Research Article Open Access
Measuring Paramedics’ Understanding of and Attitude towards Chronic Diabetes Care: A Bridge to Community Health
Joseph L. McTernan1* and Eric Matthews21Doctor of Health Sciences Program, College of Graduate Health Studies, A.T. Still University, USA
2College of Graduate Health Studies, A.T. Still University, USA
- *Corresponding Author:
- Joseph L. McTernan
Doctoral Candidate
Doctor of Health Sciences Program
College of Graduate Health Studies
A.T. Still University, USA
Tel: +845 652 0734
E-mail: jmcternan@ATSU.edu
Received date: December 07, 2014; Accepted date: January 13, 2015; Published date: Januray 16, 2015
Citation: McTernan JL, Matthews E (2015) Measuring Paramedics’ Understanding of and Attitude towards Chronic Diabetes Care: A Bridge to Community Health. J Community Med Health Educ 5:328. doi: 10.4172/2161-0711.1000328
Copyright: © 2015 McTernan JL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Objective: Chronic diabetic patients need innovative, cost-effective care. Paramedics are providers whose roles are being reviewed to include non-emergent interaction in the chronic disease population. Our research studies includes the potential for paramedics to interact with the diabetic population in the United States with the goal of cost-effective care and improved clinical outcomes through patient education with a focus on self-management and establish a baseline understanding of paramedics’ current knowledge of and attitude toward current chronic diabetes care. Methods: A two-part electronic survey determining paramedics’ knowledge (DKT) and attitude (DAS-3) toward chronic diabetes was completed by 120 participants, of whom 73 met the inclusion criteria. Results: The majority of paramedics (79.4%, n=58) were able to answer 70% of the DKT knowledge survey questions correctly. Stronger scores on the DKT were not associated with length of time as a paramedic, age, sex, education level, having a close friend or relative with diabetes, or any of the DAS-3 components. The DAS-3 results revealed paramedics had a positive attitude about patients with diabetes and their ability to self-manage their disease. Conclusions: The research has shown that baseline paramedic understanding and attitude has the potential to expand the paramedic’s scope of service within the chronic diabetic population. Further research is needed to determine if paramedic chronic diabetes intervention programs would affect patient outcomes.
Keywords
Paramedic; Chronic diabetes care; Community paramedic; Community health
Introduction
According to the Centres for Disease Control and Prevention [1], diabetes prevalence and incidence have risen, and the disease is the seventh leading cause of death in the United States. Currently, there are an estimated 25.8 million Americans who have diabetes, of whom seven million are undiagnosed [1]. Projections estimate diabetes will increase from current levels of eight cases per 1,000 in 2008 to approximately 15 cases per 1,000 in 2050. There are estimates that prevalence will increase from 14% to 21-33% [2] during that same period. Additionally, the cost of caring for the diabetic population has increased and is estimated at $245 billion per year [1]. Direct costs measure $176 billion with an estimated 43% making up hospital expenses [3]. The annual cost per capita to care for a diabetic patient is estimated to be $13,700 [3].
Impact of patient education on diabetes care
Studies have shown that educational interventions have a positive impact on diabetic patient outcomes [4]. These studies also found that educational interventions have positive effects in 50-80% of patient interactions [4]. Individual patient education results in better glucose control, which was accompanied by improved psychosocial and behavioural outcomes [5]. Empowerment, which is a patient approach that aims to increase a patient’s ability to think critically and make informed decisions, has shown positive outcomes related to weight, nutrition, and physical activity [6]. Setting behavioural goals on top of a structured didactic curriculum has been shown to be effective in supporting patient self-management [7].
Provider perceptions
One barrier to patient education and self-management lies in how providers perceive patients. Torres, Rozemberg, Amaral, and Bodstein [8] conducted a review of the perceptions, knowledge, and practices of primary care health providers who care for patients with type-2 diabetes. The review revealed shortfalls in provider preparation and knowledge of diabetes, including the diabetes educational delivery model. Additionally, providers felt that patients were unable to learn and understand the information that was presented to them [8]. This perception may affect how the provider delivers the educational content, as well as how the provider “buys in” to the importance of patient education to patient outcomes.
