Research Article Open Access
Maxillofacial Aneurysmal Bone Cysts in Isfahan 1987-2013: A Clinicohistopathological Study of 16 Cases
Mohammad Hosein Kalantar Motamedi1* Ali Ebrahimi2, Ahmad Behroozian3, Neda Kargahi4, Hamid Reza Rasouli5 and Ali Shams Nouraie5
1Professor of Oral & Maxillofacial Surgery, Trauma Research Center, Baqiyatallah University of Medial Sciences, Tehran, Iran
2Associate Professor, Plastic Surgery Ward and Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
3Private Practice Orthodontist, Trauma Research Center, Baqiyatallah University of Medial Sciences, Tehran, Iran
4Assistant Professor, Torabinejad Dental Research Center and Department of Oral and Maxillofacial Pathology, School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran
5Consultant Researcher, Trauma Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
- *Corresponding Author:
- Mohammad Hossein Kalantar Motamedi
Professor of Oral & Maxillofacial Surgery
Trauma Research Center
Baqiyatallah University of Medial Sciences
Tehran, Iran
Tel: 982188053766
Fax: 982188053766
E-mail: motamedical@yahoo.com
Received Date: July 21, 2014; Accepted Date: July 29, 2014; Published Date: August 04, 2014
Citation: Motamedi MHK, Ebrahimi A, Behroozian A, Kargahi N, Rasouli HR, et al. (2014) Maxillofacial Aneurysmal Bone Cysts in Isfahan 1987-2013: A Clinicohistopathological Study of 16 Casest. Oral Hyg Health 2:155. doi: 10.4172/2332-0702.1000155
Copyright: © 2014 Motamedi MHK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Purpose: This study aimed to assess the prevalence, demographics, clinicohistopathological features and treatment outcomes of maxillofacial aneurysmal bone cysts (ABCs) in Isfahan.
Materials and method: A unicenter retrospective study of patient charts dated from 1987-2013 (26 years) was undertaken to assess maxillofacial ABCs. Variables such as age, gender, location (maxilla, mandible, anterior or posterior segments), histological type (solid, mixed, vascular), signs, symptoms, radiographic features ,treatment modalities and outcomes of this lesion were evaluated by the authors. The data was analyzed using SPSS 20 software (p<0.05).
Result: 16 patients were diagnosed and treated in our study, which included 6 (37.5%) males and 10 (62.5%) females. There was a significant female predilection (p<0.05). The mean age of occurrence was16.2 ± 7.9 years ranging from 6 to 28 years.The prevalence was not significantly higher in any decade of life. The rate of affliction was 0.6 case per year. ABC was significantly more common in the mandible (p<0.05) and the posterior areas (p<0.05). The most common histopathological type was the mixed type (p<0.05).Bony hard Swelling was the most common clinical finding (p<0.05) and all cases were radiolucent. All cases were treated with excision and curettage. Two patients (12.5%) showed recurrence during the follow-up period (1-26 years).There was no relationship between recurrence and other parameters.
Conclusion: ABCs of the jaws are rare lesions with variable presentation and often respond well to excision and curettage. Apparently it seems that there is no need to do more aggressive surgery because recurrence is low.
