Research Article Open Access
Measuring the Pain of Mucositis using Oucher and DEGR
Richard Hain1*, Meriel Jenney2, Ben Carter3 and Ruth Davies41LATCH Senior Lecturer/Honorary Consultant in Paediatric Palliative Medicine Cardiff University School of Medicine, Cardiff, UK
2Consultant Paediatric Oncologist, Children’s Hospital, Cardiff, UK
3Lecturer in Medical Statistics, University of Birmingham, Birmingham, UK
4Senior Lecturer in Paediatric Nursing, Swansea University, Swansea, UK
- Corresponding Author:
- Richard Hain
MD, Senior Lecturer/Honorary Consultant in Paediatric Palliative Medicine
Department of Child Health
Cardiff School of Medicine, UK
Tel: +44 29 2074 3373
Fax: +44 29 2074 4283
E-mail: HainRD@Cardiff.ac.uk
Received date: May 15, 2015, Accepted date: June 30, 2015, Published date: July 03, 2015
Citation: Hain R, Jenney M, Carter B, Davies R (2015) Measuring the Pain of Mucositis using Oucher and DEGR. J Palliat Care Med 5:222. doi: 10.4172/2165-7386.1000222
Copyright: © 2015 Hain R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Aim: To measure pain in mucositis using two pain scales of contrasting design (DEGR and Oucher), and to compare the two scores.
Patients and methods: Children receiving treatment for pain related to cancer therapy on a regional specialist oncology ward were eligible for the study. Children’s pain was scored in parallel using DEGR administered by the ward nurses and Oucher administered by a research nurse.
Results: Thirty families participated in the study. Pain score data were incomplete for nine. 143 DEGR scores and 92 Oucher scores were obtained. Scores from either scale were discarded if too remote (i.e. >4 hours apart) from their paired score from the other. Forty-six complete sets of paired data were obtained from 21 subjects. Mucositis pain persisted for several days. Oucher scores were significantly and inversely influenced by time while DEGR scores were not, such that scores diverged after three days.
Conclusions: Pain persisted despite intensive treatment. Behaviour patterns associated with persistent pain seemed to become apparent during acute episodes of mucositis. Our data suggest DEGR was more sensitive to persistent pain than the Oucher but patient numbers were small.
Keywords
Mucositis; Oucher scale; Paediatric oncology; DEGR
Introduction
Even today, the pain of mucositis is one of the most unpleasant aspects of treatment for childhood cancer [1,2]. The key to managing it effectively is to match the analgesic dose closely with the reported pain intensity [3,4].
To measure a child’s pain experience in a way that allows this in practice, however, remains a fundamental challenge [5-8]. Physiological responses to pain can be measured [9]. But few are specific to pain; most are mimicked by distress. Furthermore, such measurements take no account of pain’s subjective nature. How pain ‘feels’ to children cannot be objectively assessed. This study uses two different instruments to measure pain, both designed for children. The Oucher scale has been well validated [10-15]. It is an example of a self-report ‘faces’ scale.
Pain that does not remit quickly has been termed ‘persistent pain’ (Collins, JJ, 2010, personal communication) to distinguish it from acute or chronic pain. Children whose pain persists will not protest indefinitely [16], but over time may modify movements to minimise pain, then become accustomed to it [17]. After a period, a child may appear pain-free, but only by avoiding uncomfortable movements or simply becoming resigned to a certain severity of pain [16].
Measuring those adjustments is the basis of the DEGR scale [17-20]. Its authors hypothesise that children demonstrate an adaptive behavioural responseto persistent pain, akin to resignation, which they call ‘psychomotor atonia (PMA). They suggest that quantitating PMA gives an indication of persistence. The DEGR further evaluates a child’s attempts to minimise pain (‘direct signs of pain’ DSP), and verbalisation of severity (‘voluntary expressions of pain’, VEP). By refining subjective VEP scores using PMA and DSP scores, say its authors, the DEGR is able to identify differences in duration between pains giving the same global score [17-20].
The aim of this study was to use and to compare the two scales in measurement of mucositis pain in children with cancer.
Methods
Full ethical consent was obtained from South Wales Local Research Ethics Committee. Patients were eligible for this study if they were between five and 19 years old, under the care of the Welsh regional Paediatric Oncology Team, commencing analgesic therapy other than paracetamol (acetaminophen) prescribed solely as an antipyretic, and expected to require analgesics for more than 24 hours. Patients with neurodevelopmental delay were excluded as manifestations of pain in this group are different [21,22].
