Research Article Open Access
MDR1 C3435T Polymorphism is a Susceptible Marker for the Late Onset Japanese UC
Sawasaki T, Nanjo S and Sugiyama T*Department of Gastroenterology, Graduate School of Medicine and Pharmaceutical Science, Sugitani 2630, Toyama City, Toyama 930-0194, Japan
- *Corresponding Author:
- Toshiro Sugiyama
MD, Ph.D., Department of Gastroenterology
Graduate School of Medicine and PharmaceuticalScience
Sugitani 2630, Toyama City, Toyama 930-0194, Japan
Tel: 81-76-434-7300
E-mail: tsugi@med.u-toyama.ac.jp
Received date: August 11, 2015 Accepted date: August 21, 2015 Published date: August 28, 2015
Citation: Sawasaki T, Nanjo S, Sugiyama T (2015) MDDR1 C3435T Polymorphism is a Susceptible Marker for the Late Onset Japanese UC. J Gastrointest Dig Syst 5:326. doi:10.4172/2161-069X.1000326
Copyright: © 2015 Sawasaki T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: The multi-drug resistance 1 (MDR1) gene is reported to correlate with the function and the expression of P-glycoprotein (P-gp), and the carriers of MDR1 C3435T polymorphism are speculated to have an increased susceptibility to ulcerative colitis (UC) in western countries. The aim of this study is to investigate whether MDR1 C3435T polymorphism is a susceptible marker for the onset of UC in Japanese patients. Patients and Methods:We obtained blood samples from 38 patients with UC and that from 76 healthy controls, and genomic DNA from leucocytes was extracted. MDR1 C3435T polymorphism was determined by polymerase chain reaction-restriction fragment length polymorphism methods. The expression of P-gp was examined by immunohistochemistry in colonic tissues with UC. Results: Both the frequencies of TT genotype (p=0.023) and T allele (p=0.011) were significantly higher in the late onset UC groups than in the control group in Japanese UC patients. The protein of P-gp in colonic tissues showed lower expression in UC patients with TT genotype by immunohistological analysis. Conclusion: MDR1 C3435T polymorphisms are linked to the susceptibility of the late onset Japanese UC patients, probably via the lower exported activity of the related pathogenic environmental factors in colon.
Abstract
Background: The multi-drug resistance 1 (MDR1) gene is reported to correlate with the function and the expression of P-glycoprotein (P-gp), and the carriers of MDR1 C3435T polymorphism are speculated to have an increased susceptibility to ulcerative colitis (UC) in western countries. The aim of this study is to investigate whether MDR1 C3435T polymorphism is a susceptible marker for the late onset of UC in Japanese patients.
Patients and Methods:We obtained blood samples from 38 patients with UC and that from 76 healthy controls, and genomic DNA from leucocytes was extracted. MDR1 C3435T polymorphism was determined by polymerase chain reaction-restriction fragment length polymorphism methods. The expression of P-gp was examined by immunohistochemistry in colonic tissues with UC.
Results: Both the frequencies of TT genotype (p=0.023) and T allele (p=0.011) were significantly higher in the late onset UC groups than in the control group in Japanese UC patients. The protein of P-gp in colonic tissues showed lower expression in UC patients with TT genotype by immunohistological analysis.
Conclusion: MDR1 C3435T polymorphisms are linked to the susceptibility of the late onset Japanese UC patients, probably via the lower exported activity of the related pathogenic environmental factors in colon.
Keywords:
Ulcerative colitis; MDR1 Gene; Polymorphism; Late-Onset; Ethnic difference
Abbreviations:
UC: Ulcerative colitis, MDR-1: Multi-drug resistance 1; SNPs: Single nucleotide polymorphisms
Introduction
Inflammatory bowel diseases are chronic inflammatory disorders of the gastrointestinal tracts due to an undefined etiology. Ulcerative colitis (UC) has developed in younger generation as well as older generations around 60 years old, with two peaks of the frequency in Japan. On the other hands, Crohn's disease (CD) has restrictedly developed in younger generation. The developments of UC or CD are closely associated with genetic abnormality, other genetic factors, intestinal flora, environmental factors including foods, and those interactions. Recently, genome-wide association studies regarding the disease susceptibility were conducted and identified in CD or UC [1,2]. Genetic factors have a more dominant role in the pathogenesis of CD. For example, the CARD15/NOD2 gene, which is located on chromosome 16, was shown to be strongly associated with the susceptibility to CD, but not to UC in western countries [3-7]. However, large scaled Japanese study regarding CD was unable to confirm this association, which suggested that the ethnic differences regarding genetic factors including single nucleotide polymorphisms (SNPs) were critical in the susceptibility of CD or UC.
