Research Article Open Access
Mechanical Evaluation of 4 Different Implant Design Systems
Torrealba Y1*, Lee H2, Passos S1, Nassar U3 and Pedroza J3
1Department of Restorative Dentistry, Faculty of Medicine and Dentistry, University of Alberta, Edmonton - Canada
2Undergraduate student of Biological Sciences, University of Alberta, Edmonton - Canada
3Advanced Dental Implant Institute in Puerto Rico, Department of Dental Research, School of Dental Medicine, University of Puerto Rico, San Juan – Puerto Rico, USA
- *Corresponding Author:
- Torrealba Y
Assistant Professor
Faculty of Medicine and Dentistry
Room 5-503, Edmonton Clinic Health Academy
University of Alberta, Edmonton, Alberta
Canada T6G 1C9
Tel: 780-492-753
E-mail: torrealb@ualberta.ca
Received Date: December 19, 2016; Accepted Date: December 27, 2016; Published Date: January 10, 2017
Citation: Torrealba Y, Lee H, Passos S, Nassar U, Pedroza J (2017) Mechanical Evaluation of 4 Different Implant Design Systems. Dent Implants Dentures 2:114. doi:10.4172/2572-4835.1000114
Copyright: © 2017 Torrealba Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Dental Science and Medicine
Abstract
Purpose: The aims of this study were to: 1. Compare the fracture strengths of four different implant systems, and 2. Evaluate the failure mode of the implants. Materials and methods: A total of eighty-eight (n=88) screw implants were tested. Forty-four for compressive strength and forty-four were tested for fatigue. Each implant body were inserted into a 30 degree holding device and adapted to be used in the BOSE 3330 Electro Force Testing System. A metal sphere was placed in the contact point of the implants (ISO 14801). The compression load was applied to each specimen at a rate of 0.02 inch per minute until failure. For the fatigue testing the step-stress accelerated testing at 17 Hz with 3 increment stages of 300.000 cycles each was performed. The fracture surface was evaluated by X400 Olympus microscopy. Discussion: The failure of the Integrity Tapered Implants -1 and -2 piece abutment connection was an identical combined bending of the implant-abutment Connection. Conclusion: The Integrity implant-2 pieces implant-abutment connection presented a higher resistance value to lateral compressive loads compared to the others implant-abutment connections.
Keywords
Compression; Fatigue; Fracture
Introduction
Dental implants are an important tool in restorative dentistry for edentulous and partially edentulous patients. Having a 90 to 95% initial success rate, implants are considered to be a viable solution for many cases. However, implants can fail and fracture, posing a major problem for both the patient and the clinician 1. Some clinical observations of these failures have suggested that the major causes are: incomplete osseointegration, complications of the peri-implant soft tissue, and biomechanical problems [1,2].
In the biomechanical problems several implant-abutment interface failures are associated with engineering design and can be assessed in the laboratory setting 3. These interface designs are classified as either external or internal connections [3,4]. The external hexagon connection was initially intended as a method to facilitate implant insertion during surgery. However, there drawbacks with the exposure of the implantabutment interface and abutment screw to greater external loads and are some bending moments, which can lead to screw loosening or fatigue fracture [3]. The internal connections have been developed to help decrease the mechanical issues that arose with the external connections [4]. However, Gil et al. [5] found that the fatigue behavior of the external hexagon interface proved to be superior in comparison to the internal hexagon interfaces.
Other common mechanical issue that have been observed in both connections include screw loosening and/or screw fracture [6]. Loosening of screws can be caused by: (1) insufficient tightening, (2) poorly machined parts, (3) overloading, (4) screw design, or (5) elasticity of bone. When the applied load is larger than the yield strength of the implant bending can occur contributing to the loosening of the screws. Furthermore, failures of implants can be attributed to fatigue, which can be defined as the progressive crack propagation resulting in a fracture under repeated or fluctuating strains below the yield stress [7]. Steinebrunner et al. [8] compared the fracture strengths of 6 different implant systems. They observed differences in the fracture strength of the tested implant systems, identifying systems with increasing joint lengths to have better fracture strengths.
Cyclic loading forces that do not exceed the maximum strength of an implant connection might result in the gradual loosening of the implant–abutment connection or the sudden failure due to fatigue. The reason for the fatigue failure is either a lack of force fitting or formclosure of the connection design [9].
A comparison of the different implant-abutment designs and their strengths would give the clinician an idea of when to use the implants to their optimum potential in different situations. There is nothing in the literature comparing the mechanical behavior evaluation of these particular implants, except for UnipostTM. Therefore, the aims of this study were twofold: to investigate and compare the mechanical behavior (compressive and fatigue) of four different Tatum implant design systems using the accelerated lifetime test; as well as to determine the failure mode for each system.