Keywords
Aneurysmal bone cysts (ABCs) ; maxillofacial; epidemiology
Introduction
The aneurysmal bone cyst (ABC) is an enigmatic and misnamed lesion displaying variable etiopathogenic, histologic and radiographic characteristics [1-3]. Actually the ABC is a pseudocyst because it has no epithelial lining [3]. It can be categorized as giant cell lesion that contains caverns or blood clefts [3-7] and is most commonly found in long bones and vertebra [8]. Only 1.9% of ABCs occur in the jaws [9]. Jaffe and Lichtenstein [2] first recognized the ABC in1942. Bernier and Bhaskar in 1958 reported the first ABC of the jaws [10]. Since then, many reports of ABCs have been published with varying clinicopathological characteristics. Although ABC has been reported in almost all of the craniofacial bones (i.e. zygoma, occipital, ethmoid, temporal, etc.) [11-15] they are most commonly found in mandible especially in the posterior areas .The involvement ratio of the mandible to maxilla is 3 to 1 [16,17]. The radiographic features are not pathognomonic. The lesion may appear as a unicystic ,soap bubble, or moth-eaten causing expansion, perforation or destruction of bony cortices [3,5,18-20]. A case with “sun-ray” appearance has also been reported [21]. According to previous studies most cases of maxillofacial ABCs are more likely to present in the first two decades of life [16]. The clinical course of ABC is also confusing and may range from a self-limited lesion to an aggressive, rapidly destructive lesion similar to malignancies [1,17,18]. ABCs may manifest as a swelling that has been dormant or developed rapidly. Pain has been reported in the latter. On occasion, paresthesia, malocclusion, mobility, tooth migration or root resorption may be encountered. Maxillary lesions may involve the nasal and sinus cavities [22]. Treatment of the ABC is generally directed towards complete removal of the lesion. Complete excision is difficult in multilocular lesions the majority of cases respond well to this technique and recurrence can be attributed to incomplete removal of the lesion [6,16,21]. We sought to assess and analyze clinicohistopathological data of maxillofacial ABCs in Isfahan, Iran.
Materials and Methods
The authors retrospectively assessed patient charts at the maxillofacial surgery and pathology departments of Isfahan University of Medical Sciences; data of all patients with a definitive histopathological diagnosis of ABC (permanent histopathological report) treated from 1987-2013 were assessed. Patient charts of all cases including pathology reports and histories were also assessed. The patients that did not have definitive diagnosis of ABCs were excluded from the study. The age, sex, site (maxilla, mandible, anterior, posterior), histological type (solid, mixed, vascular), signs, symptoms, and outcomes (treatment modal, recurrence) of this lesion were evaluated by the authors (OMF surgeons and OMF pathologists). After registering the relevant data comprehensively in specific data collection sheets, the Kolmogrov- Smirnov test was used to see whether the distribution of variables was normal or not. According to this appropriate test established using SPSS 20 software (SPSS, Chicago, IL, USA).A p-value less than 0.05 was considered significant.
Results
We found 16 cases diagnosed and treated for ABCs during a 26- year period (1987-2013) the patients included 6 (37.5%) males and 10 (62.5%) females. There was as significant predilection to female gender (P<0.05). The mean age of occurrence was 16.2 ± 7.9 years (6 to 28 years) and our analysis showed that ABCs are not more common in any certain age group. The prevalence was 0.6 cases per year.
Involved bone
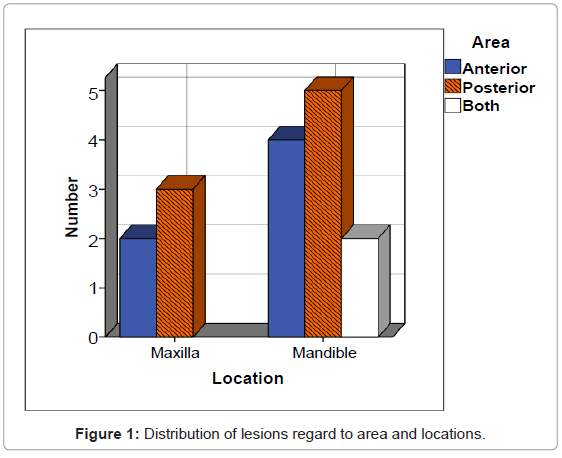
In 68.8% (n=11) of cases the mandible was involved and in 31.2% (n=5) ABC was found in maxilla. ABC was significantly more common in the mandible (P<0.05). In all of cases, the lesion occurred in the body and alveolar process of maxilla and mandible. Namely In our sample we did not find any involvement of the coronoid process, condyle, zygomatic process or ramus. Posterior segment involvement was found in 50% (n=8) of cases and 37.5% (n=6) of cases were found in anterior segment (P<0.05). In 12.5%, (n=2) of cases both anterior and posterior segments were involved. Figure 1 shows the distribution of lesions based on area and location.
