Research Article Open Access
May-Thurner Syndrome, the Role of Endovascular Intervention with Review of Published Treatment and Follow up Strategies
Aws Alfahad1*, Raghuram Lakshminarayan2 and Mohammed Ahmed2
1Interventional radiology fellow at Hull royal infirmary, UK
2Consultant radiologist at Hull royal infirmary, UK
- *Corresponding Author:
- Alfahad A
Hull and East Yorkshire Hospitals NHS Trust Hull
Yorkshire UK
Tel: 00441482875875
E-mail: aws.alfahad@nhs.net
Received Date: July 08, 2015; Accepted Date: August 11, 2015; Published Date: August 13, 2015
Citation: Alfahad A, Lakshminarayan R, Ahmed M (2015) May-Thurner Syndrome, the Role of Endovascular Intervention with Review of Published Treatment and Follow up Strategies. J Clin Diagn Res 3:118. doi:10.4172/2376-0311.1000118
Copyright: © 2015 Alfahad A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Clinical Diagnosis and Research
Abstract
May-Thurner syndrome is a unique condition that strikes mainly young people. Its prevalence is likely underestimated and perhaps ranges from 22 to 32%. May-Thurner is under reported and often miss-diagnosed in accident and emergency, which can result in long term complication (post thrombotic syndrome) with its detrimental effect in this young age group. We describe a case of May-Thurner syndrome, a near miss, with review of published treatment and follow up strategies. This includes direct catheter thrombolysis, angioplasty, stenting, and IVC filter placement. Our patient has made a good recovery on follow up.
Introduction
May-Thurner syndrome (MTS), also called iliocaval compression syndrome, Cockett’s syndrome, or non-occlusive iliac vein lesion, occurs secondary to compression of the left iliac vein by the overriding right iliac artery [1]. From autopsy studies, MTS accounts for 2-3% of lower limb deep vein thrombosis [2]. However; it is often underreported and miss-diagnosed in accident and emergency, resulting in long-term complication (post thrombotic syndrome) with its detrimental effect [3]. Possible mechanisms include vascular trauma to the vein from repetitive compression from the overlying pulsating artery, causing elastin and collagen deposition in the iliac vein, which eventually leads to spur formation [4].
Usually doppler ultrasound will detect if a deep vein thrombosis is present in the iliac vessels, but is unable to visualize iliac vein compression and spurs. Diagnostic modalities include helical abdominal computed tomography (CT), magnetic resonance venography (MRV), intravenous ultrasound (IVUS) and conventional venography would allow accurate diagnosis and facilitate in management planning [5].
Clinical Presentation
A 33-year-old woman presented with acute onset pain and swelling of left leg following two intense running episodes for charity. Apart from taking regular oral contraceptive pills (OCP), she had no previous history of trauma, surgery or deep vein thrombosis. On her first presentation to the accident and emergency department, she was reassured. Few days later, she represented when her left leg duplex ultrasonography didn’t identify any clots in the left leg.
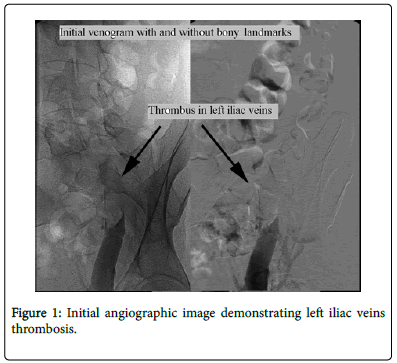
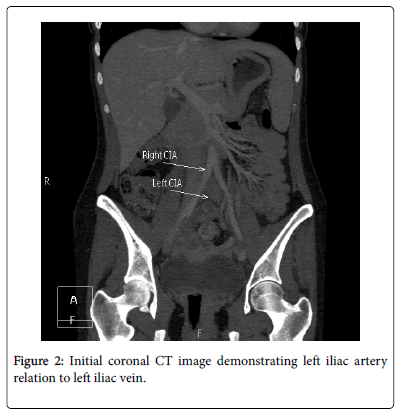
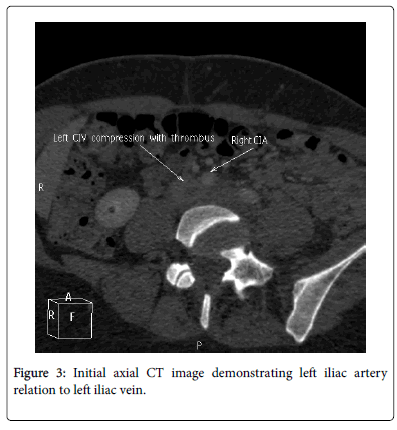
CT abdomen and pelvis with subsequent venography demonstrated isolated extensive left common and external iliac veins clot burden due to an external compression rather than intramural thrombosis (Figures 1-3).