Materials and Methods
A total of eighty-eight screw implants were used for compressive (n=44) and fatigue (n=44) testing, as follows (Table 1):
| Implant Type | Dimensions | Number of Implants | Total |
|---|---|---|---|
| Integrity Tapered with -1 piece abutment connection | 3.5-mm D x 13-mm L | Static=11 Fatigue=11 |
n=22 |
| Integrity Tapered with -2 pieces abutment connection | 3.5-mm D x 13-mm L | Static=11 Fatigue=11 |
n=22 |
| “T” Tapered Implant with Unipost™ Abutment System | 3.5-mm D x 13-mm L | Static=11 Fatigue=11 |
n=22 |
| ITO (One-piece Tapered Implants) | 3.5-mm D x 13-mm L | Static=11 Fatigue=11 |
n=22 |
| n=88 |
Table 1: Screw implants for compressive (n=44) and fatigue (n=44) testing.
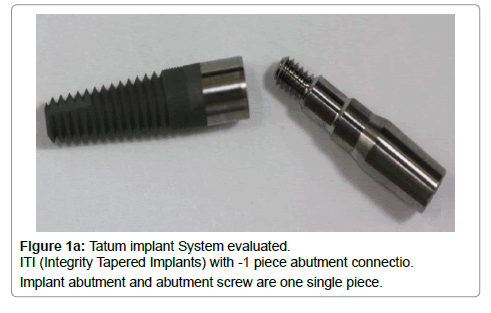
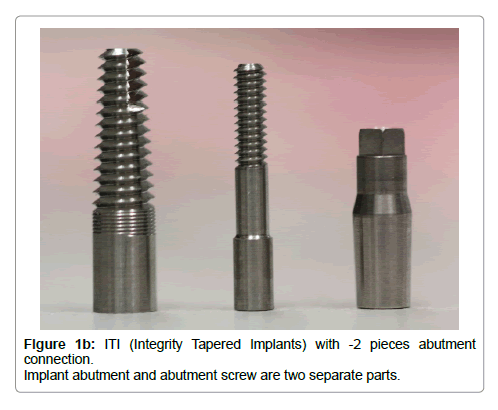
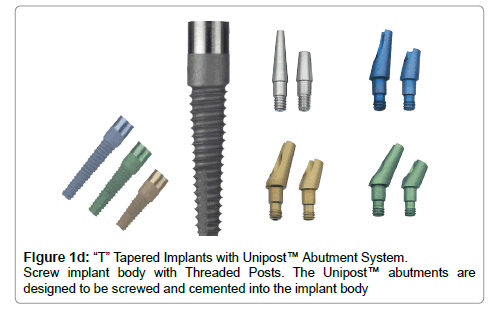
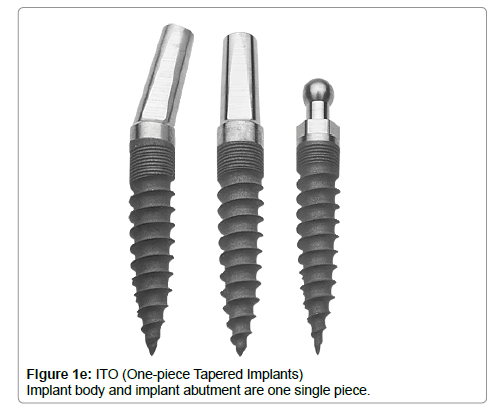
All samples were provided by the manufacturers Suncoast Dental, Inc from production inventory and were from the same batch # 57689 Lot 38. All implant systems were used with their respectively prefabricated straight abutment and abutment screw, except for the ITO (One-piece Tapered Implants) since this one is fabricated as a single piece, implant and abutment together (Figure 1). The testing and measurements were made at the Zimetrix private testing laboratory of the University of Calgary, Calgary, Alberta, Canada.