Hospital ward staff was trained in use of the DEGR in its definitive form [17-20]. Suitable potential subjects were identified and invited to consent to participate using age-appropriate consent forms and information sheets. Where appropriate, parental consent was also sought. Prescription and modification of analgesia in response to pain scores was according to the ward protocol. Where possible, total daily opioid requirement was recorded.
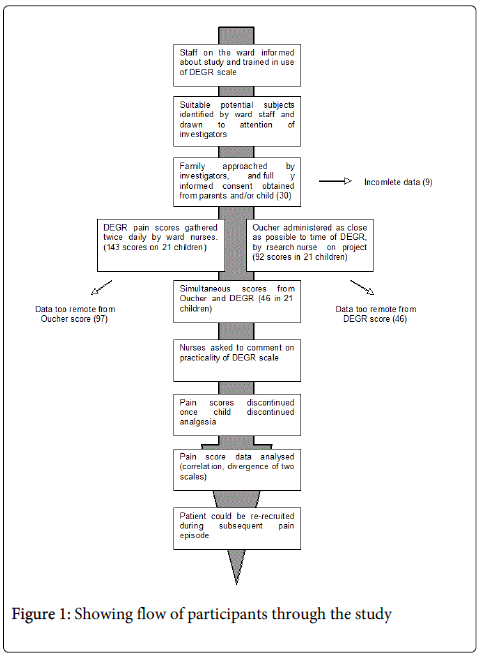
A pain score was obtained twice daily using each of the two scales (Figure 1) as nearly simultaneously as practically possible. Only resting pain was assessed. Data were discarded if the interval between the two scores exceeded four hours (Figure 1). The DEGR is designed to be used, retrospectively at change of shift and was therefore used twice daily for each patient. The Oucher has been developed for use in the research setting and was administered by a research nurse blinded to the DEGR scores, according to the designer’s instructions.
Data analysis: clinical methods comparison
Previous comparisons of the Oucher and another behavioural scale [13] suggest a mean difference of 15%. A clinically significant difference was considered to be 10%. A priori power calculation based on reported standard deviation of 1.5 units for the Oucher and 6.2 for the DEGR (20) suggested between 20 and 50 data points were needed to show significant difference (alpha <0.05, power 0.8). In the event there were 46 sets of data from 21 patients.
Comparison was made between the Oucher scores and those of the DEGR in each of the three domains separately and globally. Individual patient profile plots are presented to show the average change in pain scores over time. The agreement and association between the two scales are presented using two plots: a scatterplot partitioned into acute pain (captured on days 1, 2 or 3), and persistent pain captured on day 4 and later. The two scales were compared using the Bland and Altman method [23].
The effects of time on the pain score was analysed for both scales. A poisson generalized regression methodology was used with a log link to model the pain count scores independently for the two instruments, fitted with the R software [24].
Results
Patients
Thirty families agreed to participate in the study and were recruited at the Welsh Regional Paediatric Oncology Centre, now based at the Children’s Hospital in Cardiff (Figure 1). Forty-six complete pain score measurements were collected from 21 patients (Figure 1). The median age was 12.0 years (range 3.9-19.7 years), 9 were male and 12 were female. Participants spent between one and 15 days in the study (Table 1).
| Numbers of days in the study | Number of patients |
|---|---|
| 1 | 13 |
| 2 | 1 |
| 3 | 1 |
| 8 | 3 |
| 14 | 1 |
| 15 | 2 |
Table 1: Showing number of days spent by each of the subjects in the study.
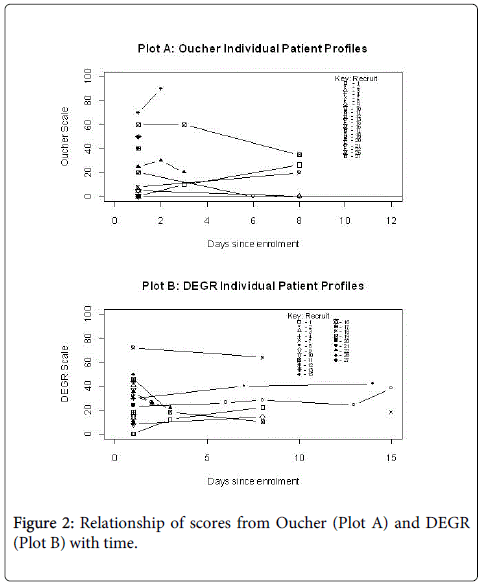
The individual patient profile plots present the pain scores for the two scales (Figure 2, plots A and B). Figure 2, Plot A presents the individual profiles for patients outcomes of the Oucher scale. Figure 2, Plot B presents the individual profile plots for the same patients reporting the DEGR outcome. Within the Oucher scores, but not the DEGR, there is a change over time from enrolment (p<0.05).