Clinical findings
Bony hard swelling was present in 50% (n=8) of cases (p<0.05). Pain and simultaneous swelling were also documented.
Histopathological features
We found the mixed and solid patterns in 75% (n=12) and 18% (n=3) respectively. There was no Vascular patterns among cases and in 1 case, histopathologic type was not documented. The mixed type was the most common histopathological pattern (P<0.05). Associated lesions were also seen in one case that ABC was associated with central giant cell granuloma. There was no relationship between histopathologic type and other parameters like clinical course and recurrence rate.
Treatment and recurrence
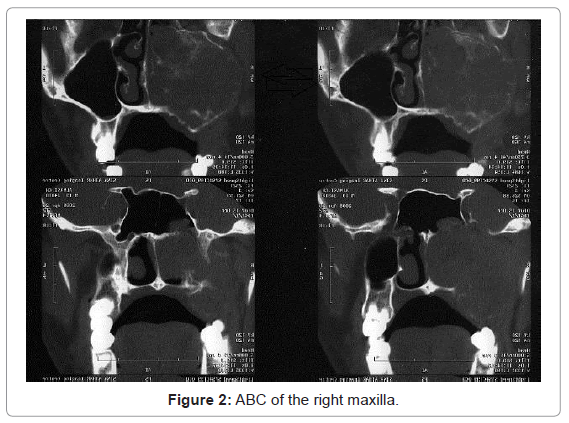
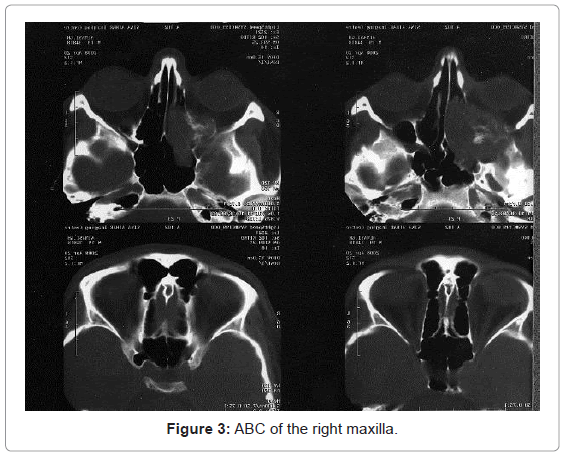
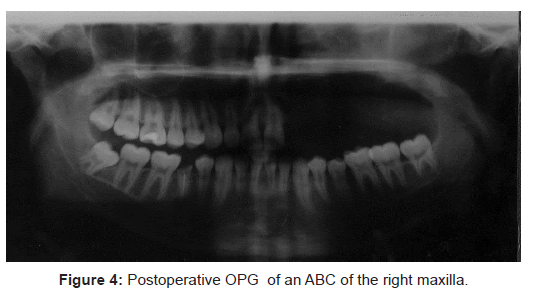
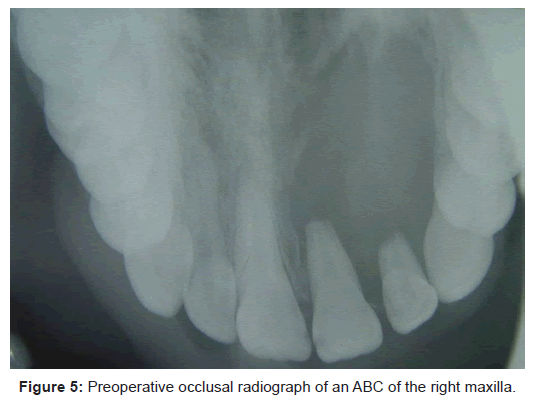
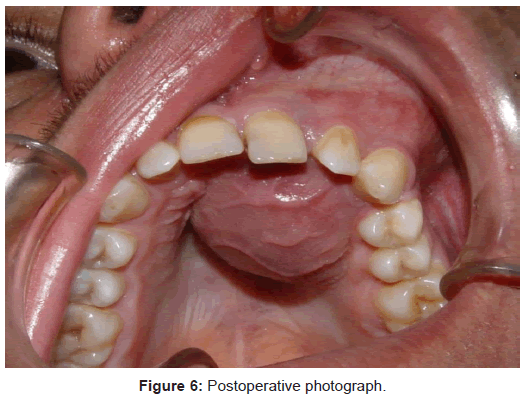
Excision and curettage was the treatment rendered in all cases and in 87.5% (n=14) the treatment was successful, (p<0.05). Ct scans and radiographs were used for diagnosis (Figure 2-6). Recurrence was reported in 2 patients (12.5%) during the follow-up period (1-26 years) who were retreated via re-curettage, resection.