Implant preparation
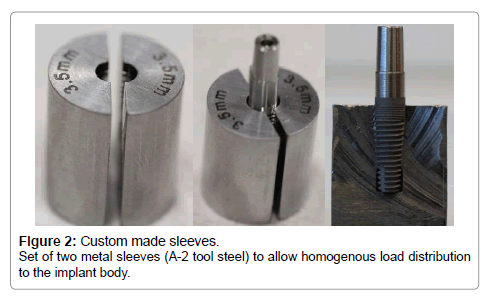
One set of two 20 mm long metal sleeves (A-2 tool steel) was fabricated for each implant system (University of Alberta, Edmonton, Canada) - (Approved by the FDA), 1996 (Figure 2). These sleeves allowed homogenous load distribution to the implant body. Following the ISO 14801:2007 standard protocol, the sleeves were placed 3 mm ± 0.5 mm apically from the nominal bone level as specified in the manufacturer’s instructions for use. This distance was chosen to provide a representative case with respect of bone loss. Each straight pre-fabricated abutment was cut on top to obtain the same dimensions for all specimens (Hardinge Super-Precision Machine). The distance from the top of the sleeves to the top of the abutments was 11 mm ± 0.5 mm, which represented the moment arm.
Application of the controlled torque
Integrity Tapered Implants with -1 piece abutment connection and Integrity Tapered Implants with -2 pieces abutment connection, were rigidly held to avoid rotation in a special holding device during abutment screw tightening to 35 Ncm with a Digital Torque Gauge (Model BGI, Mark 10, LD No. 9094). Following the manufacturer’s protocol; after 10 minutes, implants were re-torqued to 35 Ncm. The Unipost™ Abutment System samples were screwed and cemented to the “T” Tapered Implants with Resiment Cement. Resiment is a multipurpose permanent BIS-GMA resin self-cure radiopaque cement recommended for final cementation. Manufacturer’s instructions were followed during this procedure. No procedure was performed for the ITO (One-piece Tapered Implants) samples since they are fabricated in a single piece (implant-abutment together).
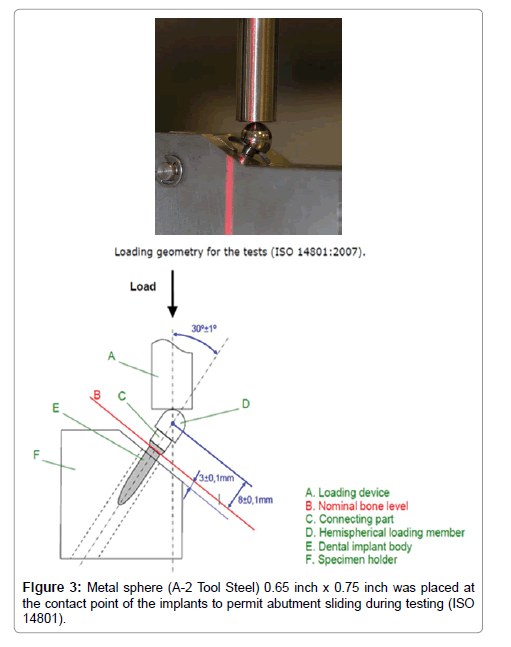
Alignment of implants in the holding device
Each implant body with their respective sleeves was inserted into a Rigid-rigid 30 degree specimen holder device and adapted to be used in the BOSE 3330 ElectroForce Test System (Zimetrix Laboratory, Calgary - Canada). A hemispherical loading member (A-2 Tool Steel) 8 mm x 7 mm was placed on top of the abutment of the implants to represent the loading centre, such that the moment arm can be measured and calculated. (ISO 14801:2007) – (Figure 3).
Testing
Compressive testing: the individual specimens were placed with their respective sleeves in a Rigid-rigid 30 degree fixture. A testing machine BOSE 3330 ElectroForce Test System was used to apply a static compressive load. A computer monitored the applied force continuously (Software Test Ware SX). The compression load was applied to each angulated specimen by an unidirectional vertical platform and loaded with compression at a rate of 0.02 inch per minute until failure. Failure was defined as a fracture of the implant body or the implant-abutment interface [10].
The maximum single impact loaded to failure (N) and the maximum elasticity was computer recorded and a force versus displacement curve for each sample was produced. All implants were examined macro and microscopically.
Fatigue testing: the individual specimens were placed with their respective sleeves on a Rigid-rigid 30 degree fixture. The BOSE 3330 ElectroForce Test System was used to apply the step-stress accelerated testing at 15 Hz of fatigue load with 3 increment stages of 300.000 cycles each. A computer monitored the applied force continuously (Software Test Ware SX). The fatigue load was applied to each angulated specimen by a unidirectional vertical platform and loaded with fatigue forces of 10% (stage 1) of the UTS previously obtained. This was followed by stage 2 with 20% of the UTS, and stage 3 with 40% of the UTS (Table 2). All implants were examined macro and microscopically after the corresponding compressive and fatigue testing.
| Implant System | Maximum Elasticity Mean | Stage 1 (10 %) | Stage 2 (20%) | Stage 3(40%) |
|---|---|---|---|---|
| ITI-2 piece abutment connection | 2160N | 216N | 432N | 864N |
| ITI-1 piece abutment connection | 1850N | 185N | 370N | 740N |
| ITO (One-piece Tapered Implants) | 1398.5N | 139.8N | 279.6N | 559.2N |
| Unipost™ implants System | 1148.7N | 114.8N | 229.6N | 459.2N |
Table 2: Vertical load for Stages 1, 2 and 3 during the fatigue test.