Community health workers
In the United States, community health workers’ role the healthcare system has been limited, primarily by lack of reimbursement through the fee-for-service model [9]. Across the U.S. there is little standardization in training, utilization, or compensation for community health workers [9]. There has been interest in the community health worker model across the globe, including making such workers integral, paid, full-time members of health systems [10]. The community health worker concept is replicable and scalable, having been shown effective across many areas of healthcare including chronic disease management [11]. The One Million Community Health Workers Campaign in Africa is training and deploying such workers in the local health systems. Programs in India use community health workers who are reimbursed through a fee-for-service structure where services such as immunization are performed [11]. Brazil uses community health workers in its family health programs [10].
Impact of community health workers on diabetes
Community health workers have focused on diabetes control in several areas of the U.S. One such program was the Mexican American Trial of Community Health Workers (MATCH), in which Rothschild et al. [12] studied 114 Mexican-Americans over a period of two years. One cohort was provided a bilingual newsletter on diabetes control and a second cohort received 36 home visits by a community health worker. The study found better-sustained glycemic control in the community health worker cohort [12].
Project Dulce was a culturally competent chronic disease management program in San Diego County, California, that focused on 153 high-risk diabetic patients using a nurse case manager who oversaw community health workers. The goal was to improve clinical outcomes, patient disease knowledge, and treatment satisfaction among diabetic patients. The study compared baseline and one-year levels of HbA1c, lipids, blood pressure, patient understanding of disease, and patient satisfaction. The focused intervention group showed significant improvements in all parameters [13,14].
A review of lay health advisors who worked on health promotion and disease prevention with a focus on Hispanic communities included 37 studies. Training for lay health advisors fell between six and 160 hours, and their role ranged from improving patient recruitment, acting as health advisors, materials distribution, and acting as community advocates. Of the 37 studies reviewed, 14 showed significant levels of effectiveness in management of diabetes [15].
EMS and community paramedicine
Many EMS patient interactions involve highly complex and acutely ill patients [16]. The current scope of practice for paramedics to provide treatments that are implemented via both on- and off-line medical direction from physicians after a assessment and impression that requires the paramedic to make complex decisions in often-stressful situations [16]. Paramedic education programs ensure competency in all skills and have oversight by state regulatory agencies [16].
Though new to the United States [17], community paramedicine is an organized system integrated into the local health system provided by EMS responders based on the local needs of the community. Emergency and primary-care physicians generally provide oversight of community paramedic programs. Community paramedic programs have recently received increased review and focus by government, professional organizations, and healthcare systems as the extensive healthcare reforms of the Accountable Care Act have made healthcare organizations look for innovative models of care delivery to address community needs and prevent unnecessary hospital readmissions [17].
Community paramedic programs use EMS providers in a different capacity from the current EMS system. Instead of rapidly responding, assessing, treating, and transporting patients, community paramedics are attempting to prevent unnecessary transportation, hospital admission, and transportation to alternate medical destinations [17]. The goal is to improve outcomes in vulnerable populations with associated cost and utilization reductions [17].
Currently there are three models for community paramedics. The first model has paramedics providing primary-care services under the direction of a physician in a patient’s home [17]. The paramedic acts within the scope of practice and has received specific training to provide such services. This model is not an on-going treatment method; rather, it is a discrete encounter during which the paramedic obtains a history and physical and communicates with other providers regarding the next steps. The second model is through a local health department that focuses on preventative services including immunizations and screenings at health fairs. The third model is the use of paramedics to assess, treat in the field, and then release or refer patients to other providers without transporting the patient to the emergency room [17]. There are many questions regarding the effectiveness of this method of care delivery, including oversight, reimbursement for services, and ensuring that patients have appropriate outcomes [17].
Around 2000, the Canadian province of Nova Scotia began a program that was the basis for the community paramedic movement. A single physician covered two islands in Nova Scotia, and when the physician’s retirement resulted in a massive gap in primary care [18], paramedics were hired to fill in. Approximately five years later, San Francisco, San Diego, and Washington D.C. began programs under which paramedics were sent into homeless populations with the goal of reduction of unnecessary EMS calls and emergency department visits. These programs have shown significant outcomes. For example, the program in San Francisco reduced emergency calls by 75% in 18 months within the targeted population. Cost savings for that program were estimated to be $12 million. However, as there was no reimbursement for these services, the program was ended by budget cuts in 2009 [18].