Discussion
This retrospective study was done from 1987-2013 and sought to assess ABCs at the Isfahan University of Medical Sciences. ABCs are most commonly found in long bones and vertebral column [8]. Only 1.9% of ABCs occurs in the jaws [9]. Most of articles about ABC are sporadic case reports. In the present study we found 16 cases occurring during 26 years (0.6 cases per year). There was no report of Maxillofacial ABCs in Isfahan in the literature to date. In ABCs of the other parts of the human skeleton the vast majority (approximately 80%) of primary ABC patients are less than 20 years old [23]. Likewise ABCs of the jaws are more prevalent in first two decades of life [16]. We may conclude that ABCs generally affected young people, under the age of 20. This was confirmed in our study also by a mean of 16.2 years. In ABCs of the other parts of the human body, females are affected slightly more often than males [16,23]. We found similar results in our study. The so-called aneurysmal bone cyst is neither a cyst nor a neoplasm; it is not aneurysmal because there is no endothelial lining, rather it is probably an intraosseous arteriovenous malformation, sometimes seen in association with other well-known benign lesions [4,24]. We encountered one case associated with CGCG. Originally described by Jaffe and Lichtenstein in 1942 following articles by each [2,25-27], showed ABC was sufficiently characteristic to classify it as a distinctive pathologic entity. We found ABCs were significantly more common in the mandible than the maxilla. Also we found that the lesion is more prevalent in the posterior areas of the both jaw areas consistent with other studies [6,16,18].
Histopathology
In microscopic view, no kind of epithelial lining can be can be seen, so ABC can be called a pseudocyst rather than true cyst [28]. The characteristic microscopic view of ABC includes blood filled caverns or sinusoids within fibrous connective tissue stroma in variable amounts and multinucleated giant cells. In some cases hemosiderin and osteoid can be seen. The ratio of mentioned elements determines the histopathologic type of the ABC. In vascular type the stroma is loose and scant and unclotted blood-filled spaces that are separated by fibroblastic-not epithelial or endothelial-septa is the dominant view. In contrast ,the solid type consist of dense fibrous stroma and scanty blood filled spaces. The mixed type lies between these 2 extremes [16]. In our study the mixed type was the most common (75%) and solid type comprised 18% of ABCs and there was no vascular type. In one case the histopathologic type was not mentioned clearly. According to the nature of the ABC and its similarity to some other lesions less invasive methods like fine-needle aspiration cannot be helpful in definitive diagnosis although aspiration of a dark red or brownish hemorrhage fluid favors the diagnosis of ABC. Biopsy is the sole definitive diagnostic tool for ABC [29]. The etiology of ABC is unknown, it can be develop de novo or as a secondary lesion that arises within a previous bone cyst or within a pre-existing intrabony vascular lesion [16]; a lot of conditions have been mentioned as predisposing, contributing or causative factors in formation of ABC (Table 1). Vascular malformations that predispose the region to hemodynamic impairment are mentioned in majority of studies and this is the most probable theory. Levy [30] stated that trauma can be an etiologic factor. His theory was based on hemodynamic disturbance of bone due to physical trauma. In our study only 6.3% (n=1) of cases had documented history of trauma; however, trauma is rarely recalled and often not documented. It was not a significant factor in predisposing the region to ABC. In agreement with our study Bataineh [28] found no patient with a history of trauma. Motamedi [16] that has published the largest sample of aneurysmal bone cyst of the jaws, did not report trauma history in his cases .One can say that trauma is not a major factor in ABC of the jaws, however we should keep in mind that history of trauma is not a well-documented criteria in the patients charts and it often is not recalled. Another possible theory is the different pathogenesis of the ABC s of the jaws and long bones. It is important to examine the whole tissue to exclude the associated additional pathologic