Statistical analysis
The outcome variables tested were compressive and fatigue strength; the independent variable was the implant-abutment systems. For the compressive strength and fatigue resistance evaluation, forty-four (44) implants units were tested for each, eleven implants per system (n=11). The null hypothesis was that there was no significant difference in the compressive testing among the different implant systems. A post-hoc Tukey test and an analysis of variance were used to compare means for significant difference between groups.
Results
Compressive testing results
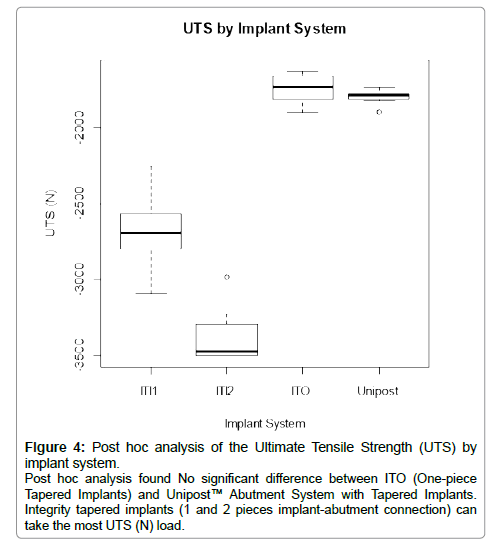
An analysis of variance on the compression test results suggested that the Integrity Tapered Implants -2 pieces implant-abutment connection presented a statistically different value to lateral and oblique compressive loads (F(3,40)=307.20, p<0.001).
The mean maximum UTS (Ultimate tensile strength) of Integrity Tapered Implants -2 pieces implant-abutment connection was 3500.2 N, compared to a mean of 3090.6 N for Integrity Tapered Implants -1 piece implant-abutment connection, 1898.4N for ITO-one piece tapered implant, and 1892.9 N for Unipost™ Screw implants. Post-hoc Tukey test showed that the Integrity Tapered Implants-2 pieces was significantly different compared to the other groups (Figure 4).
Figure 4: Post hoc analysis of the Ultimate Tensile Strength (UTS) by implant system. Post hoc analysis found No significant difference between ITO (One-piece Tapered Implants) and Unipost™ Abutment System with Tapered Implants. Integrity tapered implants (1 and 2 pieces implant-abutment connection) can take the most UTS (N) load.
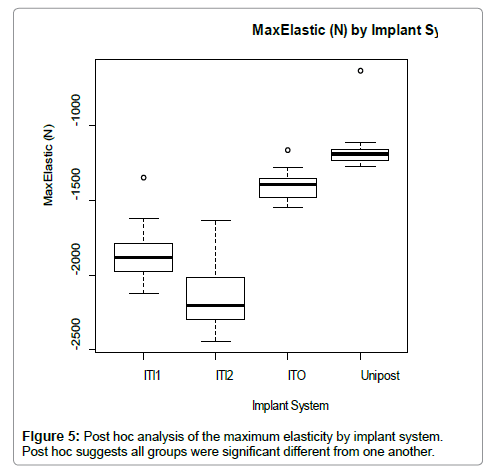
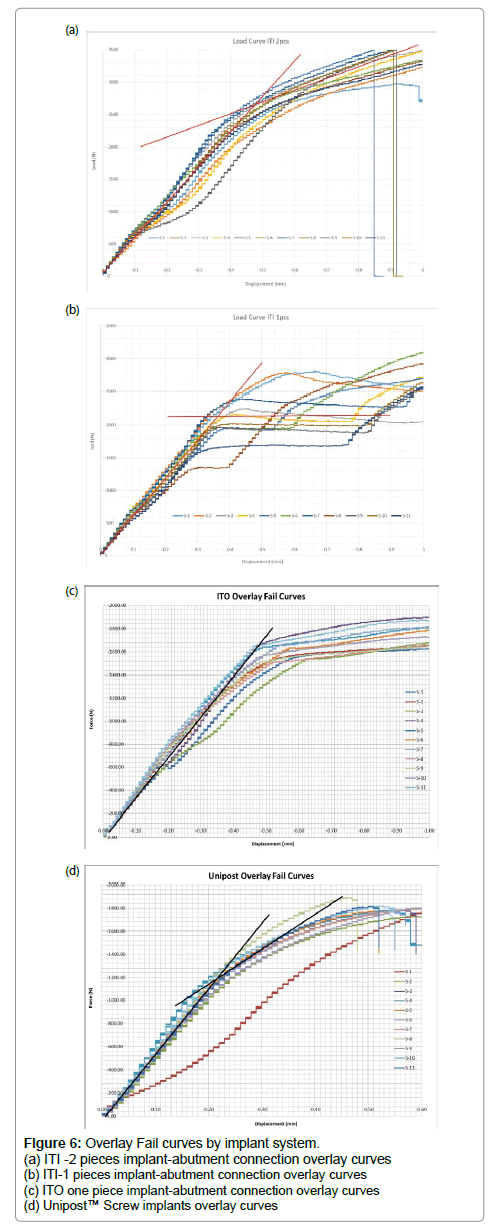
