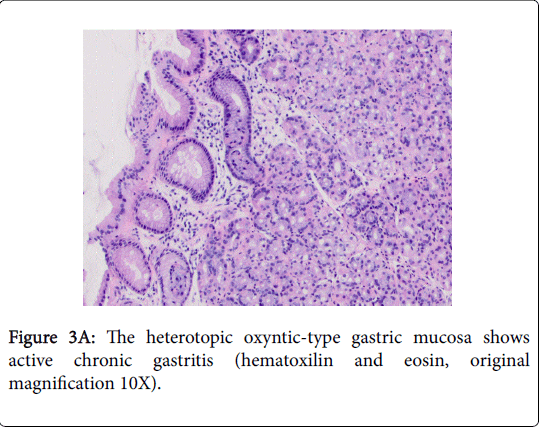
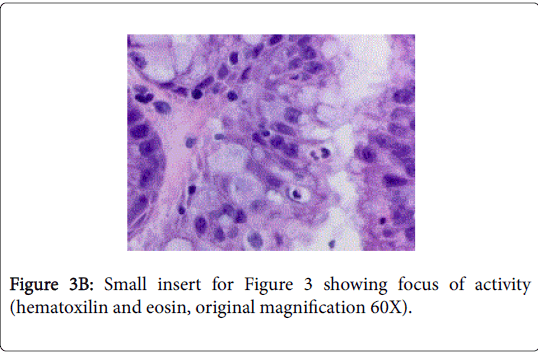
A colonoscopy six years prior was significant for three colon polyps and a 9 mm nodule at the anal-rectal verge (Figure 1A). All were biopsied. The nodule at the anal-rectal verge was found to consist of several polypoid fragments oxyntic gastric mucosa with chronic and focally active gastritis (Figure 2 and Figures 3A and 3B).
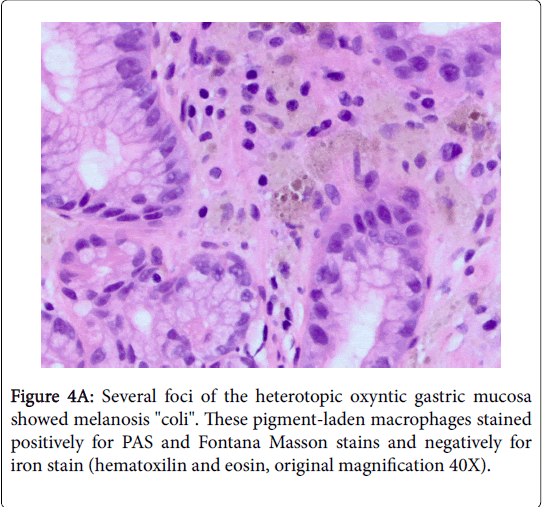
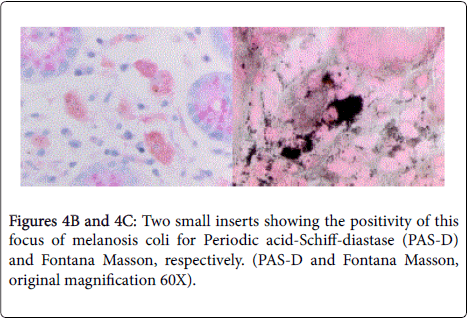
There were also several foci of melanosis “coli” within the lamina propria that stained positively for PAS-D and Fontana Masson with adequate controls (Figures 4A-4C).
An iron stain with adequate control was negative. The mucosa was negative for Helicobacter pylori
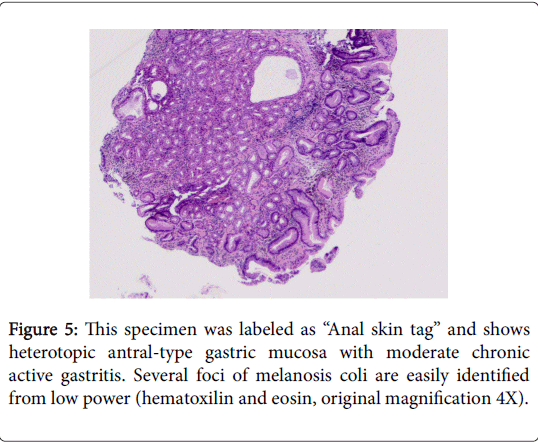
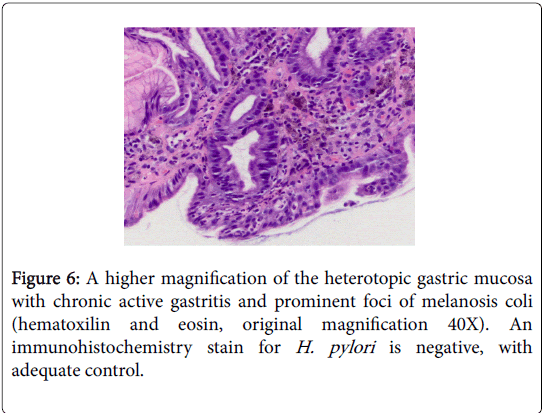
The present colonoscopy was significant for four colon polyps and pigmented anal mucosa, all of which were biopsied. The anal mucosa was found to consist of antral gastric mucosa with evidence of active chronic gastritis and melanosis “coli” (Figures 5 and 6). The mucosa was negative for Helicobacter pylori .