processes [29]. The concept of aneurysmal bone cyst as a secondary phenomenon occurring in a preexisting lesion has been validated by multiple investigators; in approximately one third (29-35%) of cases that reported in long bones and vertebra some preexisting lesion can be identified [30,31-33]. The most common lesion is giant cell tumor, which accounts for 19-39% of those cases in which the preceding lesion is found .Other common precursor lesions include osteoblastoma, angioma, and chondroblastoma [30,31-33]. We found that in one of the cases, ABC was associated with CGCG lesions. In contrast to the other parts of the body, in ABCs of the jaws incidence of concomitant tumors is less and no accompanying malignancy has been reported. Martinez et al. [32] found that about 15% of all giant cell tumors will have areas of cystic change that resemble the aneurysmal bone cyst .We have no clear evidence to say these lesions precede ABC or vice versa. Vegrel [23] reported high histopathologic similarity between ABC and Central giant cell granuloma (CGCG) and stated that sometimes these lesions are indistinguishable. CGCG is more common in females and according to our study this is a common feature of CGCG and ABC, but in contrast with BAC, CGCG is more common in anterior segments of the jaws and normally occurs later than ABC [34,35]. As a conclusion ABC and CGCG are very similar lesions, but they have not necessarily cause and effect relationship .Knowing that the recommended treatment protocol is the same for these two, it does not matter clinically what the exact nature of the lesion is. We found the most common clinical manifestation of ABC to be swelling as in other studies [16,20,23,36]. This expansion may cause marked asymmetry of the face or penetration to the soft tissue or adjacent structures like nasal cavity or maxillary sinuses. Motamedi et al [16] related the clinical course to histopathological type; destructive, rapidly progressive lesions were attributed to vascular pattern and small localized lesions were attributed to the solid type. But we did not find any significant relationship between histopathologic type and clinical presentation. ABC is known as a benign condition .Indeed some cases of spontaneous regression have been reported in long bones [37]. Careful curettage and removal of entire lesion is the recommended protocol [5]. Others have proposed different treatment modalities like cryotherapy,openpacking, block resection and bone grafting and therapeutic embolization that may be considered regarding the volume, vascularity, anatomy position of the lesion and destruction of bony cortices [1,6,24,38-42] Motamedi et al [16] reported 84.4% success with excision and curettage. In long bones and vertebra the recurrence rate was 10-44 % of case, most of them reported within the first postoperation year [23,26,43,44]. Irradiation of the ABC is not advisable due to a high risk of sarcomatous change, Sanchez [45] reported 26-56% recurrence and most of these recurrences diagnosed the first postsurgical year. This high recurrence can be attributed to incomplete removal and inadequate access. Our success rate was 87.5% in 26 year fallow up that is similar to Motamedi’s [16] study. The higher success rate of our study compared with ABCs of long bones can partly be attributed to different nature of ABCs of the jaws. We found no statistical relationship between recurrence and other parameters like age, sex, and location, histologic, radiographic or clinical features. The most important limitation of our study was the incomplete patient charting, especially in clinical examination and history data and paucity of cases.
| Prresumed etiologies for ABC |
|---|
| Sub periosteal or intramedullary hemorrhage with misguided reparative processes as a result of trauma [30] |
| Vascular origin as a result of local circulatory disturbance [25,26] |
| secondary phenomenon due to a hemorrhagic “blow-out “ in a preexisting lesion [23] |
| Thrombosis of a sizable vein [25,26] |
| Chromosomal anomalies [31] |
| Familial predilection and genetics [23,32,33] |
Table 1: Etiologies for ABC.
Conclusion
Our study showed that ABCs of the jaws is more common in females, and in posterior segment of the mandible. The most clinical presentation was firm painless swelling. Most of the cases respond well to excision and curettage.