The multi-drug resistance 1 (MDR1) gene is one candidate for disease susceptibility in UC in western countries. The MDR1 gene is located at the susceptibility locus for IBD identified using genome wide scanning in UK cohort study [8]. MDR1 gene is encoding P-glycoprotein (P-gp), which is localized at the apical membrane of intestinal epithelial cells. P-gp is an adenosine triphosphate-binding cassette transporter that exports some substances outside from cells with energy-dependent manner [9-12]. P-gp has also functions as an important barrier, protecting organs against foreign chemicals and bacteria and their toxins, and may also play a role in steroid metabolism. In addition, the expression and function of MDR1 gene products can directly affect the effectiveness of therapeutic drugs [13]. Mdrla-/- mice have developed UC-like colitis under specific pathogen free condition and the colitis can be resolved with antibiotic treatment [14]. Therefore, MDR1 might associate to develop UC-like colitis due to having some effects on the interaction between host response and environmental factors including intestinal flora.
The MDR1 gene is highly polymorphic. Two SNPs, variants C3435T and G2677T/A, were correlated with the activity and the expression of P-gp14. In 2003, Schwab et al. reported that both the T allele and TT genotype of the MDR1 C3435T polymorphism were associated with an increased susceptibility to UC patients in Germany [15]. Since then, the search for the MDR1 C3435T polymorphism has advanced in various countries. However, the linkage to MDR1 C3435T polymorphism with the onset of UC were controversial among the ethnic [16-18]. Only one study in Japanese patients [19] reported that MDR1 C3435T was a predictive factor for in the susceptibility of UC patients. However, it remains unclear how the MDR1 C3435T polymorphism was related to US and how the polymorphism was related to the function in Japanese study. Therefore, we investigated that the linkage to MDR1 C3435T polymorphism with the onset of UC, the functional linkage and other clinical phenotypes, including the extent of disease, the effect of steroid therapy, and disease severity in Japanese UC patients.
Materials and Methods
Study subjects
A total of 38 Japanese UC patients (19 men, 19 women; mean age: 39.3 ± 12.8 years) and 76 healthy control subjects (38 men, 38 women; mean age: 32.4 ± 5.8 years) were included in the study. The subject number of healthy control group was twice to UC patients group and with gender matching. Diagnosis of UC was assessed according to the clinical guidelines in Japan and criteria based on clinical, endoscopic, radiological, and histopathological examination. Clinical data including the extent of disease, use of steroid, and disease severity, were recorded. All data were collected while the investigator was blinded on the MDR1 genotype and allele. The patients were divided into 2 groups based on age of onset of UC: the early onset group (onset before 30 years of age) and the late onset group (onset at 30 years of age or older).
Blood samples were obtained from UC patients recruited from Toyama University Hospital and Takaoka City Hospital.
Genotyping
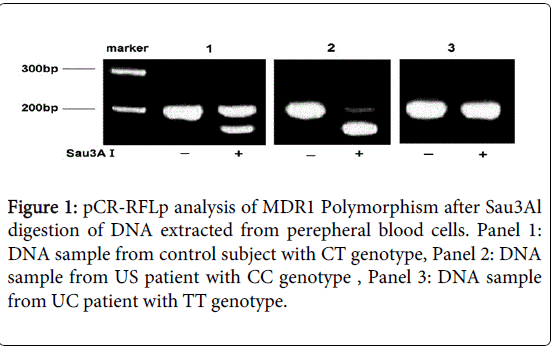
Genomic DNA samples were isolated from whole blood using the QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany), and were analyzed using polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) methods. The PCR primer pairs and restriction enzyme described by Cascorbi et al. [20] were used for PCR amplification and restriction enzyme digestion of the MDR1 gene. The PCR conditions were the following: initial denaturation at 94°C for 2 min, followed by 35 cycles of denaturation at 94°C for 30 s, annealing at 60°C for 30 s, extension at 72°C for 30 s, and finally, terminal elongation at 72°C for 7 min. The PCR reactions were carried out in a Gene Amp® PCR System 9700 thermal cycler (Applied Biosystems Japan, Tokyo, Japan). After amplification, Sau3A I (New England BioLabs, Inc., Acton, Massachusetts , USA) was added to the basal buffer and incubated at 37°C for 2 h to digest the 197-bp DNA product into 158-bp and 39-bp fragments. DNA fragments generated after restriction enzyme digestion were separated on a 3.5% agarose gel. Restriction fragments were visualized with ethidium bromide staining of the agarose gel using an ultraviolet transilluminator. Written informed consents were taken from all patients and control subjects before starting the study.
