Research Article Open Access
Medical Emergency Teams and Death at the Hospital - Do They Call Us? Results from an Integrated Educational Program with Medical Emergency Teams
Jorge Martins1, Nuno Príncipe1, Cláudia Dias2, Glória Campello1, Cristina Granja2,3* and Luís Azevedo2,31Hospital Pedro Hispano, Rua Dr Eduardo Torres, 4450 Matosinhos, Portugal
2Biostatistics and Medical Informatics Department, Faculty of Medicine of Porto, 4200 Porto, Portugal
3CINTESIS – Centre for Research in Health Technologies and Information Systems, Faculty of Medicine of Porto, 4200, Porto, Portugal
- *Corresponding Author:
- Dr. Cristina Granja
Biostatistics and Medical Informatics Department
Faculty of Medicine of Porto, 4200 Porto, Portugal
E-mail: cristinagranja28@gmail.com
Received date: February 08, 2012; Accepted date: March 24, 2012; Published date: March 26, 2012
Citation: Martins J, Príncipe N, Dias C, Campello G, Granja C, et al. (2012) Medical Emergency Teams and Death at the Hospital – Do They Call Us? Results from an Integrated Educational Program with Medical Emergency Teams. J Palliative Care Med 2:117. doi:10.4172/2165-7386.1000117
Copyright: © 2012 Martins J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: The present study was conducted with the main objective of evaluating the occurrence of Medical Emergency Team (MET) calls in patients who died during their hospital stay and their association with the presence of MET calling criteria in the 24 hour and 8 hour period before death and the existence of a do not resuscitate (DNR) order. Patients and methods: Retrospective analysis of the medical records of patients that died at the hospital between 1st October 2007 and 30th June 2008. Patients from the emergency room and intensive care department were excluded, as METs are not activated for these areas. Studied variables included demographics, MET calls, the presence of MET calling criteria within the 24 hour and 8 hour period before death and the existence of a DNR order. The occurrence of MET calls in patients who died during their hospital stay and their association with the presence of MET calling criteria in the 24 hours and 8 hours before death and the existence of a do not resuscitate (DNR) order were analyzed. Results: 348 patients died – in-hospital mortality rate - 2, 5%. 56% were male, mean age was 75 years old. Seventy-five percent exhibited an explicit DNR order written in their clinical records. Twenty-five percent (88 patients) had no explicit DNR order in their clinical records. For 39% of these MET was activated. Twenty–four percent of these presented at least one alarm sign 24h before the MET activation, being the most common threatened airway and persistent hypotension, 82% had an alarm sign during the last 8 h before MET activation, with airway threatened (59%) and downgrade of Glasgow Coma Scale > 2 points (32%) the most frequent. In 5 of the 88 patients there was no DNR order and no MET activation. In these patients no alarm signs were found 24h before death, and only in 2 patients, alarm signs 8 h before death were identified: downgrade of Glasgow Coma Scale > 2 points in one patient and hypotension in another patient. Four of these 5 patients died during the night shift. Conclusion: In the present study the detection of alarm signs in patients and the subsequent MET activation is a good quality of care indicator. When there is no MET system these data are not available and patients with alarm signs, if not corrected might proceed, with clinical deterioration until cardiac arrest and eventually death occur.
Keywords
Medical emergency teams; Hospital survival; Educational program; Hospital mortality; Cardiopulmonary resuscitation; Do notresuscitate orders
Introduction
A significant proportion of hospital patients experience serious adverse events during their stay, like cardiac arrest, unplanned admissions to the intensive care unit (ICU) and death [1,2]. In-hospital cardiac arrest is usually preceded by signs of physiological instability, giving an opportunity for early intervention, as long these signs are properly recognized [1-4]. Sandroni et al. in an extensive literature review found that interventions likely to improve survival from inhospital cardiac arrest include early recognition and stabilization of patients at risk [5].