Agreement between Oucher and DEGR
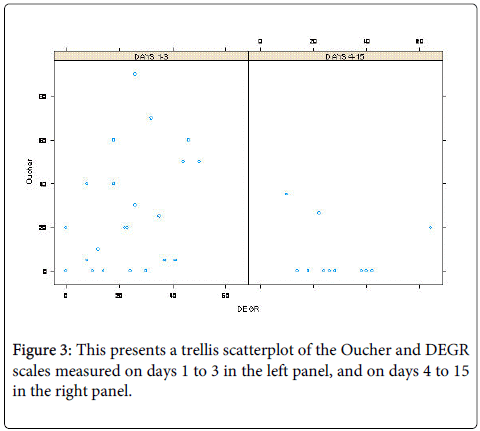
A comparison between the two scales (Figure 3), is shown as a scatterplot. The data suggest that for the first three days after enrolment (left panel), patient scores from the two instruments are moderately associated but that this association is less clear between four and 15 days (right hand panel).
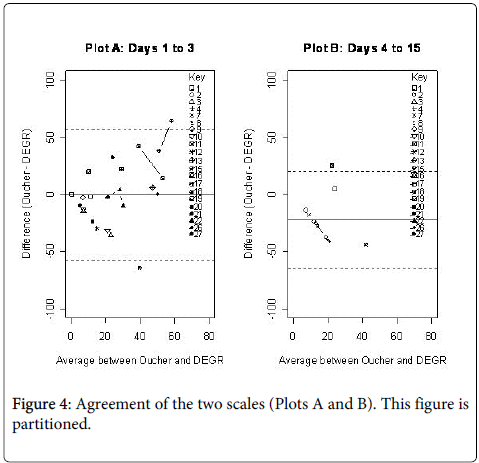
Figure 4, plots A and B present the Bland-Altman plots of agreement that comparing average of Oucher and global DEGR scores against difference between the scores. There is good agreement between the two scales during the lower pain scores. Towards higher scores there appears to be a systematic bias, such that at higher scores the Oucher tends to over-read relative to the DEGR. This bias is introduced from the patient, rather than the instrument, since patients consistently score one scale greater than the other. The same pattern was seen in all three domains of the DEGR scores (data not shown), but was least marked in VEP. The Bland-Altman plot shows difference between the scores (Oucher-DEGR) on the y-axis and average of the scores (surrogate for the ‘true’ score) on the x-axis. Plot A (left) presents observations collected on days 1 to 3, and Plot B presents days 4 to 15. The agreement between the two is good, but there is evidence of systematic bias at the higher scores, with a tendency for the Oucher to read higher than the DEGR. While timing of the scores has little influence, Poisson regression suggests there may be participant bias.
A generalised Poisson regression model was fitted using both count scores to determine the effect of time and recruit on the outcome measure, using a log-link and scaled by the deviance.
The poisson regression model fitted using the Oucher indicates that scores from the Oucher are significantly influenced by the individual (p<0.01) and by the day of measurement (p=0.016; mean slope -0.049 and 95% CI [-0.087, -0.009]). In contrast, using the DEGR, the model indicates that although scores were influenced by the individual (p<0.01), they were not significantly influenced by day (p=0.29; mean slope 0.011 and 95% CI [-0.009, 0.031]).
Changes over time
Over the course of the study, scores using the Oucher fell with time (Figure 3, p<0.05). Using the DEGR, however, there was no such fall (Figure 3) whilst the child continued to require analgesia. Of eight individual patients with more than one pair of scores, six showed a decline in scores using the Oucher (Figure 2). Using the DEGR over the same period, five patients indicated either little change or even an increase in their score (Figure 2). This included both patients who provided scores into a second week.
