Medication Adherence among Type 2 Diabetes Ambulatory Patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia
Received: 24-Aug-2017 / Accepted Date: 09-Sep-2017 / Published Date: 19-Sep-2017 DOI: 10.4172/2161-1165.1000322
Abstract
Background: The rapid increases in prevalence of diabetes mellitus is a great cause for concern and poor adherence to diabetic medication treatment is common problem which causes severe health complications and increased mortality. Measuring the level of adherence and associated factors on treatment is needed to evaluate the overall treatment outcome of chronic illness including diabetes. This study aimed to assess medication adherence among ambulatory patients with type 2 Diabetes mellitus in Zewditu memorial hospital in Addis Ababa, Ethiopia.
Methods: Institutional based cross sectional study was employed in Zewditu Memorial hospital. The data were collected from March-April, 2016 on 275 systematically selected patients that are already registered and have follow up. A structured questionnaire was used to interview respondents and a retrospective patient medical record review was also made. Data were analyzed using SPSS version 20 for windows software. A p-value of 0.05 or lower was considered statistically significant. Ethical clearance was obtained from Jimma university institutional review board and permission from respective heads of internal medicine department at diabetic clinic in Zewditu memorial hospital.
Results: Among 275 respondents adherence to anti-diabetic drugs was sub-optimal 141 (51.3%). The mean age for the studied population was 53.07 (SD ± 12.784) years (range from 24-87 years). And females were 59 (51.3%). Income (AOR=141, 95%CI: 0.46-1.430), lack of patients physician relationship and communication (AOR=3.432, 95% CI: 1.695-6.948), patient education (AOR=3.854, 95%CI: 2.156-6.888) and exercise (AOR=3.12, 95%CI: 1.607-6.116) were factors that had a significant association to medication non adherence.
Conclusion: Adherence to anti-diabetic drugs was sub-optimal. The patient physician relationship and communication is low. Health professionals should educate diabetic patients on the importance of medication adherence. Collaborative relationship between patient and provider may improve adherence.
Keywords: Diabetes mellitus; Chronic illness illness; Anti-diabetic drugs; Diabetic patients
Background
Globally, the prevalence of Type 2 Diabetes Mellitus (T2DM) is increasing and has become one of the major public health problems [1]. Such rapid increases in prevalence are a great cause for concern. This rise also is associated with economic development, ageing populations, increasing urbanization, dietary changes, reduced physical activity, and changes in other lifestyle patterns [2,3].
Many patients, especially patients with chronic illness, including, diabetes experience difficulties in following treatment recommendations. Even in developed countries, adherence to longterm therapy for chronic illnesses in averages only 50%. The result is due to Non adherence to their medication, that is to say patients do not receive the full benefit from their drug therapy. Partial treatment can direct to increased use of public health care services (acute care and hospitalizations), reduction in patient’s quality of life, and increased health care resources (the money that they will spend for their drug and hospital) [4].
Poor adherence to diabetes treatment is common problem which causes severe health complications and increased mortality. This is reflected for instance by an increase in the risk of cardiovascular diseases, neuropathy, retinopathy, nephropathy, and hospitalization rates; if the problem becomes sever, it can even lead to death. It has been recognized that Poor adherence, as one of the principal cause of development of complications in diabetes [5].
Adherence rates are usually reduced for patients with chronic conditions such as T2DM than those with acute conditions; this is associated with the long-term nature of chronic diseases because the decline in adherence is most rapid after the first 6 months of therapy [6]. When conditions are treated suboptimal, symptoms and complications may worsen, leading to increased use of hospital and emergency room services, office visits, and other medical resources i.e. the treatment becomes expensive [7].
So, Non-adherence to therapeutic regimens among people with diabetes is an ongoing problem and healthcare providers are constantly faced with the challenge of getting individuals to adhere to their medication regime for optimal management of their condition [8].
For diseases like diabetes, medication adherence has a significant role. Because increased level of medication adherence T2DM patients, will lead to controlled glycemic level and lowers the disease-related medical costs (hospital readmissions and emergency room visits). So this study has significant help in improving conditions that are related to non-adherence. It can also help educating the patients about the importance of proper medication use because, It’s vital that patient adherence to prescribed medications is crucial to the goal of reaching metabolic control. So the finding of this study will provide and fills the information gap related to medication adherence in T2DM patients. It can also provide base line data for policy makers and other researchers for further improvements of medication adherence for T2DM.
Methods and Materials
Study settings
The study was conducted in Zewditu Memorial Hospital (ZMH); it is located in kirkose Sub City woreda 08 Addis Ababa, Ethiopia. The hospital is named after Empress Zewditu, the cousin and predecessor of Ethiopian King Emperor Hailesilesia. Today ZMH is operated by Federal Ministry of Health under Addis Ababa health bureau. ZMH is one of the few hospitals which has diabetic clinic for diabetic patient. ZMH has three clinics visit every week for patients with T2DM and average number of patients attending the clinic in one day was known from registration book to be 40 and in one week it was 120.
Study design and period
Institutional based cross sectional study was employed by patient interview, using a questionnaire and a retrospective patient medical record reviews. The interview and medical record review was done for the same patient. Patient interviews and medical record reviews were conducted from 1st of March to April 10th of 2016 on 275 systematically selected patients that are already registered and have follow up during their appointment day.
Inclusion criteria: T2DM patients with complete medical record, who are coming to ambulatory clinic at ZMH, and with a follow up history of more than 6 month has been included.
Exclusion criteria: T2DM patients who are seriously ill, unable to communicate and patients who are not willing to participate were excluded.
Sample size and sampling procedures: The required sample size for this study is determined by using the following assumptions of 95% confidence interval usually set as 1.96, 5% was d which is the margin error, P of 0.5 is used to maximize the sample size in estimation of the prevalence rate for the population and the average number of patients attending the clinic during the study period i.e. six weeks was known from registration book to be 720 (using the 2007 E.C and 2008 E.C ZMH DM clinic registration book). Since the population is less than 10000, the formula used was single population proportion correction formula nf=Z2p(1-p)/d2(N-1)p(1-p). nf=1.962, 0.5(1-0.5)/0.05(720-1) 0.5 (1-0.5) is equals to 250 and Then 10% contingency was added on 250, it has become 275 T2DM patients 720/275=2.6≈2. Sampling Techniques was Patients who are included in the study has been selected through systematic random sampling method, that is the first participant was selected randomly then patients every other patient were selected until getting the required sample size of T2DM patients who attend the clinic based on their scheduled appointments of the hospital for at least 6 months as well as inclusion and exclusion criteria.
Data collection instrument
Interview using structured open and closed ended questionnaire (Annex 1) has been used to assess the medication adherence and practice of the diabetic patients. The questionnaire has contained Morisky Medication Adherence Scales (MMAS) to measure the adherence [9].The interview has assess back ground information including glycemic control practice, medications patients use, patientprovider relationship. The questions have focused on diabetic medication adherence among T2DM patients. Patient’s data was collected by reviewing medical charts. The data that was extracted from the medical charts include medical characteristic (fasting blood glucose levels), the type of medication used and dosage form. The patient data was collected after physician consultation with the patient.