Several reports indicate that medical emergency teams (METs) may decrease the incidence of cardiopulmonary arrests, inpatient mortality, unexpected intensive care unit (ICU) transfers and readmissions and ICU/inpatient lengths of stay [6-8]. Moreover, Jones et al. [9,10] have introduced the “dose effect” concept where the introduction of objective MET calling criteria resulted in a significant increase in MET call rates and a significant reduction on cardiac arrest rate and global mortality.
Based on a growing body of evidence coming from different reports, in 2005 took place the First Consensus Conference on Medical Emergency Team [11] which recommended the implementation of complete systems. A rapid response system should be based not only on a MET, but also in an entire system, including an afferent component (event detection and response triggering); an efferent component (first response in less than 15 min, personnel, equipment and methods to assess urgent unmet needs); a patient safety/process improvement component and a governance/administrative structure. We have shown that the program implemented in our hospital reproduced very closely these recommendations and we have described it elsewhere [12]. We have demonstrated that implementation of a program that included, widened emergency call criteria, institution-wide BLS (Basic Life Support) training, METs and records to enable audit of the entire program, may contribute to reduce cardiac arrest incidence and mortality in at risk patients. In particular we demonstrated that the effectiveness of the program was critically related with the staff education, awareness and responsiveness to physiological instability of the patients [12].
However, several important barriers to staff calling for higher assistance have been identified, being fear from criticism and fear from wrong evaluation of patients the most frequently reported in the literature [13].
In our own previous work we found that long term effectiveness of the program may decrease in the absence of periodic and continued implementation of educational interventions. Moreover, the program should be frequently audited to find areas of suboptimal care [12].
With such a program functioning at our hospital, in-hospital death could possibly occur only on two ways: a) after a DNR order, b) after a MET activation. On this latter hypothesis, a DNR order would eventually be decided by the MET.
The present study was conducted with the main objective of evaluating the occurrence of MET calls in patients who died during their hospital stay and their association with the presence of MET calling criteria in the 24 hour and 8 hour period before death and the existence of a do not resuscitate (DNR) order.
Materials and Methods
Hospital Pedro Hispano is an urban general hospital with 470 beds. The integrated emergency program is fully implemented in our hospital since 2003, it has been described elsewhere [12] and it included seven main points:
1. A MET responding to the widened alert criteria that were adapted from those published by Lee et al. [14] and by Hillman et al. [15]. METs include a physician and a nurse from the Intensive Care Unit (ICU). Physicians are trained in advanced life support and in management of critically ill patients. Nurses are trained in immediate life support and in critically ill patients care. They are on call 24 h per day; they have their own tasks in the ICU and a mobile radio to enable mobility inside the hospital. The radio is activated by a dedicated emergency phone line.
2. Institution-wide training on BLS to all physicians, nurses, auxiliary and administrative staff of our hospital. Widened emergency call criteria were extensively explained and trained.
3. Simulation scenarios with mannequins in the wards and video recording. After the simulation scenario, video visualization and discussion took place with the staff.
4. Interactive meetings with medical and nursing staff, these meetings took place mainly with the staff from medical and surgical wards, where the widened criteria were discussed and the role of the METs explained. These meetings were particularly important for ensuring compliance with the program.
5. “Information Posters” scattered throughout the hospital in strategically located points, i.e., wards, emergency department, radiology department, halls and outpatient clinics. These posters contain the widened emergency call criteria.
6. Audits based on records from the METs in order to guarantee compliance with the program. Feedback from these audits is given to the physicians and nurses involved, aiming to improve compliance with the program and improve their performance.
7. Periodic and non-scheduled audits to the hospital emergency equipment in order to ensure quality of the available material and readiness of response. A dedicated nurse is responsible for the audit of the system and has half time labour dedicated to this task.