Discussion
Children remained in significant pain for several days after analgesia was commenced (Figures 2-4). Opioid requirements remained above 1 mg/kg/24 hrs OME (oral morphine equivalent) for several days (Table 2).
| Recruit no. | Day no. | Analgesia (OME mg/kg/24h) |
|---|---|---|
| 1 | 1 | 2.4 |
| 3 | 1.8 | |
| 7 | 1.8 | |
| 2 | 1 | 3.2 |
| 5 | 4.4 | |
| 12 | 0.7 | |
| 14 | 0.4 | |
| 3 | 1 | 1.6 |
| 4 | 1 | 1.8 |
| 7 | 13 | 0.1 |
Table 2: Showing analgesic requirements (OME = oral morphine equivalence)
When comparing two clinical measurement tools, a common error is to use correlation techniques rather than those, such as the Bland-Altman method, that measure agreement [23]. An earlier comparison of the Oucher with another behavioural scale [13] demonstrated poor correlation between them overall, but agreement, particularly at lower scores, was good.
Agreement between the two scales in this study was also good, though there was systematic bias at higher scores, with the DEGR over-reading compared with the Oucher. Analysis of the data shows that both scores are influenced significantly by the individual reporting it; in other words, one child will tend to score more highly than another, irrespective of which scale is used. This is not an unexpected finding.
Strikingly, scores from the Oucher were independently influenced by how long the measurement was taken after enrolment into the study, with scores tending to decline over time after enrolment. This influence was not seen with the DEGR, indicating that the DEGR remains sensitive to pain for longer than the Oucher, and this is supported by the profiles of scores from individual patients (Figure 2) in whom opioid requirements remained significant for some days (Table 2). This would seem to support its authors’ hypothesis that the DEGR scale is able to measure persistent pain.
The point at which the two scores diverge in our study gives an indication of the time taken for acute pain responses to give way to more adaptive ones in children. Pain that does not remit is associated in adults with the emergence of psychological adaptations, including depression [25-27], which closely resemble the syndrome of PMA described by the designers of the DEGR [17-20]. The point at which the child accommodates and become resigned to it is therefore when the two scores diverged. In our study, this appeared to be after only three days (Figure 3).
This is significant in clinical practice. Episodes of mucositis pain requiring inpatient management with major opioids usually exceed three days. Our study suggests that conventional ‘faces’ type pain scales may underestimate it beyond the first few days after admission.
It is important to recognise, however that the number of patients in this study is small and this should mean caution in interpreting its conclusions definitively. Although the number of data points was reasonable, the number of individual patients from whom they came was only just adequate according to our power calculations. As would be expected, this paucity of data was most marked at later time points (Figure 2), so that although our results regarding persistent pain are suggestive, they are far from conclusive. It would be important to confirm these findings in a larger study. This should include many patients’ scores over the whole study period, and particularly over the cusp we have identified at three days.
Furthermore, there are alternative explanations for the observed divergence of the scores. The DEGR has been validated in children between two and six years old and, although in principle it seems plausible that it would be valid in the wider range of ages in our study, patient numbers were too small for us to demonstrate this.
It is also possible that the DEGR measures a phenomenon other than pain. Low mood or depression could, by the nature of the DEGR, plausibly confound the results. The persisting use of analgesics by patients in the study (Table 2) suggests, however, that patients themselves interpreted their experience as pain.
More likely is that there might be a difference in consistent application of the two tools. Both scales rely for their validity on accurate application by appropriately trained personnel. In our study, the Oucher was applied by a single researcher familiar with its use. The DEGR was applied, as its designers intended, by nurses working shifts on the ward. Although all had received training, it is likely the Oucher was applied with greater consistency.
In conclusion, our study has shown that mucositis pain remains a significant problem, despite intensive attention to assessing and treating it. Measured using two scales of fundamentally differing design, pain persisted for some days. There was reasonable agreement between the scales at lower scores and both scores were influenced by the individual being assessed.
Oucher scores, but not DEGR scores, fell over time. The two scores diverged after around three days. Taken together, these observations support the hypothesis that, as its authors intended, the DEGR is more sensitive to persistent pain than the Oucher.
Our study suggests that behaviour patterns that have been associated with persistent pain in children begin to become apparent after only three days of mucositis pain. The validity of using scales designed primarily to assess acute pain should be addressed in future studies.
References
- . Tomlinson D, Gibson F, Treister N, Baggott C, Judd P, et al. (2009) Designing an oral mucositis assessment instrument for use in children: generating items using a nominal group technique. Support Care Cancer 17(5):555-562.