Data collection
Data was collected by two trained nurses and one supervisor health officer that by interviewing T2DM patients in ZMH, diabetic clinic. The Investigator and supervisor has closely followed each days of the data collection process and ensure completeness and consistency of questionnaire administered. A detailed and organized questionnaire format is designed in an attempt to generate baseline information related to medication adherence and has tried to assess the condition. The questionnaire has been framed in such a way that patients could easily understand and give information that is important for the study. It is separated into five parts to get information socio-demographic factors, lifestyle related Diabetes Care Approaches, Diabetic disorder related, and Diabetic medication adherence Practice and, Morisky Medication Adherence Scales.
Data quality control
Training was given to the data collectors after that they were organized and collected the data, in order to avoid investigators bias. The questionnaire is first made in English then translated in to local language (Amharic) then translated back to English to ensure consistency. The collected quantitative data first has been rechecked for its completeness and then data was entered to EpiData and the data has been coded, and analyzed using SPSS. Pre-testing was done with 5% on Addis Ababa in Tikur anbessa referral hospital on T2DM, who were not included in the study, before the start of the main data collection.
Data processing and analysis
The Information that was obtained from interviewee with the questionnaire was analyzed using the computer statistics SPSS version 20 package. Chi square test was applied determine the associated factors that affect adherence in patients with T2DM. In all cases, a pvalue of 0.05 or lower has been considered statistically significant. A bivariate logistic regression analysis was done to see the association between the independent and dependent variables. Then, multivariate logistic regression analysis was applied by selecting only variables with P-value<0.2 in the bivariate analysis.
Ethical considerations
The ethical clearance and approval of the study protocols was granted from the Ethical Review Board of college of health science in Jimma University. In addition, the respective heads of internal medicine department at diabetic clinic in ZMH were communicated as to the objectives and benefits of the study. Each participant was informed about the objective of the study, procedures of selection and assurance of confidentiality and their names was not registered, to minimize social desirability bias and enhance anonymity. Individuals were free to withdraw from the study at any time.
Results
Socio-demographic characteristics of T2DM patients with attending the in ZMH
Out of the total 275 T2DM patients, 133 (48.4%) were females, while the rest are males. 46 (16.7%) were between 34 and 43 years of age, 72 (26.3%), 74 (26.3%) were between 54 and 63 years of age and sixty five (23.6%) were 64 and above years of age. The mean age for the studied population was 53.07 (SD=12.784) years (range from 24 to 87 years). A total of 165 (60.0%) of the patients included in the study were married. 97 (35.3%) were college and above. Regarding occupation 76 (27.6%) works a private business and 71(25.8%) were employee. Nearly half 126 (45.8%) of the respondents get a monthly income between 501 and 1500. Most of the study participants 260 (94.5%) were from urban area. These descriptions and other socio demographic characteristics are given in Table 1.
| Variable | Sex | ||
|---|---|---|---|
| Male | Female | Total | |
| 142 (51.6%) | 133 (48.4%) | 277 (100.0%) | |
| Age | |||
| 24-33 | 10 (7.0) | 8 (6.0 %) | 18 (6.5%) |
| 34-43 | 17 (37.0) | 29 (21.8%) | 46 (16.7%) |
| 44-53 | 42 (29.6%) | 30 (22.6%) | 72 (26.2%) |
| 54-63 | 35 (24.6%) | 39 (29.3%) | 74 (26.9%) |
| 64 and above | 38 (26.8%) | 27 (20.3%) | 65 (23.6%) |
| Marital status | |||
| Single | 24 (16.9 %) | 17 (12.8%) | 41 (14.9%) |
| Married | 90 (63.4%) | 75 (56.4%) | 165 (60.0%) |
| Divorced | 10 (7.0%) | 14 (1.5%) | 24 (8.7%) |
| Widowed | 18 (12.7%) | 27 (20.3%) | 45 (16.4%) |
| Educational level | |||
| Illiterates | 25 (17.6%) | 42 (31.6%) | 67(24.4%) |
| Primary Education (1-8) | 37 (26.1%) | 37 (27.8%) | 74 (26.9%) |
| Secondary Education (9-12) | 18 (12.7%) | 19 (14.3%) | 37 (13.5%) |
| College and above | 62 (43.5%) | 35 (26.3%) | 97 (35.3%) |
| Occupation | |||
| Private business | 47 (33.1%) | 29 (21.8%) | 76 (27.6%) |
| Employee | 41 (28.9%) | 30 (22.6%) | 71 (25.8%) |
| Daily laborer | 10 (7.0%) | 0 (0.0%) | 10 (3.6%) |
| Retired | 35 (24.6%) | 9 (6.8%) | 44 (16.0%) |
| Student | 1 (0.7%) | 0 (0.0%) | 1 (0.4%) |
| Housewife | 2 (1.4%) | 62 (46.6%) | 64 (23.3%) |
| Farmer | 4 (2.8%) | 3 (2.3%) | 7 (2.5%) |
| Other | 2 (1.4%) | 0 (0.0%) | 2 (0.7%) |
| Residence | |||
| Urban area | 135 (95.1%) | 125 (94.0%) | 260 (94.5%) |
| Rural area | 7 (4.9%) | 8 (6.0%) | 15 (5.5%) |
| Income | |||
| £500 | 9 (6.3%) | 21 (15.8%) | 30 (10.9%) |
| 501-1500 | 62 (43.7%) | 64 (48.1%) | 126 (45.8%) |
| 1501-2500 | 35 (24.6%) | 27 (20.3%) | 62 (22.5%) |
| >2500 | 36 (25.4%) | 21 (15.8%) | 57 (20.7%) |
Table 1: Socio-demographic characteristics of T2DM patients with attending the in ZMH, May 2016.
Mornsky measurement scale of T2DM patients with sociodemographic characteristics at ZMH, May 2016
The four types of Mornsky Medication adherence measurements scale were described in accordance to the socio-demographic characteristics of study participants, the questions were about forgetfulness to take medication (Table 2), carelessness in taking the medication (Table 3), stopping medication when feeling worse (Table 4) and stopping medication when feeling better (Table 5).