Another program in Fort Worth, Texas, through the provider MedStar, utilizes community paramedics to provide care in patients’ homes and through telephone calls. The target population is frequent users of EMS and emergency departments and patients that are at high risk for readmission to the hospital [19]. The community paramedics of Medstar are part of a mobile integrated healthcare practice. Community paramedics of Medstar follow the first community paramedic model through assessment, integration in health systems, and patient education until the patient can self-manage. This program has shown a significant improvement of utilization of the emergency department. Between July 2009 and November 2012, utilization of the emergency department decreased within the sample of 326 enrolees by 76.5% [19]. This has shown a cost savings of $26,818 per enrolled patient for EMS and emergency department utilization. Emergency department capacity has increased by more than 14,000 bed hours, and heart failure readmissions have decreased [19,20].
The concept of community paramedics is being explored and implemented internationally as well. Several programs in Australia have allowed paramedics to provide an alternative to transportation for emergency department evaluation [21]. These community paramedics patient encounters follow strict pre-defined criteria. Patient outcomes have been favorable in early analysis. Only 40% of patients treated by community paramedics were transported to the emergency department, compared with 74% of patients in traditional paramedic models. Of the patients released by the community paramedics, only 5% had an acute admittance to the emergency department within seven days of the community paramedic interaction [21].
Within the U.S., there has been significant movement and investment in community paramedic programs in Minnesota. The work on a community paramedic model began over 15 years ago when solutions to providing care to rural areas were being discussed [22]. This led to state pilot funding and development of a state training program. As the success of the pilot was realized, the program was expanded. In 2011 Minnesota became the first state through legislative efforts to establish reimbursement through state Medicaid for providers to be reimbursed for community paramedic visits [22].
Purpose
The data on the significance of diabetes on the population are clear from a clinical, population health, and financial perspective. Patient education programs and self-management programs have shown positive results in the management of diabetes through community health workers. Paramedics are integral members of the healthcare system. Changes to healthcare systems have provided opportunities for new and innovative health programs to address population health and health cost control. Community paramedic programs suggest that paramedics can successfully expand their roles beyond pre-hospital assessment, treatment, and rapid transportation. There may be continued opportunity for paramedics to expand their current scope of practice to specific population health management in vulnerable chronic-disease populations.
Our research highlighted the potential for paramedics to interact with the diabetic population in the United States with the goal of cost-effective care and improved clinical outcomes through patient education, with a focus on self-management and establish a baseline understanding of paramedics’ current knowledge of and attitude toward current chronic diabetes care.
Hypotheses
1.Paramedics can identify patients at high risk for diabetes, or diagnosed patients with self-management difficulties, and intervene with patient education and non-emergent interventions. Non-emergent interventions include patient screening, education and referral to additional health and social resources.
2.Positive paramedics attitude regarding the care of diabetes can make a paramedic delivered self-management program successful.
Methodology
Research design
The researchers performed a descriptive study to address the research questions. The proposed study design was a cross-sectional analysis, as it measured a single interaction between a researcher and participants using a survey. Data collection required a one-time administration of the survey, and there was minimal risk to participants, as participants’ risk was not greater than risks encountered ordinarily in daily life or psychological examinations or tests. The studied was reviewed by the A.T. Still University IRB and received exempt status.
Study participants
Participants recruited for the study were currently certified New York State Emergency Medical Technician-Paramedics. Participation was voluntary. Subjects were identified from public data accessible by the researchers. The participants were contacted via email and professional organizations. The data collection tool was accessible via a third-party online service. The collected data were entered into an Excel spreadsheet and analyzed using SPSS software.
Evaluation/measurement methods
The researcher used two tools to test the research questions. The first was the Diabetes Knowledge Test (DKT) by the Michigan Diabetes Research and Training Center [MDRTC] [23], used by permission. The DKT measures general knowledge of insulin-dependent and non-insulin dependent diabetes using 23 multiple-choice items. According to Fitzgerald et al. [24] the DKT showed reliability and validity in two different samples. Fitzgerald et al. [24] found that the coefficient was α ≥ 0.70. Collins, Mughal, Barnett, Fitzgerald and Lloyd [25] reached similar findings validating the DKT.