Immunohistochemistry
Immunohistochemical analysis was conducted in 38 patients who had undergone colonoscopy and colon biopsies. The formaldehyde-fixed, paraffin-embedded tissue sections were deparaffinized in xylene and rehydrated. A 0.05% citraconic anhydride solution (ImmunoSaver; Nissin EM Co., Ltd., Tokyo, Japan) was used for antigen retrieval. Endogenous peroxidase activity was quenched with a 3% H2O2 solution for 5 min. Slides were dipped in 5% bovine serum albumin for 5 min. We used the MDR1 monoclonal antibody JSB-1 as the primary antibody (Millipore Corp., Billerica, MA, USA). JSB-1 antibody was diluted by phosphate-buffered saline at a dilution of 1:100 for immune-histochemistry. The anti-mouse IgG antibody conjugated with HRP from the EnVision+ System/HRP Mouse kit (Dako, Carpenteria, CA, USA) was used. Slides were then treated with 3,3-diaminobenzidine tetrahydrochloride (DAB; Sigma, St. Louis, MO, USA) for visualization. All slides were counterstained with hematoxylin and mounted. As a negative control, primary antibody was omitted and phosphate-buffered saline was used instead.
Statistical Analysis
Values are expressed as the means ± S.D. Fisher's exact test was used to examine the differences in genotype and allele frequencies between groups and in immunohistological study of colon tissues and p values less than 0.05 were considered as a statistical significance.
Ethical Considerations
All of this study was approved by the ethics committee of the Medical Faculty of Toyama University, and the informed consent was obtained from all participants prior to the study .
Results
The clinical characteristics of the patients are summarized in Table 1. In UC patients, there was no gender difference and the mean age was 39.3 years and the mean onset age was 30.3 years. An example of the electrophoresis to determine the MDR1 C3435T polymorphism was shown in Figure 1, in which the PCR product of C allele was digested by Sau3A1 and the small digested bands were observed, and PCR product of T allele was not digested by Sau3AI. In CC genotype (Figure 1, lane 2), two C alleles were digested and small broad digested band was observed. In TT genotype, PCR products were not digested and the size of PCR products was not changed (Figure 1, lane 3). The genotype and allele frequencies of the MDR1 C3435T polymorphism in the 38 UC patients and 76 age and gender matched healthy control subjects are shown in Table 2. Although the genotype TT and allele T tended to be higher frequencies in UC patients, the difference was not statistically significant (p=0.121 for genotype and p=0.069 for allele). Additionally, there was no gender differences in patient group and in UC group.
| Male | 19 |
| Female | 19 |
| Age (ys) | |
| Mean ± SD | 39.3 ± 12.8 |
| Range | 18-73 |
| Onset Age (ys) | |
| Mean ± SD | 30.3 ± 11.9 |
| Range | 15-60 |
| Disease Location | |
| Pan-colitis | 26 |
| Left-side colitis | 10 |
| Proctitis | 2 |
Table 1: Clinical characteristics of Japanese patients with UC.
| Patients/ Controls | Genotype(%) | Allele(%) | CC vs. TT | C vs. T | |||
| CC | CT | TT | C | T | p-value | ||
| UC | 3 | 19 | 16 | 25 | 51 | ||
| (n=38) | (7.9) | (50) | (42.1) | (32.9) | (67.1) | 0.121 | 0.069 |
| Control | 16 | 42 | 18 | 74 | 78 | ||
| (n=76) | (21.1) | (55.3) | (23.6) | (48.7) | (51.3) | ||
Table 2: Frequency of MDR1 C3435T allele and genotype of the patients with UC and controls.