| Variable | Do you ever forget to take your medicine? | ||
|---|---|---|---|
| Yes | No | Total | |
| Sex | |||
| Male | 52 (36.6%) | 90 (63.4%) | 142 (100%) |
| Female | 65 (48.9%) | 68 (51.1%) | 133 (100%) |
| Total | 117 (42.2%) | 158 (57.7) | 275 (100%) |
| Age | |||
| 24-33 | 6 (33.3%) | 12 (66.7%) | 18 (100%) |
| 34-43 | 17 (37.0%) | 29 (63.0%) | 46(100%) |
| 44-53 | 29 (40.3%) | 43 (59.7%) | 72 (100%) |
| 54-63 | 40 (54.1%) | 34 (45.9%) | 74 (100%) |
| 64 and above | 25 (38.5%) | 40 (61.5%) | 65 (100%) |
| Marital status | |||
| Single | 19 (46.3%) | 22 (53.7%) | 41 (100.0%) |
| Married | 66 (40.0%) | 99 (60.0%) | 165 (100%) |
| Divorced | 8 (33.3%) | 16 (66.7%) | 24 (100%) |
| Widowed | 24 (53.3%) | 21 (46.7%) | 45 (100%) |
| Educational level | |||
| Illiterates | 31 (46.3%) | 36 (53.7%) | 67 (100%) |
| Primary Education (1-8) | 40 (54.1%) | 34( 45.9%) | 74 (100%) |
| Secondary Education (9-12) | 13 (35.1%) | 24 (64.9%) | 37 (100%) |
| College and above | 33 (34.0%) | 64 (66.0%) | 97 (100%) |
| Occupation | |||
| Private business | 27 (35.5%) | 49 (64.5%) | 76 (100%) |
| Employee | 33 (46.5%) | 38 (53.5%) | 71 (100%) |
| Daily laborer | 5 (50.0%) | 5 (50.0%) | 10 (100%) |
| Retired | 18 (40.9%) | 26 (59.1%) | 44 (100%) |
| Student | 1 (100%) | 0 (0.0%) | 1 (100%) |
| Housewife | 30 (46.9%) | 34 (53.1%) | 64 (100%) |
| Farmer | 2 (28.6%) | 5 (71.4%) | 7 (100%) |
| Other | 1 (50.0%) | 1 (50.0%) | 2 (100%) |
| Residence | |||
| Urban area | 112 (43.1%) | 148 (56.9%) | 260 (100%) |
| Rural area | 117 (42.5%) | 10 (66.7%) | 15 (100%) |
| Income | |||
| £500 | 19 (63.3%) | 11 (36.7%) | 30 (100%) |
| 501-1500 | 65 (51.6%) | 61 (48.4%) | 126 (100%) |
| 1501-2500 | 21 (33.9%) | 41 (66.1%) | 62 (100%) |
| >2500 | 12 (21.1%) | 45 (78.9%) | 57 (100%) |
Table 2: Mornsky measurement of adherence on forgetfulness in taking medications at ZMH, May 2016.
| Variable | Are you careless at times about taking your medicine? | |||
|---|---|---|---|---|
| Yes | No | Total | ||
| Sex | ||||
| Male | 27 (19.0%) | 115 (81.0%) | 142 (100%) | |
| Female | 32 (24.1%) | 101 (75.9%) | 133 (100%) | |
| Total | 59 (21.5%) | 216 (78.5%) | 275 (100%) | |
| Age | ||||
| 24-33 | 7 (38.9%) | 11 (61.1%) | 18 (100%) | |
| 34-43 | 8 (17.4%) | 38 (82.6%) | 46 (100%) | |
| 44-53 | 14 (19.4%) | 58 (80.6%) | 72 (100%) | |
| 54-63 | 20 (27.0%) | 54 (73.0%) | 74 (100%) | |
| 64 and above | 10 (15.4%) | 55 (84.6%) | 65 (100%) | |
| Marital status | ||||
| Single | 11 (26.8%) | 30 (73.2%) | 41 (100%) | |
| Married | 33 (20.0%) | 132 (80.0%) | 165 (100%) | |
| Divorced | 5 (20.8%) | 19 (79.2%) | 24 (100%) | |
| Widowed | 10 (22.2%) | 35 (77.8%) | 45 (100%) | |
| Educational level | ||||
| Illiterates | 15 (22.4%) | 52 (77.6%) | 67 (100%) | |
| Primary Education (1-8) | 18 (24.3%) | 56 (75.7%) | 74 (100%) | |
| Secondary Education (9-12) | 8 (21.6%) | 29 (78.4%) | 37 (100%) | |
| College and above | 18 (18.6%) | 79 (81.4%) | 97 (100%) | |
| Occupation | ||||
| Private business | 12 (15.8%) | 64 (84.2%) | 76 (100%) | |
| Employee | 20 (28.2%) | 51 (71.8%) | 71 (100%) | |
| Daily laborer | 3 (30.0%) | 7 (70.0%) | 10 (100%) | |
| Retired | 5 (11.4%) | 39 (88.6%) | 44 (100%) | |
| Student | 1 (100%) | 0 (0.0%) | 1 (100%) | |
| Housewife | 16 (25.0%) | 48 (75.0%) | 64 (100%) | |
| Farmer | 1 (14.3%) | 6 (85.3%) | 7 (100%) | |
| Other | 1 (50.0%) | 1 (50.0%) | 2 (100%) | |
| Residence | ||||
| Urban area | 55 (21.2%) | 205 (78.8%) | 260 (100%) | |
| Rural area | 4 (26.7%) | 11 (73.3%) | 15 (100%) | |
| Income | ||||
| £500 | 11 (36.7%) | 19 (63.3%) | 30 (100%) | |
| 501-1500 | 32 (25.4%) | 94 (74.6%) | 126 (100%) | |
| 1501-2500 | 9 (14.5%) | 53 (85.5%) | 62 (100%) | |
| >2500 | 7 (12.3%) | 50 (87.7%) | 275 (100%) | |
Table 3: Mornsky measurement of adherence on carelessness in taking the medications at ZMH, May 2016.
| Variable | Sometimes if you feel worse when you take the medicine, do you stop taking it? | ||
|---|---|---|---|
| Yes | No | Total | |
| Sex | |||
| Male | 19 (13.4%) | 123 (86.6%) | 142 (100%) |
| Female | 24 (18.0%) | 109 (82.0%) | 133 (100%) |
| Total | 43 (15.6%) | 232 (84.4%) | 275 (100%) |
| Age | |||
| 24-33 | 3 (16.7%) | 15 (83.3%) | 18 (100%) |
| 34-43 | 4 (8.7%) | 42 (91.3%) | 46 (100%) |
| 44-53 | 15 (20.8%) | 57 (79.2%) | 72 (100%) |
| 54-63 | 12 (16.2%) | 62 (83.8%) | 74 (100%) |
| 64 and above | 9 (13.8%) | 56 (86.2%) | 65 (100%) |
| Marital status | |||
| Single | 7 (17.1) | 34 (82.9%) | 41 (100%) |
| Married | 27 (16.4%) | 138 (83.6%) | 165 (100%) |
| Divorced | 2 (8.3%) | 22 (91.7%) | 24 (100%) |
| Widowed | 7 (15.6%) | 38 (84.4%) | 45 (100%) |
| Educational level | |||
| Illiterates | 12 (17.9%) | 55 (82.1%) | 67 (100%) |
| Primary Education (1-8) | 20 (27.0%) | 54 (73.0%) | 74 (100%) |
| Secondary Education (9-12) | 5 (13.5%) | 32 (86.5%) | 37 (100%) |
| College and above | 6 (6.2%) | 91 (93.8%) | 97 (100%) |
| Occupation | |||
| Private business | 7 (9.2%) | 69(90.8%) | 71 (100%) |
| Employee | 14 (19.7%) | 57 (80.3%) | 10 (100%) |
| Daily laborer | 0 (0.0%) | 10 (100%) | 44 (100%) |
| Retired | 5 (11.4%) | 39 (88.9%) | 1 (100%) |
| Student | 0 (0.0%) | 1 (100.0%) | 64 (100%) |
| Housewife | 15 (23.4%) | 49 (76.6%) | 7 (100%) |
| Farmer | 1 (14.3%) | 6 (85.7%) | 2 (100%) |
| Other | 1 (50.0%) | 1 (50.0%) | 275 (100%) |
| Residence | |||
| Urban area | 41 (15.8%) | 219 (84.2%) | 260 (100%) |
| Rural area | 2(13.3%) | 13 (86.7%) | 15 (100%) |
| Income | |||
| £500 | 5(16.7%) | 25 (83.3%) | 30 (100%) |
| 501-1500 | 29 (23.0%) | 97 (77.0%) | 126 (100%) |
| 1501-2500 | 6 (9.7%) | 56 (90.3%) | 62 (100%) |
| >2500 | 3 (5.3%) | 54 (94.7%) | 57 (100%) |
Table 4: Mornsky measurement of adherence on stopping medications when feeling worse at ZMH, May 2016.
