Meckel Diverticulum in the Setting of Acute Appendicitis: A Mimic of Peri-Appendiceal Abscess
Received: 11-Sep-2018 / Accepted Date: 25-Sep-2018 / Published Date: 04-Oct-2018 DOI: 10.4172/2167-7964.1000300
Keywords: Meckel diverticulum; Meckel diverticulitis; Appendicitis; Periappendiceal abscess
Introduction
Meckel Diverticulum (MD) is the most common congenital malformation of the gastrointestinal tract, occurring in approximately 1%-3% of the population [1]. Although mostly asymptomatic, in 4%-6% population it becomes symptomatic and can present as intestinal obstruction, diverticulitis, bleeding, or perforation [2]. Intestinal obstruction is the most common presentation, but it is Meckel diverticulitis that often mimics acute appendicitis, with the diagnosis usually made after surgery [1]. We report a case in which MD was initially thought to be periappendiceal abscess and was sent for percutaneous drainage. But review of the scan before drainage suggested communication of the collection with the ileum clinching the diagnosis of MD and preventing inadvertent percutaneous drainage of a MD. The purpose of this report is to emphasize that a careful review of the images is warranted, especially when the inflamed appendix appears intact.
Case Report
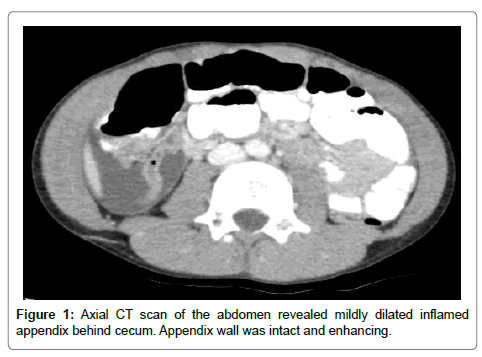
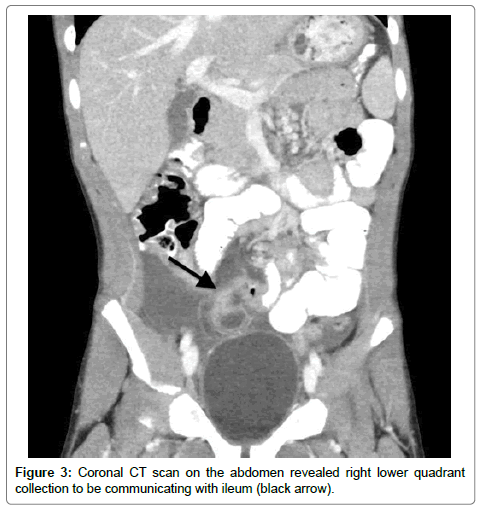
A 7-year-old otherwise healthy athletic boy presented to our institution with severe right lower quadrant (RLQ) abdominal pain and associated emesis. He has been having intermittent abdominal pain and cramps for a few weeks that parents attributed to spicy foods. Patient’s temperature was 100 F with a white cell count of 15000. Abdominal ultrasound showed free fluid in RLQ, however appendix was not visualized. This prompted a Computed Tomography (CT) scan, which revealed a mildly dilated appendix measuring 7 mm with enhancing walls and fat stranding (Figure 1). In addition there was an enhancing collection in RLQ near midline (Figure 2). Presumptive diagnosis of appendicitis with periappendiceal abscess was made. Patient was referred to biopsy and drainage service for percutaneous drainage of the abscess. On further review of CT scan before procedure revealed rimenhancing collection to be communicating with distal ileum (Figure 3). A suspicion of MD was raised and drainage was deferred. Patient was taken to the operating room by the referring Pediatric surgical team.
A 12-mm umbilical incision was made and 5-mm port was placed within the peritoneal cavity. After that two additional 5-mm ports were placed under direct visualization in mid and left lower abdomen. A loop of bowel was noted to be adherent onto the anterior abdominal wall, which appeared to be the site of the MD as it corresponded to the CT scan. MD was mobilized from the abdominal wall and appears to be perforated. Adjacent bowel and mesentery was significantly inflamed and edematous. Clamps were placed proximal and distal to MD and bowel was divided by electrocautery. A side-to-side stapled anastomosis was the performed and mesenteric defect was approximated with suture. Attention was then focused onto right lower abdomen. The umblical port was upsized to 12-mm trocar. The appendix was retrocecal, inflamed and had dense adhesions. The appendiceal adhesions were mobilized and linear stapler was used to divide across the base of appendix as well as mesoappendix. The appendix was extracted through the umblical port site.