Maximum Elasticity (n) was significantly different across all groups. Integrity Tapered Implants -2 piece implant-abutment connections presented a higher elasticity with an average of 2160 N, and Unipost™ Screw implants showed the lowest elasticity with an average of 1148.7N. (Figure 5) The Overlay fail curves by implant system showing the UTS and maximum elasticity is presented in (Figure 6).
Fatigue testing results
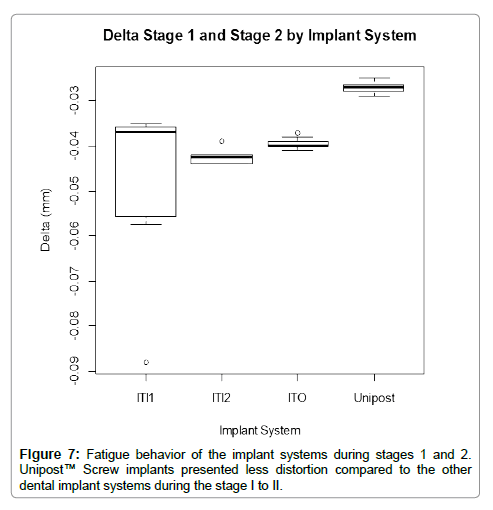
No failure was observed during stages 1 and 2 of the fatigue testing, which represent 10% and 20% of the maximum elasticity average (Table 1). However, Unipost™ Screw implants were significantly different from all other groups between stages 1 and 2, displaying less distortion and more rigidity during the stage 1 to 2 (Figure 7). An analysis of variance on the compression test results suggested that there was no difference between ITO-one piece tapered implant and Integrity Tapered Implants -1 and -2 piece implant-abutment connection (F(3,32)=6.68,p=001).
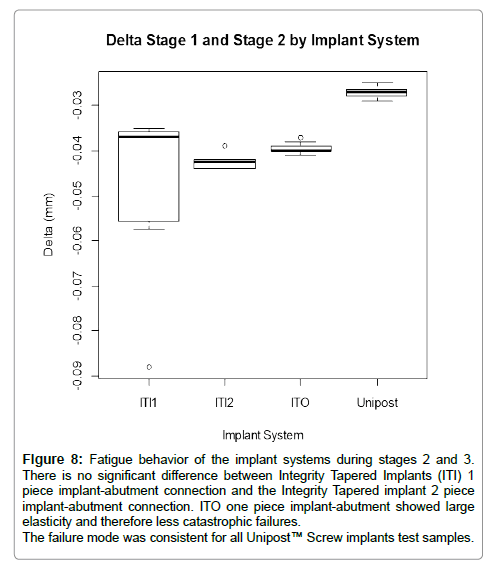
In the stages 2 and 3 there was no significant difference between Integrity Tapered Implants -1 and -2 piece implant-abutment connection, however the other groups Unipost™ Screw implants and ITO one piece implant-abutment connection were different from one another. ITO one piece implant-abutment showed large elasticity and therefore less catastrophic failures compared to the Unipost™ Screw implants (Figure 8).
Figure 8: Fatigue behavior of the implant systems during stages 2 and 3. There is no significant difference between Integrity Tapered Implants (ITI) 1 piece implant-abutment connection and the Integrity Tapered implant 2 piece implant-abutment connection. ITO one piece implant-abutment showed large elasticity and therefore less catastrophic failures. The failure mode was consistent for all Unipost™ Screw implants test samples.
