Mayer-Rokitansky-Küster-Hauser Syndrome: About Two Cases
Received: 25-Aug-2023 / Manuscript No. roa-23-112424 / Editor assigned: 28-Aug-2023 / PreQC No. roa-23-112424 / Reviewed: 11-Sep-2023 / QC No. roa-23-112424 / Revised: 18-Sep-2023 / Manuscript No. roa-23-112424 / Published Date: 25-Sep-2023 DOI: 10.4172/2167-7964.1000485
Abstract
Rokitansky syndrome (MRKH) is a rare congenital disorder characterized by the absence of a uterus and at least the upper 2/3 of the vagina in women with normal development of secondary sexual characteristics. C’est une cause rare d’aménorrhée primaire qui reste le principal signe clinique. It is a rare cause of primary amenorrhea, which remains the main clinical sign. Diagnosis is based primarily on magnetic resonance imaging (MRI). We present two cases of MRKH who both consulted for primary amenorrhea, with secondary sexual characteristics present and well developed.
Keywords
Mayer-Rokitansky-Kuster-Hauser; primary amenorrhea; utero-vaginal aplasia; MRI
Introduction
Rokitansky or Mayer Rokitansky Küster Hauser syndrome, or Mullerian aplasia, or utero-vaginal aplasia is a congenital aplasia of the uterus and upper two-thirds of the vagina in women with normal development of secondary sexual characteristics and a normal karyotype (46, XX) [1, 2]. Its incidence is estimated at 1/4500. Two forms are described: isolated (type I), or associated with other malformations (type II); type I being the least frequent. The main clinical sign of MRKH is primary amenorrhea [3, 4].
We present two typical forms of MRKH type I syndrome in an 18-year-old woman and a 34-year-old woman with primary amenorrhea investigated by abdomino-pelvic ultrasound and pelvic MRI, which revealed complete agenesis of the uterus.
Case Presentation
Case 1:
18-year-old girl, followed for pubertal stage Hodgkin lymphoma with absence of menstruation; pelvic ultrasound revealed uterine agenesis.
Medical history shows onset of pubertal development at age 9 and thelarche at age 11. Apart from her known lymphoma ATCD, the patient was pain-free and had normal statural, weight and intellectual development, with well-developed secondary sexual characteristics (normal pubic and axillary hair and normal breast development).
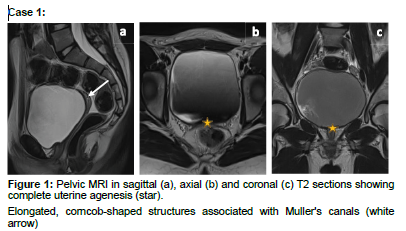
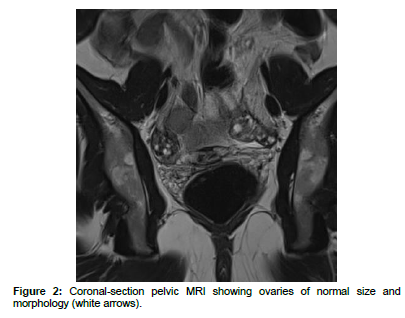
MRI confirmed the absence of uterus and cervix, associated with hypoplasia of the upper 2/3 of the vagina without focal lesion, continuing with structures laterally on both sides by a round ligament and fallopian tubes that are in T2 hypo signal elongated in the shape of an ear of corn in connection with Muller’s ducts (Case 1, Figure 1). The ovaries were of a size and morphology consistent with the patient’s age (right ovary measuring 31x19x30 mm, i.e. a volume of 8.8 ml and the left measuring 31x18x29xmm, i.e. a volume of 8.09 ml) (Case 1, Figure 2). A small amount of effusion is noted
Case 2:
34-year-old woman with primary amenorrhea and hymenal imperforation requiring pelvic ultrasound, which showed a hypoplastic uterus.
This primary amenorrhea is associated with monthly pelvic and lumbar pain exacerbated for more than two years. She has normally developed secondary sexual characteristics and normally developed external genitalia. Her hormonal profile was normal and her karyotype was 46 XX.
On physical examination, breasts and hair distribution were normal. No hirsutism or acne was noted.
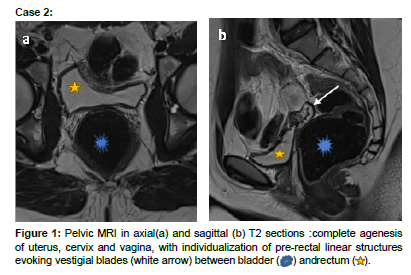
MRI revealed pre-rectal linear structures suggestive of remnants of the müllerian ducts with uterine, cervical and vaginal aplasia (Case 2, Figure 1). The ovaries are of normal size and morphology (Case 2, Figure 2).
As both patients were virgo intacta, vaginal examination was not performed.
Discussion
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome is defined by the presence of criteria for normal female secondary sexual development relating to the presence of functional ovaries associated with vaginal agenesis and uterine anomalies ranging from a rudimentary uterus to the complete absence of a uterus [5]. It was first described in 1829 by Mayer, who demonstrated partial and complete duplications of the vagina in four stillborn babies [4]. Of unknown etiology, this syndrome may result from early arrest of mullerian duct development in the seventh week of embryonic development. Although initially considered sporadic, familial cases have been reported and the hypothesis of a multigenic origin has been proposed [5]. Two clinical forms are described: MRKH type I, corresponding to isolated uterovaginal agenesis, and MRKH type II, the most widespread, characterized by incomplete agenesis and/or associated with other congenital malformations [1, 2]. It is the second most frequent cause of primary amenorrhea after gonadal dysgenesis [3]. Diagnosis is usually suspected at puberty, with the development of secondary sexual characteristics in the absence of menarche. The main clinical sign is primary amenorrhea with well-developed secondary sexual characteristics. In the diagnostic workup, assessment of sex hormones should be considered a basic element, as ovarian function is generally preserved with normal hormone levels (plasma FSH, LH and 17-estradiol). Chromosomal analysis should be performed to differentiate this syndrome from other syndromes presenting with primary amenorrhea [5, 6].