The Diabetes Attitude Scale [DAS-3], also by the MDRTC [23], and also used with permission, was the second instrument used. The goal of the DAS-3 is to provide a measure of attitudes related to diabetes. This scale can be used to measure attitudes across patients and healthcare providers. The DAS-3 is made up of 33 multiple-choice items broken into five sub-scales: the need for specialized training to provide diabetes care, the acuity of Type 2 diabetes, the importance of glucose control, the psychosocial effect, and the attitude toward self-care of diabetics. The subscales are each scored on a likert scale from one to five, with five being the high level of positive attitude. The subscales measure key components of patient care and behaviours that influence positive diabetic patient outcomes. Anderson, Fitzgerald, Funnel, and Gupen [26] found the DAS-3 to be valid and reliable and suitable for comparisons across cohorts of medical professionals. Internal consistency reliability by Cronbach's alpha coefficient was measured for each subscale with Need for special training to provide diabetes care: a=0.67, Seriousness of type 2 diabetes: a=0.80, Value of tight glucose control: a=0.72, Psychosocial impact of diabetes: a=0.65, and Attitude toward patient autonomy: a=0.76 [26].
Results
Sample characteristics
The data were analysed using IBM Statistics Package for Social Services (SPSS) Statistics version 22. Of 120 responses received, 47 were excluded as incomplete or because respondents failed to meet the inclusion criteria, leaving a sample size of 73. Results of skewness and Kurtosis testing found the data to be normal.
The majority of respondents’ length of time as a paramedic was between 10 and 20 years (38.4%, n=28). The remainder of respondents was evenly divided among 0-5 years, 5-10 years, and 20 years or longer (see Appendix A, Table 1). The largest two age groups of respondents were aged 30-39 years (n=23), and 40-49 years (n=22), with the remainder following a bell shaped curve for younger and older age groups (see Appendix A, Table 1). Highest level of education obtained of respondents varied from high school to graduate level, however, the majority were held either an associates (n=20) or bachelor’s degree (n=29) (see Appendix A and Table 1). Sex of respondents favoured male 75.3% (n=55) (see Appendix A and Table 1). The majority of respondents 68.5% (n=50) answered affirmatively the question “Do you have diabetes or have a close friend or relative with diabetes?” [Appendix A and Table 1].
| Variable | Segment | Frequency | Percentage |
|---|---|---|---|
| Time as a paramedic | <5 Years | 16/73 | 21.90 |
| 5-10 Years | 16/73 | 21.90 | |
| 10-20 Years | 28/73 | 38.40 | |
| >20 Years | 13/73 | 17.80 | |
| Age Range | 21 Years or Younger | 1/73 | 1.40 |
| 22-30 Years | 14/73 | 19.20 | |
| 30-39 Years | 23/73 | 31.50 | |
| 40-49 Years | 22/73 | 30.10 | |
| 50-59 Years | 12/73 | 16.40 | |
| 60 Years or Older | 1/73 | 1.40 | |
| Highest level of education obtained | Associate’s Degree | 20/73 | 27.40 |
| Bachelor’s Degree | 29/73 | 39.70 | |
| Graduate Degree | 8/73 | 11.00 | |
| High School / GED | 1/73 | 1.40 | |
| Some College | 15/73 | 20.50 | |
| Sex | Female | 18/73 | 24.70 |
| Male | 55/73 | 75.30 | |
| Do you have diabetes or have a close friend or relative with diabetes? | No | 23/73 | 31.50 |
| Yes | 50/73 | 68.50 |
Table 1: Properties of major study variables.