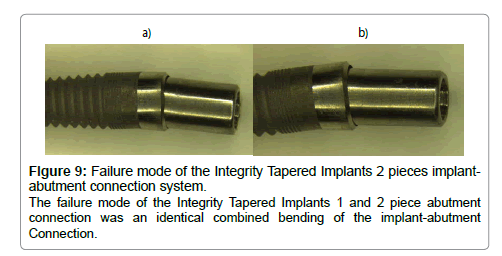
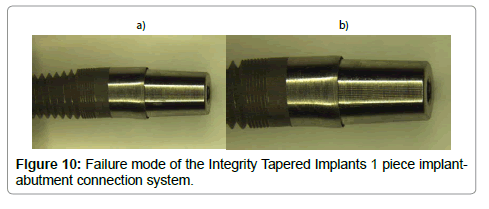
In the failure mode evaluation (under microscope), an identical combined bending of the implant-abutment connection and screw was observed for the Integrity Tapered Implants -1 and -2 piece abutment connections (Figures 9 and 10).
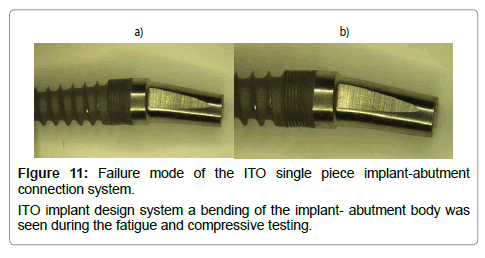
ITO one piece implant-abutment connection presented a bending of the abutment zone (Figure 11).
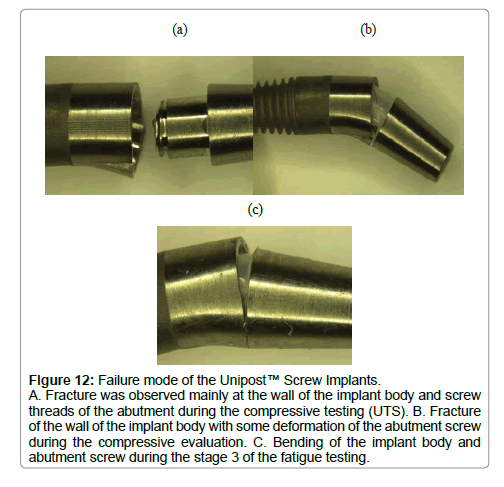
The failure mode was consistent for all Unipost™ Screw implants test samples. Fracture was observed on the wall of the implant body with some deformation or fracture of the abutment screws (Figure 12).
Figure 12:Failure mode of the Unipost™ Screw Implants. A. Fracture was observed mainly at the wall of the implant body and screw threads of the abutment during the compressive testing (UTS). B. Fracture of the wall of the implant body with some deformation of the abutment screw during the compressive evaluation. C. Bending of the implant body and abutment screw during the stage 3 of the fatigue testing.
Discussion
One of the limitations of this research is the selection of 4 different implant of the same company but at the same time all of these implant has different internal connections that provide a wide evaluation and expectation for the clinician. The main reason of this selection is the use of these implants in our graduate program. After obtaining all these results, the comparison with other implants system is our goal since clinical observations have suggested that a major cause of implant failure is screw joint instability, which includes loosening or fracturing of the abutments and screws. Loosening and fracturing are potential problems for all types of implant abutments and their screws [11]. These problems generally arise from the design of the screw, the implant-abutment interface, the distribution of the occlusal load to the osseointegrated implants, and/or the design of the implant body [8]. Mechanical failures can be decreased by increasing the implant diameter and modifying the screw joint design [3,8,12]. The screw shape of the implant body provides a large contact area between implant and bone, which increases stability, reduces the shear stress in the bone-implant interface, reduces the stress concentration in the cervical region, and relieves stress concentration [3,6,9]. Increasing the surface area of the implant improves the distribution of forces to the bone; for this reason, various shapes of implants were developed to increase stability [11].
The screw joint preload is one of the most important factors that reduce and prevent screw loosening [9]. All Tatum’s abutment screw was preloaded with 35 N. When a screw is tightened, a tensile force (preload) is concentrated in the stem of the screw and acts from the screw’s head to the threads (the weaker point) [3,6,13,14]. The preload should be as high as possible to maximize the contact force between the abutment and the implant, always following the manufacturer instructions. The manufacturer always determines the optimal torque and preload values [3,14]. The higher the preload, the higher the torque, which decreases the risk of screw loosening [3,6].