Discussion
Gastric heterotopia was first described in the proximal esophagus. It was described as a salmon-colored patch and termed “inlet patch.” The prevalence of inlet patch ranges from 0.1-13.8% [3]. Gastric heterotopia of the anorectum was first described in 1939 by Ewell and Jackson [4]. Since then, 72 cases of gastric heterotopia of the anorectum have been reported. Four cases occurred in the anus; 68 occurred in the rectum. Of the 72 patients, 63% were male. The median patient age was 22 years old. Thirty-four cases were reported in patients under the age of 18. [1]. Our patient is 58 years old. The development of gastric heterotopia of the anorectum is hypothesized to be the caused by differentiation error in pluripotent endoderm stem cells [5,6].
Gastric heterotopia of the anorectum can present as polyps, nodules, mucosal thickening, and ulcerations [7]. Of the reported cases, 51% of the lesions were non-polypoid while 36% were polypoid and 13% were ulcerated. Histologically, 83% of anorectal gastric heterotopias were found to have oxyntic mucosa, 11% with mixed oxyntic and antral mucosa, 5% with antral mucosa, and 2% with cardiac mucosa [1]. To our knowledge, melanosis “coli,” a pigmentation disorder of the colon wall, has not been reported in the literature [1-11]. Curiously, the patient in this case was found to have oxyntic gastric heterotopia of the anus on his initial colonoscopy while antral gastric heterotopia of the anus was found on his current colonoscopy. The initial lesion was well sampled. Eight biopsy fragments were received for microscopic examination. This change may represent shift in the metaplastic mucosa which has not been documented in previous cases reported in the literature. There have been 6 reported cases of gastric heterotopia of the rectum that were positive for Helicobacter pylori [8,9]. Although our case showed chronic active gastritis, no H. pylori bacteria were identified. There is potential for malignancy in heterotopic gastric mucosa of the anorectum. Adenocarcinoma occurring in inlet patches found in the esophagus has been reported [10]. There have been no reported cases of adenocarcinoma associated with gastric heterotopia of the anorectum [1-10].
The majority of cases of gastric heterotopia of the anorectum are symptomatic. The most common symptom is rectal bleeding associated with production of gastric acid [8,11]. Other symptoms include change in bowel habits, bloating, lower quadrant abdominal pain, and cramping. Only two cases of massive bleeding secondary to gastric heterotopia of the anorectum have been reported. Asymptomatic gastric heterotopia of the anorectum is usually reported in older patients and incidentally discovered on routine colonoscopy [1].
Treatment for gastric heterotopia of the anorectum varies. Conservative treatment includes H2 receptor antagonists, PPI, bismuth subsalicylate, and antibiotics for cases positive for Helicobacter pylori . Definitive treatment is resection. Surgical resection has fallen out of favor with the development of endoscopic resection [1,8].Conclusion
Conclusion
We report a case of gastric heterotopia of the anus, a finding that has only been reported four times in the literature. This case also has melanosis “coli,” confirmed by special stains, which has not been previously reported in heterotopic gastric mucosa. We also report a shift in gastric tissue from oxyntic to antral on repeat biopsy. Given that the number of reported cases of gastric heterotopia of the anorectum will likely continue to increase with the routine use of endoscopy for colon cancer screening, we propose the term “outlet patch” for this histological finding.
References
- Iacopini F, Gotoda T, Elisei W, Rigato P, Montagnese F, et al. (2016) Heterotopic gastric mucosa in the anus and rectum: first case report of endoscopic submucosal dissection and systematic review. Gastroenterol Rep (Oxf): 1-10.
- Odze R, Goldblum J (2009) Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas. (2nd edn.), Saunders Elsevier, Philadelphia.
- Yu L, Yang Y, Cui L, Peng L, Sun G (2013) Heterotopic gastric mucosa of the gastrointestinal tract: prevalence, histological features, and clinical characteristics. Scandinavian Scand J Gastroenterol 49: 138-144.
- Ewell G, Jackson R (1939) Aberrant gastric mucosa in the rectum with ulceration and hemorrhage. Wisconsin Medical Journal 48: 641-643.
- Sauer C, Bickston S, Borowitz S (2010) Gastric heterotopia of the rectum. J PediatrGastroenterolNutr 50: 329-333.
- Srinivasan R, Loewenstine H, Mayle J (1999) Sessile polypoid gastric heterotopia of rectum: a report of two cases and review of the literature. Archives of Pathology and Laboratory Medicine 123: 222-224.
- De Petris G and Leung S (2010) Pseudoneoplasms of the Gastrointestinal Tract. Arch Pathol Lab Med 134: 378-392.
- Swatek J, Ciechanek R, Smilo J (2015) Asymptomatic gastric heterotopia in the rectum with Helicobacter pylori infection. Pol J Pathol 66: 426-429.
- Kestemberg A, Marino G, de Lima E, Garcia FT, Carrascal E, Arredono J (1993) Gastric heterotopic mucosa in the rectum with Helicobacter pylori-like organisms: a rare cause of rectal bleeding. Int J Colorectal Dis 8: 9-12.
- Mannan A, Kahvic M, Bharadwaj S, Grover K (2008) Gastric heterotopia of the anus: report of two rare cases and review of the literature. Indian J PatholMicrobiol 51: 240-241.
- Colsa-Gutiérrez P, Kharazmi-Taghavi M, Sosa-Medina R, Berrío-Obregón J, Ingelmo-Setién, A (2016) Heterotopic gastric mucosa in the rectum: Report of a case. Cir Cir 84: 160-163.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13799
- [From(publication date):
October-2016 - Apr 11, 2025] - Breakdown by view type
- HTML page views : 12877
- PDF downloads : 922