However, the TT genotypes and T alleles were significantly more frequent in the late onset UC group (the onset after 30 years old) than in the control group (Table 3, p=0.023 for genotype and 0.011 for allele).
| Patients/ Controls |
Genotype(%) | Allele(%) | CC vs. TT | C vs. T | ||||
| CC | CT | TT | C | T | p-value | |||
| Early onset | 3 | 12 | 7 | 18 | 26 | |||
| (n=22) | (13.6) | (54.5) | (31.9) | (40.9) | (59.1) | 0.448 | 0.451 | |
| Late onset | 0 | 7 | 9 | 7 | 25 | |||
| (n=16) | (0) | (43.8) | (56.2) | 21.9 | 78.1 | 0.023 | 0.011a | |
| Control | 16 | 42 | 18 | 74 | 78 | |||
| (n=76) | (21.1) | (55.3) | (23.6) | (48.7) | (51.3) | |||
Table 3: Frequency of MDR1 C3435T allele and genotype of the patients with early onset and late onset UC.
Genotype and allele frequencies were not significantly different between the early onset UC group and the control group (Table 3, p=0.448 for genotype and p =0.451 for allele).
There was a significant difference in TT genotype allele frequencies between the late onset UC group and the control group.
Even if the range of the cut-off age was changed from 30 to 35 year.
The association between the phenotype of disease extent and the MDR1 C3435T polymorphism was also investigated.
Disease extent were categorized as two phenotypes, proctitis type and extended colitis type (pan-colitis and left-side colitis).
The T allele was significantly more frequent in UC patients with extended colitis (p=0.045).
In the late onset UC group, the TT genotype and T allele were significantly more frequent in patients with extended colitis (Table 4, p=0.023 for genotype and 0.008 for allele).
| Patients/ Controls |
Genotype(%) | Allele(%) | CC vs. TT | C vs. T | ||||
| CC | CT | TT | C | T | p-value | |||
| Early onset with UC with extend colitis | 3 11 7 | 17 | 25 | |||||
| (n=21) | (14.3) | (52.4) | (33.3) | (40.5) | (59.5) | 0.448 | 0.443 | |
| Late onset with UC with extend colitis | 0 | 6 | 9 | 6 | 24 | |||
| (n=15) | (0) | (40.0) | (60.0) | 20 | 80 | 0.023a | 0.018a | |
| Control | 16 | 42 | 18 | 74 | 78 | |||
| (n=76) | (21.1) | (55.3) | (23.6) | (48.7) | (51.3) | |||
Table 4: Frequency of MDR1 C3435T allele and genotype of the patients with extended colitis. (a : Fisher's exact test ).
The disease severity in UC was not significantly associated with a particular allele or genotype.
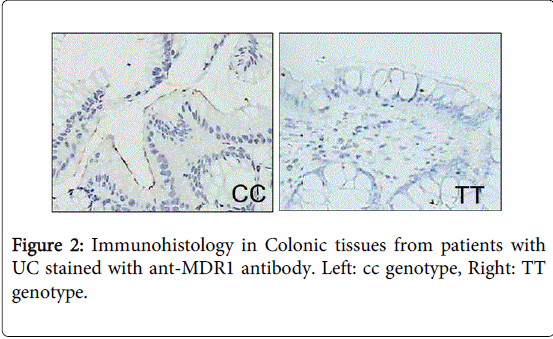
Immunostaining was conducted in colonic tissue samples from 38 UC patients (3 patients with the CC genotype, 19 patients with the CT genotype, and 16 patients with the TT genotype). The apical membrane of the colonic epithelial cells were stained in 15 patients with either the CC or CT genotype (15/22:68.2%), but only in 3 patients with the TT genotype (3/16:18.8%) (Table 5 and Figure 2).
| CC/ CTgenotype(%) | TTgenotype(%) | p-value | |
| MDR1 protein | 15/22(68.2%) | 3/16(18.8%) | 0.010a |
Table 5: Frequency of MDR1 C3435T allele and genotype of the patients with extended colitis.
MDR1 protein expression in colon tissue from the patients with TT genotype was significantly lower than that from the patients with CC/CT genotype (p=0.010).
Discussion
In this study, we have examined the relationship between the onset, the clinical phenotype of UC and MDR1 C3435T polymorphism in Japanese UC patients. Additionally, clinical subgroup by phenotype (the extent of disease, the effect of steroid therapy, and the disease severity) were investigated in our study, because the previous results were controversial among studies and conclusive evidences were not obtained [15-19]. Two peaks in the onset of UC have been observed in previous studies [21-25] and the major etiology associated to the early or late onset UC might be different between each groups. In our study, the genotype and allele frequencies of the MDR1 C3435T gene were more frequently found in the late onset group than in the control group. A significant difference on the MDR1 C3435T polymorphism between the two groups was confirmed even if the cut-off age was changed from 30 to 35 year old.