Widened calling criteria include airway compromise, bradypnea or tachypnea, bradycardia or tachycardia, sustained hypotension, sudden loss of consciousness, decrease of more than two points in the Glasgow coma scale, repeated and prolonged seizures, respiratory arrest and cardiac arrest [12].
When there is a DNR order written in the medical record of the patient, the MET is not called in case of cardiac arrest. However, if these patients present the alarm signs included in the widened calling criteria (except cardiac arrest) the MET is called.
For the purpose of analysis we defined explicit DNR order (explicit group) as one that is written in the clinical record of the patient and is known by all the ward team. Implicit DNR order (implicit group) was defined as one that is not clearly written in the clinical record of the patient but it is known by all the ward team, as it applies to patients in the final stage of their disease process that were admitted in the wards for palliative care. Patients from the emergency room and intensive care department were excluded, as METs are not activated for these areas. Studied variables included sex, age, the presence of MET calling criteria within the 24 hour and 8 hour period before death, the existence of a DNR order and the graduation of the physician that wrote the DNR order. Causes of death and end stage diseases were only looked for in those clinical records where DNR was implicit.
Medical records from all patients were reviewed by two of the authors (JM and NP), and in particular, the inclusion in the explicit or implicit group was double-checked by those authors so there could be no doubts about the inclusion of patients in one of the groups. A database was created which included all the variables that were collected. A complete form explaining the concept for each variable and how it should be collected was also created. Collected data was reviewed together by the two authors; posteriorly, when there were doubts and in all the patients from the implicit group, there were meetings with two more authors (GC and CG) to arrive to a consensus. When DNR was implicit there was an extensive chart review to confirm and understand the implicit DNR as well as the consensus meeting. Criteria to inclusion of a patient in the implicit DNR group included: all the patients without a DNR order written in the clinical record, but with an order that was verbally transmitted to the ward nurses (this information could be checked in the nurses records); all patients where instead of a written explicit DNR order in the clinical records there was the written indication for comfort therapy. Comfort therapy included the maintenance of hydration and analgesia but not any curative intention.
We conducted a retrospective analysis of the medical records of patients that died at the hospital between 1st October 2007 and 30th June 2008.
The occurrence of MET calls in patients who died during their hospital stay and their association with the presence of MET calling criteria in the 24 hours and 8 hours before death and the existence of a do not resuscitate (DNR) order were analyzed.
Results
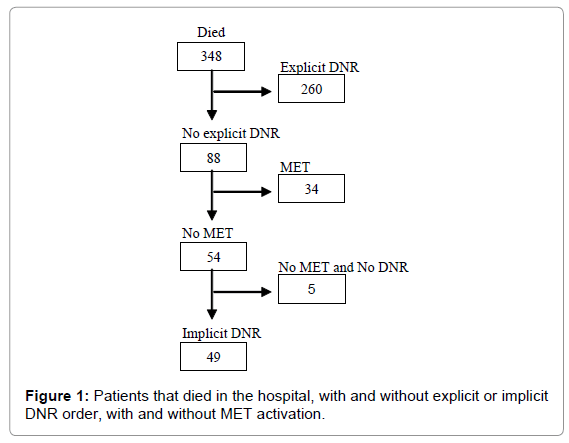
From the 13714 patients that were admitted in the hospital, 348 died (patients that died in the ICU and intermediate care units (IntCU) were excluded as MET are not activated for these areas) – hospital mortality rate - 2,5% (excluding ICU and IntCU); 56% were male, mean age was 75 (±13,6) years old. Seventy-five percent (n=260) exhibited an explicit DNR order written in their clinical records. Twenty-five percent (n=88) had no explicit DNR order in their clinical records (Figure 1). For 39% of these (n=34), MET was activated. Twenty–four percent (n=8) of these presented at least one alarm sign 24h before the MET activation, being the most common threatened airway and persistent hypotension (blood pressure inferior to 90 mmHg) (Figure 1), 82% (n= 28) had an alarm sign during the last 8 h before MET activation, with airway threatened (59%) and downgrade of Glasgow Coma Scale > 2 points (32%) the most frequent (Table 1). In 54 of the 88 patients there was no MET activation (Figure 1). An implicit DNR order was found in 49 of the 88 patients. From these, 33% (n=16) presented several alarm signs 24h before death, being airway threatened (18%) and hypotension (8%) the most frequent. Eighty-six percent (n=42) presented alarm signs 8 h before death being airway threatened (63 %), downgrade of Glasgow Coma Scale > 2 points (39 % ) and hypotension (25%) the most frequent (Table 2).