| Variable | When you feel better do you sometimes stop taking your medicine? | ||
|---|---|---|---|
| Yes | No | Total | |
| Sex | |||
| Male | 30 (21.1%) | 112 (78.9%) | 142(100%) |
| Female | 32 (24.1%) | 101 (75.9%) | 133 (100%) |
| Total | 62 (22.2%) | 213 (77.5%) | 275 (100%) |
| Age | |||
| 24-33 | 4(22.2%) | 14 (77.8%) | 18 (100%) |
| 34-43 | 7 (15.2%) | 39 (84.8%) | 46 (100%) |
| 44-53 | 16 (22.2%) | 56 (77.8%) | 72 (100%) |
| 54-63 | 20 (27.0%) | 54 (73.0%) | 74 (100%) |
| 64 and above | 15 (23.1%) | 50 (76.9%) | 65 (100%) |
| Marital status | |||
| Single | 6(14.6%) | 35(85.4%) | 41 (100%) |
| Married | 39 (23.6%) | 126 (76.6%) | 165 (100%) |
| Divorced | 5 (20.8%) | 19 (79.2%) | 24 (100%) |
| Widowed | 12 (26.7%) | 33 (73.3%) | 45 (100%) |
| Educational level | |||
| Illiterates | 20 (29.9%) | 47 (70.1%) | 67 (100%) |
| Primary Education (1-8) | 25 (33.8%) | 49 (66.2%) | 74 (100%) |
| Secondary Education (9-12) | 8 (21.6%) | 29 (78.4%) | 37 (100%) |
| College and above | 9 (9.3%) | 88 (90.7%) | 97 (100%) |
| Occupation | |||
| Private business | 14 (18.4%) | 62 (81.6%) | 76 (100%) |
| Employee | 17 (23.9%) | 54 (76.1%) | 71 (100%) |
| Daily laborer | 2 (20.0%) | 8 (80.0%) | 10 (100%) |
| Retired | 9 (20.5%) | 35 (79.5%) | 44 (100%) |
| Student | 1 (100.0%) | 0 (0.0%) | 1 (100%) |
| Housewife | 17 (26.6%) | 47 (73.4%) | 64 (100%) |
| Farmer | 1 (14.3%) | 6 (85.7%) | 7 (100%) |
| Other | 1 (50.0%) | 1 (50.0%) | 2 (100%) |
| Residence | |||
| Urban area | 59 (22.7%) | 201 (77.3%) | 260 (100%) |
| Rural area | 3 (20.0%) | 12 (80.0%) | 15(100%) |
| Income | |||
| £ 500 | 9 (30.0%) | 21 (70.0%) | 30 (100%) |
| 501-1500 | 37 (29.4%) | 89 (70.6%) | 126 (100%) |
| 1501-2500 | 12 (19.4%) | 50 (80.6%) | 62 (100%) |
| >2500 | 4 (7.0%) | 53 (93.0%) | 57 (100%) |
Table 5: Mornsky measurement of adherence on stopping medication when feeling better at ZMH, May 2016.
Levels of adherence in patients with T2DM
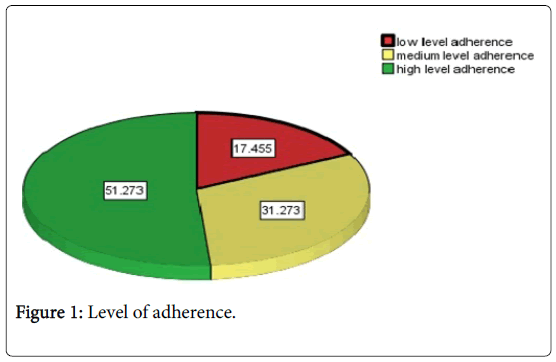
From the four Mornsky’s adherences measuring scale questions forgetfulness was the major 117 (42.5%) scored from all respondents. Based on this the 4 item Morisky measuring scale Instrument patients scoring, Out of the above four questions the patients who scored 0 was highly adherent, 1, 2 was medium adherent and 3, 4 was low adherent to their anti-diabetic medication. In the pattern of adherence to their medications, 141 (51.3%) of patients have high level of adherence, 86 (31.3%) have medium level and 48 (17.5%) have low level of adherence (Figure 1).
Levels of adherence in patients with T2DM by sociodemographic factor
The proportion of socio-demographic factors in relation to high level adherence was male 82(57.7%) are more adherent as compared to their female counterparts, which is 59 (51.3%), elderly age group were more 38(58.5%) adherent relative to other age groups, In terms of educational status who are college and above graduates were 58(59.8%) more adherent as compared to other educational status. Those whose income was more than 2,500 Ethiopian birr monthly were 40 (70.2%) more adherent relative to other income status.
The three level of adherance are classified in to two, in which the low level adherance and Middle level adherance as non-adherent and the high level as adherant to their anti dibetic medication, based on this 51.3% has become adherent and 48.7% Non-adherent.
In this study only 51.3% were adherent to their anti-diabetic medication, while the remained 48.7% were not. The medications that are taken by these T2DM Patients were insulin 154 (56.0%), Metformin 211 (76.7%) either as a single drug or in combination, and Glibenclamide 62 (22.5%). Most of them were on dual therapy for their diabetes disorder which is Insulin and Metformin. From those who are taking insulin T2DM patients, those who are on NPH (Neutral Protamine Hagedorn) insulin were 117 (42.5%) and who are on Regular Insulin were 37 (13.5%). Most of the patients 244 (88.7%), the last time they visited their physician was before three month and from these those who checked their Fasting Blood Glucose on the day of their clinical visit were 269 (86.9%).
Knowledge on diabetic disorder and its complications among T2DM patients attending the diabetic clinic in ZMH
Out of 275 respondents, 267 (97.1%) replied that they have good knowledge on T2DM and the other 8 (2.9%) has no Knowledge on T2DM. at least a single complication was known by 244 (88.7%) of them. Diabetic Foot Ulcer 218 (79.3%) and eye complication 200 (72.7%) were identified by participants as a complication of DM.