- Cheng KK. (2009) Oral mucositis: a phenomenological study of pediatric patients' and their parents' perspectives and experiences. Support Care Cancer 17:829-837.
- Kennedy L, Diamond J (1999) Assessment and management of chemotherapy-induced mucositis in children. J PediatrOncolNurs 14: 164-174.
- Collins JJ, Geake J, Grier HE, Houck CS, Thaler HT, et al. (1996) Patient-controlled analgesia for mucositis pain in children: a three-period crossover study comparing morphine and hydromorphone. J Pediatr 129:722-728.
- Franck LS, Greenberg CS, Stevens B (2000) Pain assessment in infants and children. PediatrClin North Am 47: 487-512.
- Hain RD (1997) Pain scales in children: a review. Palliat Med Sep 11: 341-350.
- Ramelet AS, Abu-Saad HH, Rees N, McDonald S (2004) The challenges of pain measurement in critically ill young children: a comprehensive review. AustCrit Care 17: 33-45.
- Von Baeyer CL (2006) Children's self-reports of pain intensity: scale selection, limitations and interpretation. Pain Res Manag 11: 157-162.
- Von Baeyer CL, Spagrud LJ (2007) Systematic review of observational (behavioral) measures of pain for children and adolescents aged 3 to 18 years. Pain 127: 140-150.
- Beyer JE (2000) Judging the effectiveness of analgesia for children and adolescents during vaso-occlusive events of sickle cell disease. J Pain Symptom Manage. 19(1):63-72.
- Beyer JE, Denyes MJ, Villarruel AM (1992) The creation, validation, and continuing development of the Oucher: a measure of pain intensity in children. J PediatrNurs. 7:335-346.
- Beyer JE, Knott CB (1998) Construct validity estimation for the African-American and Hispanic versions of the Oucher Scale. J PediatrNurs 13:20-31.
- Beyer JE, McGrath PJ, Berde CB (1990) Discordance between self-report and behavioural pain measures in children aged 3-7 years after surgery. J Pain Symptom Manage 5:350-356.
- Beyer JE, Turner SB, Jones L, Young L, Onikul R, et al. (2006) The alternate forms reliability of the Oucher pain scale. Pain ManagNurs 6:10-17.
- Luffy R, Grove SK (2003) Examining the validity, reliability, and preference of three pediatric pain measurement tools in African-American children. PediatrNurs. 29:54-59.
- http://www.ampainsoc.org/advocacy/pediatric.htm
- Gauvain-Piquard A, Rodary C, Lemerle J (1988) L'atoniepsychomotrice: signemajeur de douleur chez l'enfant de moins de 6 ans. Journeesparisiennes de pediatrie249-252.
- Gauvain-Piquard A, Rodary C, Lemerle J (1991)UneEchelled'evaluation de la douleur du jeune enfant: l'echelle DEGR. Journeesparisiennes de pediatrie95-100.
- Gauvain-Piquard A, Rodary C, Rezvani A, Lemerle J (1987) Pain in children aged 2-6 years: a new observational rating scale elaborated in a pediatric oncology unit--preliminary report. Pain 31:177-188.
- Gauvain-Piquard A, Rodary C, Rezvani A, Serbouti S (1999) The development of the DEGR(R): A scale to assess pain in young children with cancer. Eur J Pain 3:165-176.
- Hunt A, Goldman A, Seers K, Crichton N, Mastroyannopoulou K, et al. (2004) Clinical validation of the paediatric pain profile. Dev Med Child Neurol 46:9-18.
- Hunt A, Wisbeach A, Seers K, Goldman A, Crichton N, et al. (2007) Development of the paediatric pain profile: role of video analysis and saliva cortisol in validating a tool to assess pain in children with severe neurological disability. J Pain Symptom Manage 33:276-289.
- Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307-310.
- www.R-project.org.
- Buskila D, Cohen H (2007) Comorbidity of fibromyalgia and psychiatric disorders. Curr Pain Headache Rep 11:333-338.
- Fietta P, Fietta P, Manganelli P (2007) Fibromyalgia and psychiatric disorders. Acta Biomed 78:88-95.
- Weiner DK (2007) Office management of chronic pain in the elderly. Am J Med 120:306-315.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 16341
- [From(publication date):
July-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 11907
- PDF downloads : 4434