Hematological tests including complete blood count (CBC), coagulation screenings were normal and thrombophilia screening was negative.
The duration of symptoms of acute DVT in our patient was 6 days. Initially a retrievable inferior vena cava filter was placed using contralateral femoral approach. Staged catheter-directed thrombolysis treatment was then performed for two days, resulting in partial resolution of thrombus with persistent stenosis.
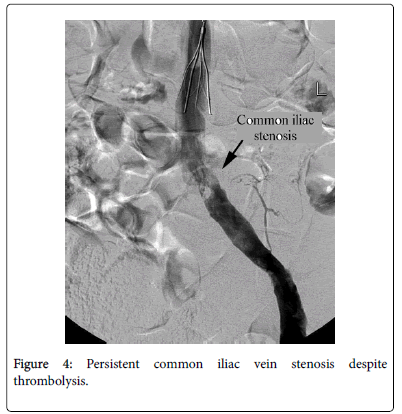
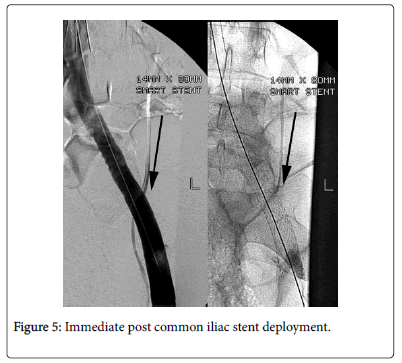
On the third day, a pelvic venogram revealed partial compression of left common and external iliac veins consistent with MTS (Figure 4). Left common and external iliac veins were angioplastied then stented with a self-expanding stent (Figure 5) with no immediate complications.
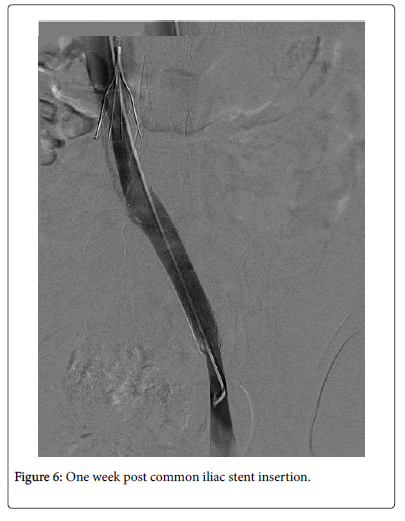
Patient was discharged home the following day on therapeutic low molecular heparin. One week later, she had uncomplicated IVC filter retrieval and a venogram showing patent iliac stent (Figure 6).
Warfarin was gradually introduced and continued for six month. Subsequently, clopidogrel was given as life-long medication. OCP was switched to another contraception method. Leg swelling and oedema resolved with one-year follow up duplex scan showed patent iliac veins and patient remained asymptomatic.
Discussion
Iliac vein compression is a frequent anatomic variant and is incidentally encountered on a few cross-sectional imaging studies. More than 50% luminal compression of the left iliac vein can be seen in up to 25% of asymptomatic healthy individuals [6].
We believed that MTS occurred in this case as a result of intense exercise causing haemodynamic changes in venous flow or venous pressure, which was exacerbated by OCP intake leading to acute DVT.
The mainstay of treatment of proximal iliofemoral obstruction in acutely symptomatic patients, is catheter directed thrombolysis plus angioplasty [7].
Embolic event has been previously reported in MTS [8]. Thus we elected for prophylactic IVC filter placement prior to angioplasty to reduce risk of pulmonary embolism.
Despite angioplasty, residual iliac thrombosis and stenosis demanded further considerations. There is increase evidence of stenting and early aggressive treatment of proximal iliofemoral thrombosis with good medium to long-term patency rate (84%) [9]. of note, surgical correction of iliofemoral or caval obstruction options should only be reserved for patients in whom endovascular options have failed or not feasible [10]. Current evidence suggests that patients in whom thrombosis develops may be at higher risk for recurrent DVT. Post thrombotic syndrome has been reported in patient with MTS despite iliac stenting and therapeutic anti coagulation with low molecular weight heparin [11].
Other alternative options to warfarin include the use of noval oral anticoagulants (NOAC), also known as non-vitamin K antagonist anticoagulant. These include dabigatran etexilate, which inhibits thrombin, and rivaroxaban, apixaban, and edoxaban, which inhibit factor Xa. These agents are effective alternatives to vitamin K antagonist for the treatment and prevention of venous thromboembolism and for stroke prevention in atrial fibrillation and for the prevention of recurrent ischaemic events after acute coronary syndrome. Currently, there are no specific antidotes available for the NOACs, which can complicate the management of life-threatening bleeding. Furthermore, The NOACs have variable effects on commonly available routine tests of coagulation, which may complicate assessment of their anticoagulant activity [12].