Reasons for non-adherence
In this study participants were forwarding their reasons that were responsible for non-adherence to their medication. Among such reasons the following were identified as forgetfulness (36%), lack of patient education (33.10%), financial problem or cost of medication (27.6%), lack of patient provider relationship (26.9%), shortage or availability problem (25.1%), health facility being far or accessibility problem (21.8%), problem in dosage form (15.5%), feeling healthy without medication (13.8%) afraid of addiction (10.5%) and being afraid of side effect were 6.5%.
Socio demographic factors associated with medication nonadherence among type 2 diabetic patients
The results of bivariate logistic regression analysis among the socio demographic characteristics of respondents’ Age, Marital status and Educational status did not show statistical association with Medication Non-adherence where as sex, Educational status, occupation and income show statistical association with Medication Non-adherence. Female (COR=1.714, 95%CI; 1.063-2.763) were more likely to be associated with medication non-adherence as compared to men. Respondents with educational status of completing college and above (COR=0.615, 95%CI; 0.328-1.152) are less likely to be non-adherent, as compared to those who were illiterate. Employee (COR=1.873, 95%CI; 0.973-3.606), and house wife (COR=1.752, 95%CI; 0.895-3.430) were more likely to be associated with medication non-adherence as compared to private business owners. Monthly income who earn Ethiopian Birr of 1501-2501(COR=0.418, 95%CI; 0.170-1.026) and income who earn above Ethiopian Birr of 2501(COR=0.246, 95%CI; 0.097, 1.626) were less likely to be associated with medication nonadherence as compared to respondents whose earning is less than or equal to 500 Ethiopian birr.
Clinical characteristics associated with diabetic medication non-adherence
The results of bivariate logistic regression analysis showed the following factors to have association with non-adherence. These were Patient provider communication, Patient education, Cost of medication and accessibility to the health facility. DM patients who are not comfortable to ask question to the health provider (COR=6.81, 95%CI: 3.611-12.845) and patients whose not getting enough education from health provider (COR=6.172, 95%CI; 3.654-10.427), patient who can’t afford medication (COR=8.571, 95%CI: 0.924-79.533) and health facility is far (COR=4.627, 95%CI: 0.50142-0.740) were more likely to be associated with medication nonadherence.
Non pharmacological characteristics associated with diabetic medication non-adherence
The results of bivariate logistic regression analysis among Nonpharmacological characteristics respondents were exercise and Duration of exercise. T2DM patients who do not exercise (COR=2.528, 95%CI: 1.510-4.230) are more likely to be non-adherent compared to their counter parts. T2DM patients who don’t exercise every day for more than 30 minutes a day (COR=2.986, 95%CI: 1.541-5.785) are more likely to be non-adherent compared to their counter parts.
Multivariate logistic regression analysis result of factors associated with anti-diabetic medication non-adherence among T2DM patients attending the diabetic clinic in ZMH
The results of Multivariate logistic regression analysis among the socio demographic characteristics of respondents, there was no association between adherence to sex, occupation, residence whereas, income showed significant association. Income whose getting more than 2501 Ethiopian birr are less likely to be non-adherent by (AOR=0.141, 95% CI; 0.046-0.430) than T2DM patients whose getting less than 500 Ethiopian birr keeping other socio demographic characteristics constant. Patients with lack of patients-provider relationship (p-value 0.001) three times more likely (AOR= 3.432, 95% CI: 1.695-6.948) and patients whose not getting enough education from health provider almost four times more likely (AOR= 3.854, 95%CI: 2.156-6.888), to be associated with medication non-adherence keeping other clinical characteristics constant. T2DM patients who don’t exercise every day for more than 30 minutes a day with (p-value 0.001) (AOR=3.12, 95% CI: 1.607-6.116) are three times more likely to be non-adherent compared to their keeping other behavioral factors constant (Table 6).
| Variable | Adherence | |||
|---|---|---|---|---|
| Yes | No | COR , 95% CI | AOR, 95% CI | |
| Sex | ||||
| Male | 82 (57.1%) | 60 (42.3%) | 1 | |
| Female | 59 (44.4%) | 74 (55.6%) | 1.714(1.063,2.763) | |
| Age | ||||
| 24-33 | 9 (50.0%) | 9 (50.0%) | 1 | |
| 34-43 | 25 (54.3%) | 21 (45.7%) | 0.840 (0.282,2.501) | |
| 44-53 | 38 (52.8%) | 34 (47.2%) | 0.895 (0.318,2.515) | |
| 54-63 | 31 (41.9%) | 43 (58.1%) | 1.387 (0.494,3.897) | |
| 64 and above | 38 (58.5) | 27 (41.5%) | 0.711 (249,2.025) | |
| Marital status | ||||
| Single | 19 (46.3%) | 22 (53.7%) | 1.00 | |
| Married | 89 (53.9%) | 76 (46.1%) | 0.737 (0.371,1.464) | |
| Divorced | 14 (58.3%) | 10 (41.7%) | 0.617 (0.223,1.706) | |
| Widowed | 19 (42.2%) | 26 (57.8%) | 1.182 (0.504,2.772) | |
| Educational level | ||||
| Illiterates | 32 (47.8%) | 35 (52.2%) | 1.00 | |
| Primary Education (1-8) | 30 (40.5%) | 44 (59.5%) | 1.341 (.688,2.613) | |
| Secondary Education (9-12) | 21 (56.8%) | 16 (43.2%) | 0.697 (0.311,1.563) | |
| College and above | 58 (59.8%) | 39 (40.2%) | 0.615 (0.328,1.152) | |
| Occupation | ||||
| Private business | 45 (59.2) | 31 (40.8%) | 1 | 1.00 |
| Employee | 31 (43.7) | 40 (56.3%) | 1.873 (0.973,3.606) | 1.822 (0.909,3.652) |
| Daily laborer | 5 (50.0%) | 5 (50.0%) | 1.452 (0.387,5.441) | 0.955 (0.233,3.919) |
| Retired | 26 (59.1%) | 18 (40.9%) | 1.005 (0.472,2.139) | 0.496 (0.204,1.201) |
| Housewife | 29 (45.3%) | 35 (54.7) | 1.752 (0.895,3.430) | 0.606 (0.255,1.436) |
| Farmer | 5 (71.4%) | 2 (28.6%) | 0.581 (0.106,3.186) | 0.348 (0.056,2.178) |
| Residence | ||||
| Urban area | 131 (50.4%) | 129 (49.6%) | 1 | |
| Rural area | 10 (66.7%) | 5 (33.3%) | 0.508 (0.169,1.526) | |
| Monthly Income | ||||
| £500 | 11 (36.7%) | 19 (63.0%) | 1 | 1 |
| 501-1500 | 54 (42.9%) | 72 (57.1%) | 0.772 (0.339,1.756) | 0.619 (0.255,1.501) |
| 1501-2500 | 36 (58.1%) | 26 (41.9%) | .418 (.170,1.026) | 0.239 (0.083,0.688) |
| >2500 | 40 (70.2%) | 17 (29.8%) | 0.246 (0.097,0.626) | 0.141 (0.046,0.430) |
| Patient provider communication | ||||
| Yes | 126 (63.0%) | 74 (37.0%) | 1 | 1 |