Ultrasound via the suprapubic approach is a first-line method, which allows the diagnosis to be suspected by showing the absence of a uterine structure between the bladder and the rectum [1]. Nevertheless, a quadrangular retrovesical structure may be misidentified as a hypoplastic uterus; it corresponds to the vestigial lamina located under the median part of the transverse peritoneal fold. In addition, any associated renal malformation should be systematically checked during this ultrasound examination [3]. This ultrasound study is useful for evaluating the genitourinary system and diagnosing any associated renal malformations.
MRI is a non-invasive technique that offers a more sensitive and specific means of diagnosis than ultrasound. A detailed map of the pelvic anatomy and morphology of the internal genitalia can be drawn up using the T2 sagittal and axial section sequence, confirming uterine aplasia and the upper two-thirds of the vagina, as well as clear visualization of the rudimentary horns, as in the first patient, and the normal appearance of both ovaries [7, 8]. Uterine aplasia is best characterized on sagittal images, while vaginal aplasia is best highlighted on axial sections. MRI can also be used to search for other associated malformations (kidney and bone).
Laparoscopy should be reserved for cases where there is diagnostic doubt after MRI. It shows the absence of the uterus, normal-looking ovaries, tubal remnants, the vestigial lamina under the median part of the transverse peritoneal fold and the uterosacral ligaments. Complementary examinations must be carried out depending on the associated malformations [3].
When a patient presents with primary amenorrhea and welldifferentiated secondary sexual characteristics, the differential diagnosis is first and foremost transverse vaginal atresia or septum; the diagnosis is confirmed by careful clinical examination and the presence of a uterus on imaging.
In WNT4 gene mutation syndrome, the phenotype is very similar to MRKH, with primary amenorrhea, uterovaginal aplasia and possibly renal malformation, but these anomalies are associated with signs of hyperandrogenism (acne and hirsutism), correlated by plasma assays showing elevated testosteronemia.
Androgen insensitivity syndrome, a pseudo hermaphroditic male. The phenotype is female, with testes in the abdominal or inguinal position and a high testosterone level equivalent to that of the male subject [2, 4, 6].
Typical MRKH syndrome includes isolated forms of congenital agenesis of the vagina and uterus; however, cases of anomalies associated with type I have been reported, including renal ectopy, bifid kidney, renal aplasia and even bone aplasia. Polycystic ovaries, even ectopic ones, and ovarian tumours have been described, as well as rare cases of association with gonadal dysgenesis [3, 9]. Our two patients had no other associated abnormalities
Conclusion
Although a rare condition, MRKH syndrome is the second most common cause of primary amenorrhea. It should be suspected in the presence of primary amenorrhea in a young woman with well-developed sexual characteristics. Diagnosis is based primarily on imaging, notably ultrasound and pelvic MRI. The association with other malformations is frequent and should be systematically investigated in order to provide a roadmap for surgical planning.
References
- Mohamed Abdellaoui, Jamal El Fenni, Meryem Edderai (2021) Le syndrome de Mayer-Rokitansky Küster-Hauser comme cause d'aménorrhée primaire à propos d'un cas. Pan Afr Med J 40: 260.
- Morcel K, Guerrier D, Watrin T, Pellerin I, Levêque J (2008) The Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: clinical description and genetics. Journal de Gynécologie Obstétrique et Biologie de la Reproduction 37: 539-546.
- El Khamlichi A, Allali N, Dafiri R (2011) Forme typique du syndrome de Mayer- Rokitansky-Küster-Hauser et rein ectopique: association rare. Gynécologie Obstétrique & Fertilité Tome 39, Numéro 2, Février , Pages e40-e43.
- Valeria Fiaschetti, Amedeo Taglieri, Vito Gisone, Irene Coco, Giovanni Simonetti (2012) Mayer-Rokitansky-Kuster-Hauser : Syndrome diagnosed by Magnetic Resonance Imaging. Role of Imaging to identify and evaluate the uncommon variation in development of the female genital tract. Obstetric & Gynecologic Radiology 6: 17-24.
- Schwaab T, Bryand A (2019) Place de l’échographie dans la prise en charge du syndrome de Mayer-Rokitansky-Kuster-Hauser. Gynécologie Obstétrique Fertilité & Sénologie 47: Pages 783-789.
- Laura Londra, Farah S Chuong, Lisa Kolp (2015) Mayer-Rokitansky-Kuster-Hauser syndrome : a review. International Journal of Women’s Health 7: 865–870.
- Folch M, Pigem I, Konje JC (2000) Mullerian Agenesis: Etiology, Diagnosis, and Management. Obstetrical & Gynecological Survey 55: 644–649.
- Troiano RN, Mc Carthy SM (2004) Mullerian duct anomalies: imaging and clinical issues. Radiology 233: 19–34.
- Marrakchi A, Gharbi MH, Kadir A (2004) Association dysgénésie gonadique et syndrome de Rokitansky Kuster Hauser: à propos d’un cas. Annales d'endocrinologie vo l 5: 466-468
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Rostoum S, Kessi EM, Zhim M, Soukaina EA, Naggar A, et al. (2023) Mayer-Rokitansky-Küster-Hauser Syndrome: About Two Cases. OMICS J Radiol 12: 485. DOI: 10.4172/2167-7964.1000485
Copyright: © 2023 Rostoum S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1191
- [From(publication date): 0-2023 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 979
- PDF downloads: 212