Pathology demonstrated heterotopic gastric mucosa as well as perforation thus confirming the diagnosis. Post-operative course was uneventful and diet was slowly advanced as bowel function returned. At the time of discharge, the patient was tolerating a regular diet, having bowel movements and pain was controlled with oral medications.
Discussion
MD is a true diverticulum containing all of the layers of a normal small bowel and is usually located along the antimesentric border of ileum about 50 to 100 cm from the ileocaecal valve [3]. It is a common congenital gastrointestinal tract anomaly resulting from incomplete obliteration of the vitelline duct and accounts for 90% of all vitelline duct anomalies [4]. However MD as a mimic of periappendiceal abcess is very rare. To the best knowledge of the authors there is one case of a MD that was presumed to represent a periappendiceal abscess and percutaneously drained and retrospectively found later to reprsent a MD [2].
MD is commonly asymptomatic, with symptoms usually due to the presence of a complication. It is more common in males and classically presents before 2 years of age [5]. Bleeding is the most common presentation in children while intestinal obstruction is most common finding in adults [1]. The reason for bleeding is associated heterotopic tissue such as gastric or pancreatic tissue [4,5]. The main reasons for obstruction are adhesions, intussusception, volvulus and internal hernia [1]. Meckel diverticulitis is inflammation due to obstruction at the base of diverticulum.
Despite advances in imaging techniques, the diagnosis of symptomatic MD is still difficult with most cases preoperatively being diagnosed as acute appendicitis [1]. The most sensitive technique is Technetium-99m pertechnetate scintigraphy, with sensitivity and specificity as high as 90%-95% [1,6]. However it is less accurate in adults and moreover is rarely used for evaluation of acute abdomen, unless there is high clinical suspicion. Other imaging modalities are less sensitive and specific. Plain films and Fluoroscopic studies only show complications of MD such as bowel obstruction or perforation. Ultrasonography is non-specific and demonstrates only peritoneal fluid in majority of the cases. Rarely it can show inflamed diverticulum, which is difficult to distinguish from inflamed appendix.
CT is believed to be the most sensitive cross sectional modality for diagnosing complicated MD, in cases where normal appendix is visualized [7,8]. However as demonstrated in our case misdiagnosis can occur even on CT scan if meckel diverticulitis or perforation is secondarily complicated by appendicitis. Key finding is an intact appendix in the setting of a collection that has a communication with the ileum. Therefore a careful review of the images is warranted especially when the inflamed appendix appears intact as was in our case.
Management of asymptomatic MD incidentally detected during imaging or surgery for other reasons is controversial. Symptomatic MD is usually managed by diverticulectomy or segmental ileal resection and primary anastomosis [1].
References
- Emre A, Akbulut S, Yilmaz M, Kanlioz M, Aydin BE (2013) Double Meckel's diverticulum presenting as acute appendicitis: a case report and literature review. J Emerg Med 44: e321-324.
- Yang JC, Rivard DC, Morello FP, Ostlie DJ (2008) Presumed appendiceal abscess discovered to be ruptured Meckel diverticulum following percutaneous drainage. Ped Rad 38: 909-911
- Mohiuddin SS, Gonzalez A, Corpron C(2011) Meckel's diverticulum with small bowel obstruction presenting as appendicitis in a pediatric patient. JSLS 15: 558-561.
- Yahchouchy EK, Marano AF, Etienne JC, Fingerhut AL (2001) Meckel's diverticulum. Am Coll Surg 192: 658-662.
- Uppal K, Tubbs RS, Matusz P, Shaffer K, Loukas M (2011) Meckel's diverticulum: a review. Clin Anat 24: 416-422.
- Bani-Hani KE, Shatnawi NJ (2004) Meckel's diverticulum: comparison of incidental and symptomatic cases. World J Surg 28: 917-920.
- Elsayes KM, Menias CO, Harvin HJ, Francis IR (2007) Imaging manifestations of Meckel's diverticulum. AJR Am J Roentgenol 189:81-88.
- Bennett GL, Birnbaum BA, Balthazar EJ (2004) CT of Meckel's diverticulitis in 11 patients. AJR Am J Roentgenol 182: 625-629.
Citation: Siddiqui MA, Luke FE, Sartaj S (2018) Meckel Diverticulum in the Setting of Acute Appendicitis: A Mimic of Periappendiceal Abscess. OMICS J Radiol 7: 300. DOI: 10.4172/2167-7964.1000300
Copyright: © 2018 Siddiqui MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 4590
- [From(publication date): 0-2018 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 3833
- PDF downloads: 757