| n | (%) | |
|---|---|---|
| Alarm signs 24h before the MET activation | ||
| No | 26 | (76) |
| Yes | 8 | (24) |
| Alarm signs 8h before the MET activation | ||
| No | 6 | (18) |
| Yes | 28 | (82) |
| Airway threatened 8h before MET activation | ||
| No | 14 | (41) |
| Yes | 20 | (59) |
| Downgrade Glasgow >2 8h before MET activation | ||
| No | 23 | (68) |
| Yes | 11 | (32) |
Table 1: Patients with MET activation (n=34).
| n | (%) | |
|---|---|---|
| Alarm signs 24h before death | ||
| No | 33 | (67) |
| Yes | 16 | (33) |
| Airway threatened 24h before death | ||
| No | 10 | (82) |
| Yes | 9 | (18) |
| Hypotension 24h before death | ||
| No | 45 | (92) |
| Yes | 4 | (8) |
| Alarm signs 8h before death | ||
| No | 7 | (14) |
| Yes | 42 | (86) |
| Airway threatened 8h before death | ||
| No | 18 | (37) |
| Yes | 31 | (63) |
| Downgrade Glasgow >28h before death | ||
| No | 30 | (61) |
| Yes | 19 | (39) |
| Hypotension before death | ||
| No | 37 | (76) |
| Yes | 12 | (24) |
Table 2: Patients with implicit DNR (n=49).
In 5 of the 88 patients there was no explicit or implicit DNR order and no MET activation was recorded (Figure 1). In these patients no alarm signs were found 24h before death, and only in 2 patients, alarm signs 8 h before death were identified: downgrade of Glasgow Coma Scale > 2 points in one patient and hypotension in another patient. Four of these 5 patients died during the night shift. From the clinical records, we could not find any other information concerning these 5 patients.
Discussion
There are three main findings from the present study: First, the majority of patients who died in the hospital, died with an explicit DNR order, which is an indicator of quality of care and is in accordance with a continuous quality improvement program that was implemented in our hospital and was described elsewhere [12]. Second, only 5 patients (1,4%) died without an explicit or implicit order and without a MET activation, which again may reflect the continuous quality of care program. Reports from other institutions and in the literature are lacking and as thus we cannot compare our results with others. It is of notice that most of these deaths occurred during the night shift, a period of the day with less surveillance in the wards. Jones et al. [16] found a similar pattern where 53% of MET calls occurred during the night. These findings should question decisions on the availability of nurses on the wards during the night. Third, alarm signs were recorded 24h before MET activation in nearly a quarter of the patients in whom there was a MET activation and in more than eighty percent of the patients 8 hours before MET activation. This is in agreement with previous studies [1,3] and constitutes the main reason of the implementation of a MET system: the detection of alarm signs in patients at risk and the appropriate intervention to prevent death when this is a relevant and legitimate aim. In the present study the detection of alarm signs in patients and the subsequent MET activation is a good quality of care indicator. When there is no MET system these data are not available and patients with alarm signs if not corrected will proceed with clinical deterioration until cardiac arrest and eventually death occur. Further studies prospectively designed to see if alarm signs are timely detected and receive correct answer and feedback are thus needed. In addition, other indicators such as time between call and treatment and the success of the interventions applied by the team would also enhance our knowledge on this area.