DKT analysis
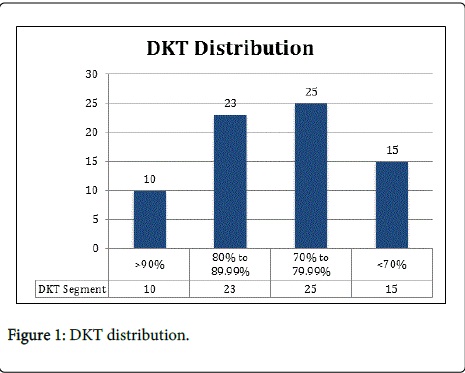
DKT scores were segmented by percentage correct into the following: greater than 90%, 80.00% and 89.99%, 70.00% and 79.99%, less than 70%. The respondents’ score on the DKT revealed 13.7% (n=10) scored greater than 90%, 31.5% (n=23) scored between 80.00% and 89.99%, 34.2% (n=25) scored between 70.00% and 79.99%, and 20.5% (n=15) scored less than 70% (see Appendix B and Figure 1). A one-way ANOVA was conducted at the p<.05 level to compare the effects of the variables on the DKT score. Length of time as a paramedic [F (3,69)=.933, p=.429], age [F (3,69)=1.375, p=.258], education level [F (3,69)=1.112, p=.350], sex [F (3,69)=.547, p=.652], or having a close friend or relative with diabetes [F (3,69)=.822, p=.486] did not have a significant effect on DKT segment [Appendix A and Table 2].
| Sum of Squares | df | Mean Square | F | Sig | ||
|---|---|---|---|---|---|---|
| I have been a paramedic for: | Between groups | 2.973 | 3 | 0.991 | 0.93 | 0.43 |
| Within groups | 73.246 | 69 | 1.062 | |||
| Total | 76.219 | 72 | ||||
| Which category below includes your age? | Between groups | 4.631 | 3 | 1.544 | 1.38 | 0.26 |
| Within groups | 77.452 | 69 | 1.122 | |||
| Total | 82.082 | 72 | ||||
| What is the highest level of education you have completed? | Between groups | 6.928 | 3 | 2.309 | 1.11 | 0.35 |
| Within groups | 143.29 | 69 | 2.077 | |||
| Total | 150.22 | 72 | ||||
| What is your sex? | Between groups | 0.315 | 3 | 0.105 | 0.55 | 0.65 |
| Within groups | 13.246 | 69 | 0.192 | |||
| Total | 13.562 | 72 | ||||
| Do you have diabetes or have a close friend or relative with diabetes? | Between groups | 0.544 | 3 | 0.181 | 0.82 | 0.49 |
| Within groups | 15.21 | 69 | 0.22 | |||
| Total | 15.753 | 72 |
Table 2: DKT Segment ANOVA Testing.
DAS-3 analysis
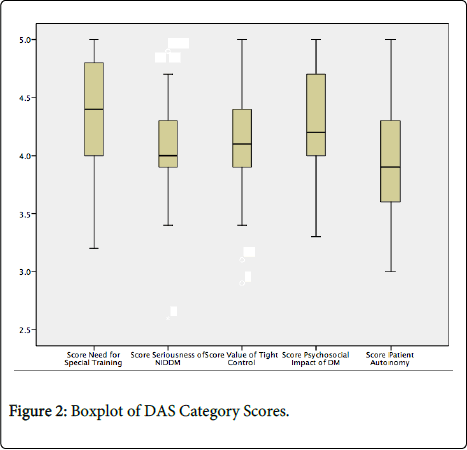
The respondents’ scores on all sections of the DAS-3 had a minimum of 3, maximum of 5, and a mode of 4. The need for specialized training had a mean of 4.39 and a median of 4.40, Seriousness of NIDDM had a mean of 4.07 and a median of 4.00, value of tight control had a mean of 4.12, and a median of 4.20, and finally the measure of patient autonomy had a mean of 3.94 and a median of 3.90 (see Appendix B and Figure 2).
A one-way ANOVA was conducted at the p<. 05 level to compare the effects of variables on the DAS-3 sections. Length of time as a paramedic, education level, sex, or having a close friend or relative with diabetes did not have a significant effect on DAS-3 Score for Special Training, Score for Seriousness of NIDDM, Score for Value of Tight Control, Score for Psychosocial Impact of DM, or Score for Patient Autonomy.
DKT score did not have a significant effect on DAS-3 Special Training [F (3, 69)=.172, p=.915], DAS-3 Score for Seriousness of NIDDM [F (3, 69)=.511, p=.676], DAS-3 score for Value of Tight Control [F (3, 69)=1.081, p=.363], DAS-3 score for Psychosocial Impact of DM [F (3, 69)=.338, p=.798], or DAS-3 score for Patient Autonomy [F (3, 69)=1.546, p=.210].