The implant-abutment interface requires adequate mechanical characteristics to resist the functional occlusal loads and minimize failures [4]. In this study the fatigue occlusal load was simulated at 3 different stages using 10%, 20%, and 40% of the previous determined ultimate tensile strength for 300.000 cycles each. These steps simulate the biting performance of the mandible for certain period of time varying from less to high forces of mastication. Fatigue simulating occlusal function at loads below the ultimate tensile strength may contribute in the gradual loosening and failure of the screw [15]. The in-vitro static and fatigue studies provide the clinicians with an idea of how implant systems perform simulating natural forces [12,13]. One of the limitations of this study is the comparison of 4 different implant design system from one company.
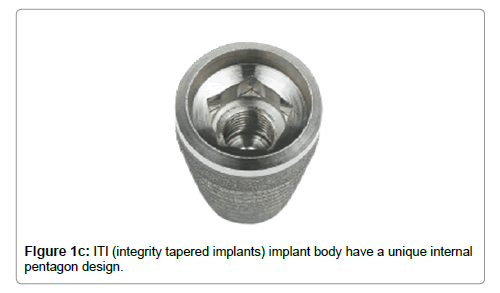
All implants were set and prepared following the ISO 14081:2007 standard protocol. The mean UTS of the Integrity Tapered Implants -2 piece implant-abutment connection is 3500.2N, suggesting that this implant abutment system is the strongest out of the four tested in the study. The strength of this implant may be due to the internal design [16-18], which allows the large retention abutment screws of 2.0 mm and 2.5 mm, to be screwed until the middle or apical third of the implant abutment. This characteristic may increase the fracture strength of the implant system. The Integrity Tapered Implants – 1 piece implant-abutment system had a mean UTS of 3090.6 N. The high UTS value of both Integrity Tapered Implants systems could be attributed to a higher resistance to lateral loads due to the lower center of rotation and better force distribution within the system. These implant systems have a unique pentagon internal abutment connection, which could have reduced the abutment-screw load on the system, resulting in more stabilility [17,19].
The mean UTS of the ITO one-piece implant abutment were 1892.9N. It is important to mention that during the static (compression) testing of these implants, they remained in the plastic strain zone longer than the other systems before the final failure occurred. Therefore, the ductile curve is far superior to the other systems, which means that ITO implant systems absorbed the energy better than the Integrity Tapered Implants and Unipost™. There was no gap between the implant and the abutment in the one piece tapered design; this design also eliminated the micro-movement of the abutment screw [5].
The null hypothesis could not be accepted because there was a statistical difference in fatigue between the Unipost™ screw implant and Integrity Tapered Implants implant designs. The Unipost™ screw implants had the lowest mean UTS value of 1892.9N compared to the other implant systems evaluated in this study. The brittle curve is higher and the ductile curve is lower. One reason for these findings could be due to a progressive vertical interlocking of the tapered connective elements under loading conditions, after definite seating and cementation of the abutment [3]. Unlike the Integrity Tapered Implants, the Unipost™ abutment is cemented and screwed to the implant body counterclockwise to avoid loosening the abutment during its preparation in the mouth. This may lead to minimal change of the vertical dimension between the abutment and the implant, resulting in a loss of screw tension at the connection [3]. When compared to the posterior natural dentition, these implants demonstrated excellent resistance to lateral loads. This may be attributed primarily to the diameter of the abutment screw with its 2.5-mm counter bore and the union with the abutment, representing a unique piece [3].
The failure mode of the Integrity Tapered Implants -1 and -2 piece abutment connections was an identical combined bending of the implant-abutment Connection. For the Unipost™ screw implant the failure was mainly at the wall of the implant body and screw of the abutment during the compressive testing (UTS). For the ITO implant design system a bending of the implant- abutment body was seen during the fatigue and compressive testing.
Conclusions
Within the limitations of this in-vitro study, the following conclusions were drawn:
- In General:
1. All implant systems failed far above the chewing forces of the human masticatory forces.
2. The performance of the Integrity Tapered Implants with -2 pieces abutment connection was superior to the other Tatum’s systems in terms of fracture strength and failure mode.
- Static or Compressive testing:
1. Integrity Tapered Implants -2 pieces abutment connection and Integrity Tapered Implants -1 piece abutment connection systems can take the most UTS (n), compared to the other studied systems.
2. There was no significant difference between ITO one-piece implant-abutment connection system and Unipost™ Screw implant system.