| No | 15 (20.0%) | 60 (80.0%) | 6.81 (3.611,12.845) | 3.432 (1.695,6.948) |
| Patient education | ||||
| Yes | 105 (70.9%) | 43 (29.1%) | 1 | 1 |
| No | 36 (28.3%) | 91 (71.7%) | 6.172 (3.654,10.427) | 3.854 (2.156,6.888) |
| Cost of medication (n=115) | ||||
| No | 4 (10.3%) | 35 (89.7%) | 1 | 1.00 |
| Yes | 1 (1.3) | 75 (98.7) | 8.571 (0.924,79.533) | 0.00 |
| Accessibility (n=115) | ||||
| No | 4 (7.3%) | 51 (92.7%) | 1 | 1.00 |
| Yes | 1 (1.7%) | 59 (98.3) | 4.627 (0.501,42.740) | 0.00 |
| Feeling healthy W/o medicine (n=115) | ||||
| No | 3 (3.9%) | 36 (94.7%) | 1 | |
| Yes | 2 (5.3%) | 74 (96.1%) | 0.730(0.117,4.563) | |
| Shortage of medicine (n=115) | ||||
| No | 1 (2.2) | 45 (97.8%) | 1 | |
| Yes | 4 (5.8%) | 65 (94.2% | 0.361 (0.039,3.338) | |
| Side effect (n=115) | ||||
| No | 5 (5.2%) | 92 (94.8%) | 1.00 | |
| Yes | 0 (0.0) | 18 (100.0%) | 0.00 | |
| Afraid of addiction(n=115) | ||||
| No | 3 (3.5%) | 83 (96.5%) | 1.00 | |
| Yes | 2 (6.9%) | 27 (93.1%) | 2.049 (0.325, 12.919) | |
| Dosage form (n=115) | ||||
| No | 2 (2.8) | 69 (97.2%) | 1 | |
| Yes | 3 (7.0%) | 40 (93.0%) | 0.386 (0.062,2.412) | |
| Forgetfulness (n=115) | ||||
| No | 0 (0.0%) | 14 (100.0%) | 1.00 | |
| Yes | 4 (4.0%) | 95 (96.0%) | 0.00 | |
| Alcohol use | ||||
| Yes | 27 (47.4%) | 30 (52.6%) | 1.00 | |
| No | 114 (52.3%) | 104 (47.7%) | 0.821 (0.458,1.472) | |
| Smoking | ||||
| Yes | 9 (45.0%) | 11 (55.0%) | 1 | |
| No | 132 (51.8%) | 123 (48.2%) | 0.762 (0.305,1.903) | |
| Exercise | ||||
| Yes | 106 (58.9%) | 74 (41.1%) | 1 | |
| NO | 34 (36.2%) | 60 (63.8%) | 2.528 (1.510,4,230) | |
| Duration of exercising per day in minute per day (n=186) | ||||
| ≥30 minute per day | 89 (66.9%) | 44 (33.1%) | 1 | 1 |
| 21 (40.4%)31 (59.6)2.986 (1.541,5.785)3.12 (1.607,6.116) | ||||
| Duration of DM | ||||
| 1-5 years | 42 (44.7%) | 52 (55.3%) | 1 | 1 |
| 6-10 years | 42 (52.5%) | 38 (47.5%) | 0.731 (0.402,1.329) | 2.073 (0.898,4.785) |
| 11-15 years | 30 (52.6%) | 27 (47.4%) | 0.727 (0.376,1.407) | 1.535 (0.657,3.582) |
| 16 and above years | 27 (61.4%) | 17 (38.6%) | 0.509 (0.245,1.056) | 1.299 (0.526,3.210) |
Table 6: Multivariate logistic regression analysis result of factors associated with anti-diabetic medication non-adherence among T2DM patients attending the diabetic clinic in ZMH, May 2016.
Discussions
The result of this study has different aspects involved such as, pharmacological and non-pharmacological approaches. For the patient both approaches need a strict adherence to the agreements reached with the physician in order to achieve the desired goals of treatment. In addition, factors that could influence Medication Adherence were also studied. Poor medication adherence seems to be a significant barrier to attainment of positive clinical outcomes among type 2 diabetes patients in both developed and developing countries [10]. Non adherence to medications has been reported as the primary factor responsible for unscheduled consults and hospitalizations among patients with diabetes [11].
In this study Medication adherence is an intermediate outcome measure. Several studies have shown that improvement of medication adherence leads to better glycemic control [12,13]. This study has managed to found out that almost 52% of patients with diabetes had high level of adherence similar to the study found to be 60.2% in (Dares Salaam, Tanzania) [14], 58.3% in Kuala Lumpur, Malaysia [15] and higher than Central Nigeria that is 26.4% [16].The reasons for suboptimal level of adherence might be, according to a WHO report suggests that the social and economic factors, the health care provider or system, the characteristics of the disease, disease therapies and patient-related factors could be the reasons [17].
In this study, income whose (AOR=0.141, 95% CI; 0.046-0.430) to be significantly associated with anti-diabetic medication adherence. This is consistent to other studies done in India and United Arab Emirates (U.A.E) [18,19]. The possible explanation for low adherence with low income patients may be due to the cost of medicines purchased from outside pharmacy, or they were unable to continue the follow up for the treatment due to various economic reasons [20]. Since Ethiopia is one of the developing country in the world in which most of the population has a low income and this is one factor that contribute the low adherence. By Most of T2DM patients during this study it was reported that high cost of the medication was one of the reasons for medication non-adherence consistent retrospective study in New Jersey (United States) has suggested that, Cost is significantly associations with (P value<0.05) low adherence.
In this study forgetfulness was the major reason for non-adherence, reported by 99 (36%) of the patients, similar to a study done in Adama, Ethiopia [21]. A Randomized Controlled Trial (RCT) study conducted in Netherland Simple interventions that are relatively easy to implement in busy daily practice are most promising to minimize forgetfulness. Alarm clock can be helpful especially useful in improving adherence for these patients who forget to take pills even though the identification of these patients appears to be difficult [22], since it asks a lot of efforts, more health professionals and cost.
Drug side effect was the other reason mentioned with nonadherence. In contrast to the Tanzania study where drug side effects accounted for about 11.6% of non-adherence, only 6.5% of this study participants reported drug side effects as their reason for nonadherence [23]. In this study 76 (27.6%) patients has reported a lack of finance to buy the medication. One of the major challenges for adherence is financial problem. Failure to afford medications is the most common reason for poor adherence among DM patients [24].
The other reason mentioned for non-adherence was “not being comfortable to ask question related to T2DM” and short consultation time, lack of privacy resulting in inadequate physician-patient communication during consultation time. This may be aroused due to shortage of health professional, high patient workload and poor work environment in the hospital setup in most resources limited countries including Ethiopia. One of the many factors that contribute to medication non adherence includes patient provider communication and relationship [25]. In this study it has been reported by 74 (26.9%) of the T2DM patients that they don’t have good communication with their healthcare provider.