References
- Hernandez GA, Castro A, Castro G, Amador E (1993) Aneurysmal bone cyst versus hemangioma of the mandible. Report of a long-term follow-up of a self-limiting case. Oral Surg Oral Med Oral Pathol 76: 790-796.
- Jaffe HL, Lichtenstein L (1942) Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathological appearance and the pathogenesis. Arch Surg 44: 1004-1025.
- Shafer WG, Hine MK, Leyt BM (1983) A Textbook of Oral Pathology. Saunders, Philadelphia, 149-152.
- Marx RE, Stern D (2003) Oral and Maxillofacial Pathology: A Rationale for diagnosis and treatment. Chicago, IL, Quintessence.
- Laskin OM (1985)Oral and Maxillofacial surgery. St Louis, MO: Mosby 2: 477-478.
- Motamedi MH, Yazdi E (1994) Aneurysmal bone cyst of the jaws: analysis of 11 cases. J Oral MaxillofacSurg 52: 471-475.
- Steidler NE, Cook RM, Reade PC (1979) Aneurysmal bone cysts of the jaws: a case report and review of the literature. J Oral Surg 16: 254-261.
- Giddings NA, Kennedy TL, Knipe KL, Levine HL, Smith JD (1989) Aneurysmal bone cyst of the mandible. Arch Otolaryngol Head Neck Surg 115: 865-870.
- Eldeeb M, Sedano HO, Waite DE (1980) Aneurysmal bone cyst of the jaws. Report of a case associated with fibrous dysplasia and review of the literature. Int J Oral Surg 9: 301-311.
- Bernier JL, BHASKAR SN (1958) Aneurysmal bone cysts of the mandible. Oral Surg Oral Med Oral Pathol 11: 1018-1028.
- Mattei TA, Mattei JA, Ramina R, Aguiar PH (2005) Fibrous dysplasia in combination with aneurysmal bone cyst presenting as a subarachnoid haemorrhage. NeurolSci 26: 178-181.
- Sheikh BY, Kanaan I, Alwatban J, Enazi A, Patay Z (1999) Aneurysmal bone cyst involving the skull base: report of three cases. Skull Base Surg 9: 145-148.
- Hrishikesh KA, Narlawar RS, Deasi SB, Aniruddha K, Maheshwari S (2002) Case report: Aneurysmal bone cyst of the ethmoid bone. J Radiol 75: 916-918.
- Cakirer S, Cakirer D, Kabukcuoglu F (2002) Aneurysmal bone cyst of the orbit: a case of rare location and review of the literature. Clin Imaging 26: 386-391.
- Itshayek E, Spector S, Gomori M, Segal R (2002) Fibrous dysplasia in combination with aneurysmal bone cyst of the occipital bone and the clivus: case report and review of the literature. Neurosurgery 51: 815-817.
- Motamedi MH, Navi F, Eshkevari PS, Jafari SM, Shams MG, et al. (2008) Variable presentations of aneurysmal bone cysts of the jaws: 51 cases treated during a 30-year period. J Oral MaxillofacSurg 66: 2098-2103.
- Trent C, Byl FM (1993) Aneurysmal bone cyst of the mandible. Ann OtolRhinolLaryngol 102: 917-924.
- Motamedi MH, Khodayari A (1993) Aneurysmal bone cyst mimicking a malignancy. J Oral MaxillofacSurg 51: 691-695.
- Kershisnik M, Batsakis JG (1994) Aneurysmal bone cysts of the jaws. Ann OtolRhinolLaryngol 103: 164-165.
- Struthers PJ,ShearM (1984) Aneurysmal bone cyst of the jaws. Clinicopathological features and pathogenesis.Int J Oral Surg 30: 88-100.
- KalantarMotamedi MH (1998) Aneurysmal bone cysts of the jaws: clinicopathological features, radiographic evaluation and treatment analysis of 17 cases. J CraniomaxillofacSurg 26: 56-62.
- Neville BW, Damm DD, Allen CM, BONQUOT JE (2009) Oral and Maxillofacial pathology. (3th Edn) Elsevier Inc, St. Louis.