3. Maximum Elasticity was significantly different across all groups.
4. Post hoc analysis suggested that all groups were significantly different from one another.
- Fatigue testing:
1. Unipost™ Screw implant system was significantly different from all other groups between stages 1 and 2.
2. During the fatigue testing there was not difference between ITO one piece implant-abutment connection system and the Integrity Tapered Implants -2 and -1 piece implant-abutment connection systems.
3. Between stage 2 and 3, there was no significant difference between Integrity Tapered Implants -2 and -1 piece implant-abutment connection systems, however Unipost and ITO are different from one another.
Further studies in fractography and true strain of the implants surfaces may provide additional information to assess the clinical significance of the findings obtained in this investigation.
Acknowledgments
The authors thank Hollis Lai, PhD, Director of Evaluation and Assessment, Undergraduate Medical Education; Faculty of Medicine and Dentistry- University of Alberta for his assistance in the statistical analysis of the results. Thanks to Suncoast Dental for the donation of the dental implants to perform this study.
References
- Tagger Green N, Machtei EE, Horowitz J, Peled M (2002) Fracture of Dental Implants: Literature Review and Report of a Case. Implant Dent11: 137-143.
- Huang HM Tsai CM, Chang CC, Lin CT, Lee SY (2005) Evaluation of loading conditions on fatigue-failed implants by fracture surface analysis. Int J Oral Maxillofac Implants 20: 854-859.
- Pedroza JE, Torrealba Y, Elias A, Psoter W (2007) Comparison of the compressive strength of 3 different implant design systems. J Oral Implantology 33: 1-7.
- Albrektsson T (1988) A multicenter report on osseointegrated oral implants. J Prosthet Dent 60: 75-84.
- Gil FJ Herrero-Climent M, Lázaro P, Rios JV (2014) Implant-abutment connections: influence on the design on the micro-gap and their fatigue and fracture behavior of dental implants. J Mater Sci: Mater Med 25: 1825-1830.
- Binon P, Sutter F, Beaty K, Brunski J (1994) The role of screws in implant systems. Int J Oral Maxillofac Implants 9: 48-63.
- Karl M, Kelly JR (2009) Influence of loading frequency on implant failure under cyclic fatigue conditions. Dental Materials 25: 1426-1432.
- Steinebrunner L, Wolfart S, Ludwig K, Kern M (2008) Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Impl Res 19: 1276-1284.
- Quek HC, Tan KB, Nicholls JI (2008) Load Fatigue Performance of Four Implant-Abutment Interface Designs: Effect of Torque Level and Implant System. Int J Oral Maxillofac Implants 23: 253-262.
- Cibirka RM, Nelson SK, Lang BR, Rueggeberg FA (2001) Examination of the implant-abutment interface after fatigue testing. J Prosthet Dent 85: 268-275.
- Papaspyridakos P, Mokti M, Chen CJ, Benic GI, Gallucci GO, et al. (2014) et al. Implant and prosthodontic survival rates with implant fixed complete dental prostheses in the edentulous mandible after at least 5 years: a systematic review. Clin Implant Dent Relat Res 16: 705-717.
- Strub JR, Gerds T (2003) Fracture strength and failure mode of five different single tooth implant abutment combinations. Int J Prosthodont16: 167-171.
- Khraisat A, Stegaroiu R, Nomura S, Miyakawa O (2002) Fatigue resistance of two implant/abutment joint designs. J Prosthet Dent 88: 604-610.
- Riberio CG, Maia MLC, Scherrer SS, Cardoso AC, Wiskott HWA (2011) Resistance of three implant-abutment interfaces to fatigue testing. J Appl Oral Sci 19: 413-420.
- Butignon LE, Basilio MA, Pereira RP, Filho JNA (2013) Influence of Three Types of Abutments on Preload Values Before and After Cyclic Loading with Structural Analysis by Scanning Electron Microscopy. Int J Oral Maxillofac Implant 28: 161-170.
- Martins LM, Bonfante EA, Zavanelli RA, Freitas Jr AC, Silva NRFA (2012) Fatigue Reliability of 3 Single-Unit Implant - Abutment Designs. Implant Dentistry 21: 67-71.
- Binon P (1990) The effect of implant/abutment hexagonal misfit on screw joint stability. Int J Prosthodont 9: 149-160.
- Basten CH (1996) Load fatigue performance of two implant abutment connections. The International Journal of Oral & Maxilofacial Implants 11: 552-528.
- Balfour A, O’Brien GR (1995) Comparative study of anti-rotational single tooth abutments. J Prosthet Dent 73: 36-42.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 6944
- [From(publication date):
December-2016 - Jul 18, 2024] - Breakdown by view type
- HTML page views : 5931
- PDF downloads : 1013