Patients with lack of patients-provider relationship (p-value<0.001) three times more likely (AOR=3.432, 95%CI: 1.695-6.948) to be nonadherent. This finding is also similar with the study done in Texas USA two times more likely to be associated with non-adherence with significant (p<0.001) [26]. This may be lack of interpersonal skills of the healthcare providers. Different literatures suggest that providerlevel factors such as the patient physician relationship and communication, provider attitudes toward diabetes and provider knowledge and skills related to diabetes treatment have the potential to influence adherence behavior. Training in communication is an essential, and effective, component of medical education and may be even more important in residency training for physicians [27,28].
In this study health care provider not giving enough information about the diabetic medication are reported by the study participant which is 126 (45.5%) and lack of getting enough education from healthcare provider almost four times more likely (AOR=3.854, 95%CI: 2.156-6.888), to be associated with medication non-adherence in whom it has a major influence on adherence leading to nonadherence for T2DM patients. This result might be due to the lack of patient education program in the hospital or inadequate consultation time.
In this study drug unavailability was the other reason associated with non-adherence. In contrast to the study done in Uganda where drug unavailability (drugs stock-outs) accounted for about 33.8% of non-adherence [29], but that of this study only 25.1% of these patients reported drugs unavailability as their reason for non-adherence. Even though in ZMH sometimes, patients are forced to refill their prescriptions from private drug retail outlets which make it difficult to afford it and leading the patients to non-adherence. Unfortunately, only few patients can afford such price.
In this study, patients who are non-adherent to their anti-diabetic Medication compared to socio demographic status was not statistically significant. The lack of association between anti-diabetic drug adherence and socio demographic was also seen in other studies [30-33]. Possible explanation for lack of association might be patients were over- reporting their adherence. These explanations could account for the situation observed in this study.
In the management of diabetes involves a healthy lifestyle and longterm adherence to treatment, aimed at controlling the glycemic level. It has been indicated in this study that 89 (32.4%) of the patients are not exercising. Compared to a study conducted in Finland indicated 10% T2DM took no exercise at all [34], that of this study the findings are high, that is 32.4% [35]. In this study it was found that T2DM patients who don’t exercise every day for more than 30 minutes a day with (pvalue 0.001) (AOR=3.12, 95% CI: 1.607-6.116) are three times more likely to be non-adherent, similar to a cross-sectional study conducted in the southeastern region of Brazil, It was reported that exercise (p=0.006) were significantly associated with the chance of patients, with non-adherence to exercise is almost twice more likely for nonadherence to their medications [36,41]. The possible explanation could be patients do not follow Healthcare Providers’ Recommendations. T2DM patients who are drinking alcohol found to be 21.1%. Compared to research conducted in CA, USA Current alcohol consumption was reported to be 50.8% of adults with T2DM patients, the results which is find in this study is lower. And this same research concluded that Alcohol consumption is a marker for poorer adherence. Medications without life style and behavioral change cannot be effective to reach the targeted glycemic controls. T2DM patients who are currently smoking are 6.9%. Comparing to a study done in Germany reported that prevalence of smoking in T2DM was 17.3% patients [37,40]. In this study the results found 6.9% was lower. Literatures have been reported on the prevention of T2DM adherence to regular physical exercise, smoking cessation and not drinking alcohol has been effective in reducing the onset of the disease [38,39].
Strengths of the study
Since, little studies have been done to assess the medication adherence among diabetic T2DM in hospital settings in Ethiopia; this study might give some more information about medication adherence in ZMH and generally in Ethiopia. Efforts had been made in convincing patients about the benefits of the study, in order to avoid refusal, to participate in the study and get a full response rate from the patients. Data collectors were trained and health professionals too.
Limitations of the study
Since, this study shares the limitations of cross-sectional studies and hence it might suffer from temporal relationship establishment with some variables and might not provide much stronger evidence of causality. This study only addressed a self-reported level of nonadherence. Use of self-report method to assess adherence to antidiabetic drug therapy is associated with recall bias which means there is a tendency to overestimate the level of adherence. Most of study population was coming from urban area and this might limit the generalizability of the results to the whole population of DM including rural are patients.
Conclusion
The highest level of adherence to anti-diabetic medication by ambulatory type 2 diabetes patients in ZMH is suboptimal 51.3% and 31.3% have medium level of adherence. Forgetfulness was the most important reason preventing optimal adherence to prescribed medications. Income and exercise were factors that had a significant association with non-medication adherence. There was no patient education program implemented in the hospital. The patient physician relationship and communication is poor, the contact time is very few minutes. Special attention and adherence counseling should be given for those who are non-adherent to their diabetic medications. As a workable solution the hospital should use reminders for patients on follow-up to adhere to their medication such as Mobile phone short message service (SMS). Provision of alarm watch by ministry of health or non-governmental organization should be considered for those who had problems of forgetfulness in taking their medications. Health education system in the hospital should be improved through providing diabetes information using consumer medicine information (CMI), and videotapes related to their treatments. Healthcare workers within the hospital should improve the relationship they have with DM patients in the chronic illness clinic by allocating more counseling time.
Declarations
Competing interest: Authors declare that they have no competing interest.
Funding
The project was funded by YM and Jimma University has no role in the design, collection, analysis and interpretation of data and manuscript development.
Author’s Contribution
All authors equally contribute in design, analysis, and write-up of the project and in development of the manuscript. The author read and approved the final manuscript for possible publication.
Acknowledgement
The authors would like to express their gratitude for all study participants who provide their sincere response and precious time. All officials communicated in the study hospital who facilitate the study are acknowledged.
References
- Garc?´a-Pe´rez LE, Alvarez M, Dilla T, Gil-Guille´n V, Beltra´n D (2013) Adherence to Therapies in Patients with Type 2 Diabetes. Diabetes Ther 4: 175-194.
- Tamiru S, Alemseged F (2010) Risk Factors for Cardiovascular Diseases among Diabetic Patients in Southwest Ethiopia: Risk Factors for Cardiovascular Diseases. Ethiop J Health Sci 20: 121-127.
- Abdulazeez F, Omole M, Ojulari S (2014) Medication Adherence amongst Diabetic Patients in a Tertiary Healthcare Institution in Central Nigeria. Trop J Pharma Res 13: 997-1001.
- Vervloet M, Dijk L, Santen-Reestman J, Vlijmen B, Bouvy M, et al. (2011) Improving medication adherence in diabetes type 2 patients through Real Time Medication Monitoring: a Randomised Controlled Trial to evaluate the effect of monitoring patients’ medication use combined with short message service (SMS) reminders. BMC Health Serv Res 11: 5.
- Wabe N, Angamo M, Hussein S (2011) Medication adherence in diabetes mellitus and self-management practices among type-2 diabetics in Ethiopia. N Am J Med Sci 3: 418-423.
- Sokol MC, McGuigan KA, Verbrugge RR, Epstein R (2005) Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost. Med Care. 43: 521-530.