MDR1 gene is encoding P-gp, which is located at the apical membrane of epithelial cells in the intestine and the colon. P-gp has an important barrier function to foreign substances by exporting mechanisms from the gastrointestinal epithelial cells into the lumen, additionally might be regulating the absorption or export of the drugs [13]. Therefore, the activity of P-gp may have an influence on the effectiveness of some drugs, which are used to treat UC. We have investigated the relationship between the efficacy of glucocorticoid therapy against UC and this polymorphism in our present study, however no clear conclusion was obtained.
Only one paper on Japanese was published by Nakamura et al. They have investigated that the association between the polymorphism (C3435T) in exon 26 of the MDR1 gene and the expression level of MDR1 mRNA in duodenal enterocytes from healthy Japanese subjects [21]. They have showed that the T allele was associated with an elevated expression of MDR1 mRNA of the subjects. This result is in contrast to the results in Caucasian studies, in which the T allele was associated with a low expression of P-gp. These controversial observations may be suggesting that the linkage between MDR1 polymorphism and the protein expression may be different among ethnics. However, our results on the expression of MDR1 protein in colonic tissues from the Japanese UC patients were consist with many Caucasian studies, showing low expression of P-gp with TT genotype. On the other hands, the result of only one previous study [19] on Japanese UC patients was also similar to the previous study, however it is also controversial on the expression of P-gp with TT genotype from our study. In our study, MDR1 protein was expressed and located at the apical membrane of epithelial cells in the colon. In terms of the path-physiological association with the onset of UC, the lower expression of MDR1 protein in the colon may be linked to the lower exported activity of UC-associated exogenous factors, including environmental factors, antigens, diet and bacterial components. Long-term exposures to these factors in colonic epithelial cells, or low exported activity of these factors by no expression of MDR1 at the apical membrane, may trigger the aberrant immune response against them and may have a functional association to the late onset of UC after the accumulations of these UC-associated exogenous factors for long period. To confirm the precise attributable risk of MDR1 polymorphism regarding the late onset of UC in Japanese patients, a larger-scaled population study might be required.
In conclusion, we investigated the relationship between the MDR1 C3435T polymorphism and the expression of P-gp in 38 Japanese UC patients. The MDR1 gene C3435T polymorphism, TT genotype, and T allele are associated to the late onset UC and the low expression of P-gp were found in the colonic tissues, probably resulted in the aberrant immune responses via the accumulation of exogenous factors including environmental factors, antigens, diet and bacterial components in late onset UC.
References
- Taylor KD, Yang H, Rotter JI (2001) Inflammatory bowel disease. II. Gene mapping. See comment in PubMed Commons below Mol Genet Metab 74: 22-44.
- Watts DA, Satsangi J (2002) The genetic jigsaw of inflammatory bowel disease. See comment in PubMed Commons below Gut 50 Suppl 3: III31-36.
- Hugot J, Chamaillard M, Zouali H, Lesage S, Cézard JP, et al. (2001) Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn's disease. See comment in PubMed Commons below Nature 411: 599-603.
- Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, et al. (2001) A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. See comment in PubMed Commons below Nature 411: 603-606.
- Hampe J, Grebe J, Nikolaus S, Solberg C, Croucher PJ, et al. (2002) Association of NOD2 (CARD 15) genotype with clinical course of Crohn's disease: a cohort study. See comment in PubMed Commons below Lancet 359: 1661-1665.
- Cuthbert AP, Fisher SA, Mirza MM, King K, Hampe J, et al. (2002) The contribution of NOD2 gene mutations to the risk and site of disease in inflammatory bowel disease. See comment in PubMed Commons below Gastroenterology 122: 867-874.
- Lesage S, Zouali H, Cézard JP, Colombel JF, Belaiche J, et al. (2002) CARD15/NOD2 mutational analysis and genotype-phenotype correlation in 612 patients with inflammatory bowel disease. See comment in PubMed Commons below Am J Hum Genet 70: 845-857.
- Satsangi J, Parkes M, Louis E, Hashimoto L, Kato N, et al. (1996) Two stage genome-wide search in inflammatory bowel disease provides evidence for susceptibility loci on chromosomes 3, 7 and 12. See comment in PubMed Commons below Nat Genet 14: 199-202.