One year follow up, our patient remained asymptomatic and left iliac vein was patent. This was in agreement with a prospective stent evaluation study of 15 patients with MTS with 80% remained asymptomatic over a medium follow up of 16 months. All three of the symptomatic patients (20%) were reported to have mild symptoms. Stent occlusions developed in two patients; one patient had mild oedema, and the other remained asymptomatic [13]. Learning point MTS is under reported yet the diagnostic accuracy is critical since it often afflicts young patients and requires endovascular management. We believe that combination of dehydration and OCP provoked the development of iliac vein thrombosis. This emphasizes the need for patient selection and follow-up protocol in those young patients to reduce such complications. Large registries are needed to define the optimal treatment strategy and follow up protocol.
References
- Gil Martín AR, Carreras Aja M, Arrieta Ardieta I, Labayen Azparren I (2014) [Cockett's syndrome, May-Thurner syndrome, or iliac vein compression syndrome]. Radiologia 56:e5-8.
- Kalu S, Shah P, Natarajan A, Nwankwo N, Mustafa U(2013) May-thurner syndrome: a case report and review of the literature. Case Rep Vasc Med.
- Patterson BO, Hinchliffe R, Loftus IM, Thompson MM, Holt PJE (2010) DVT: A New Era in Anticoagulant Therapy Indications for Catheter-Directed Thrombolysis in the Management of Acute Proximal Deep Venous Thrombosis. ArteriosclThrom Vas 30: 669-674.
- Musani MH, Matta F, Yaekoub AY, Liang J, Hull RD, et al. (2010) Venous compression for prevention of postthrombotic syndrome: a meta-analysis. Am J Med 123:735-740.
- Butros SR, Liu R, Oliveira GR, Ganguli S, Kalva S (2013) Venous compression syndromes: clinical features, imaging findings and management. Br J Radiol 86:20130284.
- Oguzkurt L, Ozkan U, Ulusan S, Koc Z, Tercan F (2008) Compression of the left common iliac vein in asymptomatic subjects and patients with left iliofemoral deep veinthrombosis. J Vasc Interv Radiol 19:366-370.
- Mousa AY, AbuRahma AF (2013) May-Thurner syndrome: update and review. Ann Vasc Surg 27:984-995.
- Rison RA, Helfgott MD (2013) Acute paradoxical embolic cerebral ischemia secondary to possible May-Thurner syndrome and an atrial septal defect: a case report. J Med Case Rep 7:172.
- Park JY, Ahn JH, Jeon YS, Cho SG, Kim JY, et al. (2013) Iliac vein stenting as a durable option for residual stenosis after catheter-directed thrombolysis and angioplasty of iliofemoral deep vein thrombosis secondary to May-Thurner syndrome. Phlebology 29: 461-470.
- Garg N, Gloviczki P, Karimi KM, Duncan AA, Bjarnason H, et al. (2011) Factors affecting outcome of open and hybrid reconstructions for nonmalignant obstruction of iliofemoral veins and inferior vena cava. J Vasc Surg 53:383-393.
- Ludwig B, Han T, Amundson D (2006) Postthrombotic syndrome complicating a case of May-Thurner syndrome despite endovascular therapy: case report and review. Chest 129:1382-1386.
- Husted S, de Caterina R, Andreotti F, Arnesen H, Bachmann F, et al. (2014) Non-vitamin K antagonist oral anticoagulants (NOACs): No longer new or novel Thromb Haemost. 111:781-782.
- Lamont JP, Pearl GJ, Patetsios P, Warner MT, Gable DR, et al. (2002) Prospective evaluation of endoluminal venous stents in the treatment of the May-Thurner syndrome. Ann Vasc Surg 16:61-64.
Relevant Topics
- Back Pain Diagnosis
- Cardiovascular Diagnosis
- Clinical Diagnosis
- Clinical Echocardiography
- COPD Diagnosis
- Diabetes Diagnosis
- Diagnosis Methods
- Diagnosis of cancer
- Diagnosis of CNS
- Diagnosis of Diabetes
- Diagnostic Products
- Diagnostics Market Analysis
- Heart diagnosis
- Immuno Diagnosis
- Infertility Diagnosis
- Medical Diagnostic Tools
- Preimplementation Genetic Diagnosis
- Prenatal Diagnostics
- Ultrasonography
Recommended Journals
Article Tools
Article Usage
- Total views: 15808
- [From(publication date):
December-2015 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 11150
- PDF downloads : 4658