- Sharma T, Kalra J, Dhasmana D, Basera H (2014) Poor adherence to treatment: A major challenge in diabetes. 15: 26-29.
- Joanna Briggs Institute (2011) Educational interventions to promote oral hypoglycaemic adherence in adults with Type 2 diabetes. Best Practice 15: 1-4.
- WHO (2003) Adherence to long-term therapies: evidence for action. Geneva: Switzerland.
- Wild S,Roglic G, Green A, Sicree R, King H (2004) Global Prevalence of Diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 27: 1047-1053.
- WHO(2010) Member States adopted the WHO Global Strategy on Diet, Physical Activity and Health. NMH Fact Sheet: 1-2.
- Cefalu W (2014) Standards Of Medical Care In Diabetes:Abridged For Primary Care Physicians. Care Diabetes 1: 1-18.
- Sharma T, Kalra J, Dhasmana DC, Basera H (2014) Poor adherence to treatment: A major challenge in diabetes. J Indian Acad Clin Med 15: 26-29.
- Centers for Disease Control and Prevention (2014) National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States.
- Expert Committee on the Diagnosis and Classification of Diabetes Mellitus (2003) Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 25: 6-20.
- Loghmani ES (2005) Nutrition therapy for overweight children and adolescents with Type 2 Diabetes. Current Diabetes Reports [Internet]. Springer Nature 5: 385-390.
- Vermeire E, Wens J,Royen P, Biot Y, Hearnshaw H, et al. (2009) Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus.Cochrane Database Syst Rev 18: CD003638.
- Arifulla M, John L , SreedharanJ, Muttappallymyalil J, Basha S (2014) Patients’ Adherence to Anti-Diabetic Medications in a Hospital at Ajman, UAE. Malays J Med Sci 21: 44-49.
- Robbins J, Vaccarino V, Zhang H, Kasl S (2001) Socioeconomic Status and Type 2 Diabetes in African American and Non-Hispanic White Women and Men: Evidence From the Third National Health and Nutrition Examination Survey. Am J Pub Health 91: 76-83.
- Wan Nazaimoon WM, MdIsa SH, Wan Mohamad WB, Khir AS, Kamaruddin NA, et al. (2013) Prevalence of diabetes in Malaysia and usefulness of HbA1c as a diagnostic criterion.Diabet Med 30: 1-4.
- Ruhembe CC, Mosha TC, Nyaruhucha CN (2014) Prevalence And Awareness Of Type 2 Diabetes Mellitus Among Adult Population In Mwanza City, Tanzania. Tanzan J Health Res. 16: 1-11.
- Hall V, Thomsen R, Henriksen O, Lohse N (2011) Diabetes in Sub Saharan Africa 1999-2011: Epidemiology and public health implications. A systematic review. BMC Pub Health 11: 1-12.
- Cristiane L, Boas G, Lima M, Pace A (2014) Adherence to treatment for diabetes mellitus: validation of instruments for oral antidiabetics and insulin. Rev Latino-Am Enfermagem 22: 11-8.
- Clark M (2004) Adherence to treatment in patients with type 2 diabetes. J Diabetes Nurs 8: 386-391.
- Mahfouz E, Awadalla H (2011) Compliance to diabetes self-managementin rural El-MinIa, Egypt. Cent Eur J Pub Health 19: 35-41.
- Fairman K, Brenda Matheral B (2000) Evaluating medication adherence: which measure Is Right for Your Program?.J Man Care Pharm 6: 499-506.
- Ahmed AT, Karter J, Liu J (2006) Alcohol consumption is inversely associated with adherence to diabetes self-care behaviours. Diabet Med 23: 795-802.
- Cander S, Gül Ö, Gül C, Yava? S, Ersoy C (2015) Re-Training of Type 2 Diabetic Patients for Better Adherence to Diabetes Care Plan in Oral Anti-Diabetics. Turk Jem. 19: 49-54.
- Mann DM, Ponieman D, Leventhal H, Halm EA (2009) Predictors of adherence to diabetes medications: the role of disease and medication beliefs.J Behav Med 32: 278-284.
- Gelaw B, Mohammed A, Tegegne G, Defersha A, Fromsa M, et al. (2014) NonAdherence and Contributing Factors among Ambulatory Patients with Anti Diabetic Medications in Adama Referral Hospital. Adv Pharmacoepidemiol Drug Saf 3: 1-7.
- Morisky DE, Green LW, Levine DM (1986) Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 24: 67-74.
- Gangwar SS, Ahmad A, Singh SP, Parimalakrishnan S (2013) Medication Concordance Among The Out-Patients With Type 2 Diabetes In Kanpur At Northern India. Int. J. Res. Dev. Pharm. L. Sci 2: 251-257.
- Cani CG, Lopes Lda S, Queiroz M,Nery M (2015) Improvement in medication adherence and self-management of diabetes with a clinical pharmacy program: a randomized controlled trial in patients with type 2 diabetes undergoing insulin therapy at a teaching hospital. Clinics (Sao Paulo) 70: 102-106.
- Chua SS, Chan SP (2011) Medication adherence and achievement of glycaemic targets in ambulatory type 2 diabetic patients. J App Pharmaceutical Sci 1: 55-59.
- Shaimol T, Biju C,Anilasree B, Jayakrishnan S,Babu G (2014) Medication Adherence to Oral Hypoglycemic Agents in Type 2 Diabetic Patients. JPharma Res ClinPrac 4: 8-12.
- Zolnierek KB,DiMatteo MR (2009) Physician Communication and Patient Adherence to treatment: A Meta-analysis. Med Care 47: 826-834.
- Hsu C, Lemon J, Wong E,4, Cheng E, Perkins M, et al. (2014) Factors affecting medication adherence: patient perspectives from five veterans affairs facilities. BMC Health Serv Res 4: 533.
- Bagonza J,Rutebemberwa E, William Bazeyo (2015) Adherence to antidiabetic medication among patients with diabetes in eastern Uganda; a cross sectional study. BMC Health Serv Res 15: 168.
- Faria HTG, Rodrigues FFL,Zanetti ML,Araújo MFM, DamascenoMMC (2013) Factors associated with adherence to treatment of patients with diabetes mellitus. Acta Paul Enferm 26: 231-237.
- Schipf S, Schmidt C, Alte D, Werner A, Nave C, et al. (2009) Smoking prevalence in Type 2 diabetes: results of the Study of Health in Pomerania (SHIP) and the German National Health Interview and Examination Survey (GNHIES). Diabet Med 26: 791-797.
Citation: Mesfin Y, Assegid S, Beshir M (2017) Medication Adherence among Type 2 Diabetes Ambulatory Patients in Zewditu Memorial Hospital, Addis Ababa, Ethiopia. Epidemiology (Sunnyvale) 7:322. DOI: 10.4172/2161-1165.1000322
Copyright: © 2017 Mesfin Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7117
- [From(publication date): 0-2017 - Dec 03, 2025]
- Breakdown by view type
- HTML page views: 5954
- PDF downloads: 1163