Limitations from this study include: first, it is a retrospective analysis implying the limitations present on the clinical records; second, it is a single institution study with a MET system working, and although it has been described previously, it might not allow the generalizability of the results.
MET and Rapid Response Systems (RRS) are not free of criticism and the need for reflection, as complex systems involving human activities, they imply profound cultural changes in the practice of hospitals where they are implemented [17,18]. We believe that reporting results as the one we now present may further add to our knowledge and understanding on the benefits of RRS and MET.
This study has been partially presented in the 20th Annual Congress of the European Society of Intensive Care Medicine, in Lisbon, September 2008.
References
- Schein RM, Hazday N, Pena M, Ruben BH, Sprung CL (1990) Clinical antecedents to in-hospital cardiopulmonary arrest. Chest 98: 1388-1392.
- Bedell SE, Deitz DC, Leeman D, Delbanco TL (1991) Incidence and characteristics of preventable iatrogenic cardiac arrests. JAMA 265: 2815-2820
- Franklin C, Mathew J (1994) Developing strategies to prevent in-hospital cardiac arrest: analyzing responses of physicians and nurses in the hours before the event. Crit Care Med 22: 244-247.
- Goldhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A (1999) The patient-at risk team: Identifying and managing seriously ill ward patients. Anaesthesia 54: 853-860.
- Sandroni C, Nolan J, Cavallaro F, Antonelli M (2007) In-hospital cardiac arrest: incidence, prognosis and possible measures to improve survival. Intensive Care Med 33: 237-245.
- Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart GK, et al. (2003) A prospective before-and-after trial of a medical emergency team. Med J Aust179: 283-287.
- Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, et al. (2002) Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ324: 387-390.
- Bristow PJ, Hillman KM, Chey T, Daffurn K, Jacques TC, et al. (2000) Rates of in-hospital arrests, deaths and intensive care admissions: the effect of a medical emergency team.Med J Aust173: 236-240.
- Jones D, Bellomo R, DeVita MA (2009) Effectiveness of the Medical Emergency Team: the importance of dose. Crit Care 13: 313.
- Jones D, Bellomo R, Bates S, Warrillow S, Goldsmith D, et al. (2005) Long term effect of a medical emergency team on cardiac arrests in a teaching hospital. Crit Care9: R808-R815.
- DeVita M, Bellomo R, Hillman K, Kellum J, Rotondi A, et al. (2006) Findings of the First consensus conference on medical emergency teams. Crit Care Med 34: 2463-2478.
- Campello G, Granja C, Carvalho F, Dias C, Azevedo LF, et al. (2009) Immediate and long-term impact of medical emergency teams on cardiac arrest prevalence and mortality: a plea for periodic basic life-support training programs. Crit Care Med 37: 3054-3061.
- Jones L, King L, Wilson C (2009) A literature review: factors that impact on nurses’ effective use of the medical emergency team (MET). J Clin Nurs 18: 3379-3390.
- Lee A, Bishop G, Hillman KM, Daffurn K (1995) The Medical Emergency Team. Anaesth Intensive Care 23: 183-186.
- Hillman K, Parr M, Flabouris A, Bishop G, Stewart A (2001) Redefining in-hospital resuscitation: the concept of the medical emergency team. Resuscitation 48: 105-110.
- Jones D, Bates S, Warrillow S, Opdam H, Goldsmith D, et al. (2005) Circadian pattern of activation of the medical emergency team in a teaching hospital. Crit Care 9: R303-R306.
- Tee A, Calzavacca P, Licari E, Goldsmith D, Bellomo R (2008) Bench-to-bedside review: The MET syndrome – the challenges of researching and adopting medical emergency teams. Crit Care 12: 205.
- Litvak E, Pronovost PJ (2010) Rethinking Rapid Response Teams. JAMA 304: 1375-1376.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13944
- [From(publication date):
July-2012 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9437
- PDF downloads : 4507