Discussion
The scores of the DKT reveal that 79.4% (n=58) of paramedics were able to answer 70% of the DKT questions correctly. Of the questions that paramedics answered incorrectly there were no discernable patterns. The majority of paramedics had an understanding of chronic diabetes, diabetes self-management, and interventions. Stronger scores on the DKT were not associated with length of time as a paramedic, age, education, sex, having a close friend or relative with diabetes, or any of the DAS-3 components. The findings demonstrate that paramedics have the potential to intervene with patient education in non-emergent chronic medical care.
The DAS-3 score revealed paramedics have a positive attitude about patients with diabetes and their ability to self-manage their disease. Higher scores on the DAS-3 were not associated with length of time as a paramedic, age, education level, sex, having a close friend or relative with diabetes, or DKT score. This finding suggested that paramedics believe that self-management of chronic diabetic patients is important and possible. There were no identified drivers for this belief with the exception of being a paramedic.
Paramedics had mean scores that were consistent or better than other healthcare providers. Clark and Hampson [27] studied attitudes of patients, physicians, nurses, and dieticians toward diabetes using the DAS-3. Compared to the Clark and Hampson’s [27] findings, paramedics scored higher than patients in all subscales of the DAS and higher than physicians in all areas with the exception of seriousness of diabetes. Compared to nurses and dieticians, paramedics scored lower on DAS-3 subsections for special training, seriousness of Type-2 diabetes, and patient autonomy, and scored higher on value of tight control and psychosocial impact of diabetes. These findings show that paramedics’ attitude is positive regarding the care of diabetes; therefore, the potential of a successful paramedic-delivered diabetic self-management program exists.
However, further integration of paramedics in the current healthcare system poses additional questions. The first is the form these potential expanded-scope paramedic programs might take. Community health worker models have been associated with positive outcomes [9] and provide a framework for care delivery that could be transferrable to the extended scope of paramedic practice. If a community health worker model is chosen, a gap analysis would be needed to identify the differences in practice and education between paramedic and community health worker programs. The structure of the program would then drive the appropriate education, i.e., whether it should be integrated into the base paramedic national training standards or an additional program after initial training. Changes may be necessary to current laws regarding paramedic scope of practice on a state level to implement any new programs. The final two areas that need to be addressed are actual outcomes associated with such programs and the reimbursement model needed to sustain such programs.
Conclusion
The research confirmed both hypotheses: 1) that paramedics can identify patients at high risk for diabetes, or diagnosed patients with self-management difficulties, and intervene with patient education and non-emergent interventions and 2) that a positive attitude regarding the care of diabetes can make a paramedic-delivered self-management program successful. The findings of the research demonstrate that paramedics have a knowledge base and appropriate attitude to provide diabetes self-management programs as part of an expanded scope of paramedic practice. There are additional areas that current paramedic training standard does not cover.
A future diabetes management program using paramedics as a delivery model is a possibility. Utilizing existing educational delivery models, primarily the community health worker model, to train paramedics is a low cost alternative to current community paramedic training models or utilization of higher costs nursing or allied health resources. Patient education and communication is currently not included in paramedic training standards, but would be necessary for a patient education or self -management program to be successful. These paramedics could be contracted though health delivery, managed care, or accountable-care organizations to provide home delivered diabetes management programs from a population health perspective. Currently most diabetes self-management programs are delivered in a setting outside of a patient’s home. If a delivery program were delivered inside of a patient’s home, where the patient eats, exercises, and interacts with family the self-management program could be tailored directly for that individual patient. From an operational perspective there is a existing operational structure, personnel, vehicles, and health organization relationships.
The use of paramedics would enable the healthcare system to use an existing resource, which if implemented correctly, could provide additional services to improve overall patient care, health outcomes, and costs. Paramedics hold great potential as a resource to reach vulnerable chronic disease populations to whom the current healthcare system has limited access.
References
- Centers for Disease Control and Prevention (2011) National diabetes fact sheet: national estimates and general information on diabetes and pre-diabetes in the United States.
- Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF (2010) Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr, 8:29.
- American Diabetes Association (2013). Economic costs of diabetes in the US in 2012. Diabetes Care, 36:1033-1046.
- Lagger G, Pataky Z, Golay A (2010) Efficacy of therapeutic patient education in chronic diseases and obesity. Patient education and counseling, 79,283-286.
- Sperl-Hillen J, Beaton S, FernandesO, Von WA, Vazquez-B G, et al. (2011) Comparative effectiveness of patient education methods for type 2 diabetes: a randomized controlled trial. Archives of internal medicine 171:2001-2010.
- Anderson RM,Funnell MM (2010) Patient empowerment: myths and misconceptions. Patient education and counseling 79:277-282.
- Haas L, Maryniuk M, Beck J, Cox CE, Duker P, et al. (2013) National standards for diabetes self-management education and support. Diabetes Care 36(Supplement 1): S100-S108.
- Torres HC Rozemberg B, Amaral MA, Bodstein RC (2010) Perceptions of primary healthcare professionals towards their role in type 2 diabetes mellitus patient education in Brazil. BMC public health 10:583.
- Singh P, Chokshi DA (2013) Community health workers: an opportunity for reverse innovation–Authors' reply. The Lancet 382:1327.
- Singh P, Sachs JD (2013) 1 million community health workers in sub-Saharan Africa by 2015. The Lancet 382:63-365.
- Bhutta ZA, Lassi ZS, Pariyo G, Huicho L (2010) Global experience of community health workers for delivery of health related millennium development goals: a systematic review, country case studies, and recommendations for integration into national health systems. Global Health Workforce Alliance.
- Rothschild SK, Martin MA, Swider SM, Lynas CT, Avery EF, et al. (2012) The Mexican-American Trial of Community Health workers (MATCH): Design and baseline characteristics of a randomized controlled trial testing a culturally tailored community diabetes self-management intervention. Contemporary clinical trials 33:369-377.
- Gilmer TP, PhilisTA, Walker C (2005) Outcomes of Project Dulce: a culturally specific diabetes management program. Annals of Pharmacotherapy 39:817-822.
- PhilisTA, Walker C (2001) Improved care for diabetes in underserved populations. The Journal of ambulatory care management 24(1): 39-43.
- Rhodes SD, Foley KL, Zometa CS, Bloom FR (2007) Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. American journal of preventive medicine 33:418-427.
- National Highway Traffic Safety Administration (2007). National EMS scope of practice model. DOT HS 810: 657.
- Goodwin J (2012) The Power of Community. Three new community paramedicine programs are poised to take off with federal innovation grants. Best Practice in Emergency Services 15:1-8.
- Johnson K (2011) Responding before a call is needed. New York Times, A12.
- MedStar (2012)MedStar launches new 9-1-1 nurse triage program. EMS World.
- Mitchell M (2011) In Fort Worth, MedStar's community health program cutting costs, improving patients' well-being. Fort Worth Star-Telegram.
- Hoyle S, Swain AH, Fake P, Larsen PD (2012) Introduction of an extended care paramedic model in New Zealand. Emergency Medicine Australasia 24:652-656.
- Michigan Diabetes Research and Training Center (2013). Survey instruments.
- Erich J (2013) How Minnesota got its community medics paid. 2013.
- Fitzgerald JT, Funnell MM, Hess GE, Barr PA, Anderson RM, et al. (1998) The reliability and validity of a brief diabetes knowledge test. Diabetes care 21:706-710.
- Collins GS, Mughal S, Barnett AH, Fitzgerald J, Lloyd CE (2011) Modification and validation of the Revised Diabetes Knowledge Scale. Diabetic Medicine 28:306-310.
- Anderson R, Fitzgerald JT, Funnell MM, Gruppen LD (1998) The third version of the Diabetes Attitude Scale. Diabetes care 21:1403-1407.
- Clark M, Hampson SE (2003) Comparison of patients’ and healthcare professionals’ beliefs about and attitudes towards Type 2 diabetes. Diabetic medicine 20:152-154
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 14914
- [From(publication date):
February-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10324
- PDF downloads : 4590