- Vergel De Dios AM, Bond JR, Shives TC, McLeod RA, Unni KK (1992) Aneurysmal bone cyst. A clinicopathologic study of 238 cases. Cancer 69: 2921-2931.
- Mirra JM (1989) Bone tumors: clinical, radiologic and pathologic correlations.Philadelphia, Lea&Febiger.
- Lichtenstein L (1950) Aneurysmal bone cyst. A pathological entity commonlymistaken for giant cell tumor and occasionally for hemangioma and osteogenicsarcoma. Cancer 3:279-289.
- Lichtenstein L (1953) Aneurysmal bone cyst; further observations. Cancer 6: 1228-1237.
- Jaffe HL (1950) Aneurysmal bone cyst. Bull Hosp Joint Dis 11: 3-13.
- Bataineh AB (1997) Aneurysmal bone cysts of the maxilla: a clinicopathologic review. J Oral MaxillofacSurg 55: 1212-1216.
- Tang IP, Shashinder S, Loganathan A, Anura MM, Zakarya S, et al. (2009) Aneurysmal bone cyst of the maxilla. Singapore Med J 50: e326-328.
- Levy WM, Miller AS, Bonakdarpour A, Aegerter E (1975) Aneurysmal bone cyst secondary to other osseous lesions. Report of 57 cases. Am J ClinPathol 63: 1-8.
- Biesecker JL, Marcove RC, Huvos AG, Miké V (1970) Aneurysmal bone cysts. A clinicopathologic study of 66 cases. Cancer 26: 615-625.
- Martinez V, Sissons HA (1988) Aneurysmal bone cyst. A review of 123 cases including primary lesions and those secondary to other bone pathology. Cancer 61: 2291-2304.
- Bonakdarpour A, Levy WM, Aegerter E (1978) Primary and secondary aneurysmal bone cyst: a radiological study of 75 cases. Radiology 126: 75-83.
- Neville BW, Damm DD, Allen CM, Bonquot JE (2009) Oral and Maxillofacial pathology. (3th Edn) Elsevier Inc, St. Louis, P: 640-645.
- Neville BW, Damm DD, Allen CM, Bonquot JE (2009) Oral and Maxillofacial pathology. (3th Edn) Elsevier Inc, St. Louis, P: 626.
- Kransdorf MJ, Sweet DE (1995) Aneurysmal bone cyst: concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol 164: 573-580.
- Sherman RS, SOONG KY (1957) Aneurysmal bone cyst: its roentgen diagnosis. Radiology 68: 54-64.
- Power RA, Robbins PD, Wood DJ (1996) Aneurysmal bone cyst in monozygotic twins: a case report. J Bone Joint Surg Br 78: 323-324.
- Motamedi MH (2002) Destructive aneurysmal bone cyst of the mandibular condyle: report of a case and review of the literature. J Oral MaxillofacSurg 60: 1357-1361.
- McQueen MM, Chalmers J, Smith GD (1985) Spontaneous healing of aneurysmal bone cysts. A report of two cases. J Bone Joint Surg Br 67: 310-312.
- Schreuder HW, Veth RP, Pruszczynski M, Lemmens JA, Koops HS, et al. (1997) Aneurysmal bone cysts treated by curettage, cryotherapy and bone grafting. J Bone Joint Surg Br 79: 20-25.
- Dahlin DC, McLeod RA (1982) Aneurysmal bone cyst and other nonneoplastic conditions. Skeletal Radiol 8: 243-250.
- Ruiter DJ, van Rijssel TG, van der Velde EA (1977) Aneurysmal bone cysts: a clinicopathological study of 105 cases. Cancer 39: 2231-2239.
- Matt BH (1993) Aneurysmal bone cyst of the maxilla: case report and review of the literature. Int J PediatrOtorhinolaryngol 25: 217-226.
- Sánchez AP, Diaz-Lopez EO, Rojas SK, Neri HA, Valle PL, et al. (2004) Aneurysmal bone cyst of the maxilla. J CraniofacSurg 15: 1029-1033.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 15109
- [From(publication date):
November-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10499
- PDF downloads : 4610