- Gottesman MM, Pastan I, Ambudkar SV (1996) P-glycoprotein and multidrug resistance. See comment in PubMed Commons below Curr Opin Genet Dev 6: 610-617.
- Ambudkar SV, Dey S, Hrycyna CA, Ramachandra M, Pastan I, et al. (1999) Biochemical, cellular, and pharmacological aspects of the multidrug transporter. See comment in PubMed Commons below Annu Rev Pharmacol Toxicol 39: 361-398.
- Ueda K, Clark DP, Chen CJ, Roninson IB, Gottesman MM, et al. (1987) The human multidrug resistance (mdr1) gene. cDNA cloning and transcription initiation. See comment in PubMed Commons below J Biol Chem 262: 505-508.
- Chen CJ, Clark D, Ueda K, Pastan I, Gottesman MM, et al. (1990) Genomic organization of the human multidrug resistance (MDR1) gene and origin of P-glycoproteins. See comment in PubMed Commons below J Biol Chem 265: 506-514.
- Hoffmeyer S, Burk O, von Richter O, Arnold HP, Brockmöller J, et al. (2000) Functional polymorphisms of the human multidrug-resistance gene: multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo. See comment in PubMed Commons below Proc Natl Acad Sci U S A 97: 3473-3478.
- Panwala CM, Jones JC, Viney JL (1998) A novel model of inflammatory bowel disease: mice deficient for the multiple drug resistance gene, mdr1a, spontaneously develop colitis. See comment in PubMed Commons below J Immunol 161: 5733-5744.
- Schwab M, Schaeffeler E, Marx C, Fromm MF, Kaskas B, et al. (2003) Association between the C3435T MDR1 gene polymorphism and susceptibility for ulcerative colitis. See comment in PubMed Commons below Gastroenterology 124: 26-33.
- Croucher PJ, Mascheretti S, Foelsch UR, Hampe J, Schreiber S (2003) Lack of association between the C3435T MDR1 gene polymorphism and inflammatory bowel disease in two independent Northern European populations. See comment in PubMed Commons below Gastroenterology 125: 1919-1920.
- Glas J, Török HP, Schiemann U, Folwaczny C (2004) MDR1 gene polymorphism in ulcerative colitis. See comment in PubMed Commons below Gastroenterology 126: 367.
- Ho GT, Nimmo ER, Tenesa A, Fennell J, Drummond H, et al. (2005) Allelic variations of the multidrug resistance gene determine susceptibility and disease behavior in ulcerative colitis. See comment in PubMed Commons below Gastroenterology 128: 288-296.
- Osuga T, Sakaeda T, Nakamura T, Yamada T, Koyama T, et al. (2006) MDR1 C3435T polymorphism is predictive of later onset of ulcerative colitis in Japanese. See comment in PubMed Commons below Biol Pharm Bull 29: 324-329.
- Cascorbi I, Gerloff T, Johne A, Meisel C, Hoffmeyer S, et al. (2001) Frequency of single nucleotide polymorphisms in the P-glycoprotein drug transporter MDR1 gene in white subjects. See comment in PubMed Commons below Clin Pharmacol Ther 69: 169-174.
- Nakamura T, Sakaeda T, Horinouchi M (2002) Effect of the mutation (C3435T) at exon 26 of the MDRl gene on expression level of MDRl messenger ribonucleic acid in duodenal enterocytes of healthy Japanese subjects. Clinical Pharmacology & Therapeutics 71:297-303.
- Ekbom A (2004) The epidemiology of IBD: a lot of data but little knowledge. How shall we proceed? See comment in PubMed Commons below Inflamm Bowel Dis 10 Suppl 1: S32-34.
- Björnsson S, Johannsson JH, Oddsson E (1998) Inflammatory bowel disease in Iceland, 1980-89. A retrospective nationwide epidemiologic study. See comment in PubMed Commons below Scand J Gastroenterol 33: 71-77.
- Björnsson S, Jóhannsson JH (2000) Inflammatory bowel disease in Iceland, 1990-1994: a prospective, nationwide, epidemiological study. See comment in PubMed Commons below Eur J Gastroenterol Hepatol 12: 31-38.
- Bernstein CN, Blanchard JF, Rawsthorne P, Wajda A (1999) Epidemiology of Crohn's disease and ulcerative colitis in a central Canadian province: a population-based study. See comment in PubMed Commons below Am J Epidemiol 149: 916-924.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13928
- [From(publication date):
August-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9409
- PDF downloads : 4519