Maternal Risk Factors Associated with Term Low Birth Weight Infants at Government Health Clinics in Ipoh, Perak-A Case-Control Study
Received: 01-Jun-2020 / Accepted Date: 03-Sep-2020 / Published Date: 10-Sep-2020 DOI: 10.4172/2471-9846.1000247
Abstract
Birth weight is the first weight measured almost immediately or within the first hour after birth. Generally, birth weight is considered as a benchmark of reproductive health and general health status of the population. Low birth weight is a valuable public health indicator of maternal health, nutrition, healthcare delivery, and poverty. The World Health Organization (WHO), in 1992 recognized low birth weight (LBW) as a reliable indicator in monitoring and evaluating the success of maternal and child health programs and has been defined as a birth weight less than 2500 g.
Keywords: Birth weight; Health care; WHO; Public Health
Introduction
A birth weight of <2500 g or ≤ 2499 g is defined as Low birth weight (LBW) [1]. This practical cut-off for international comparison is based on epidemiological observations that infants weighing <2500 grams are approximately 20 times more likely to die than heavier babies by United Nations Children’s Fund (UNICEF) and World Health Organization in 2004 [2]. The same cut point has been applied in Malaysia by the Ministry of Health.
World health organization estimates that 25 million LBW babies are born annually worldwide and 95% occur in developing countries [3]. Globally, it is estimated that 15 to 20% of all births, or >20 million newborns annually, are low birth weight infants [4,5]. This 15% of births, however, accounts for some 60 to 80% of all neonatal deaths. Low and middle-income countries account for a disproportionate burden of LBW [6]. The largest contributions are coming from South Asia.
Regional estimates of LBW include 28% in South Asia, 13% in sub- Saharan Africa and 9% in Latin America [5]. It highlighted that the rates are high, in spite of data on high prevalence of low birth weight; the actual numbers remain unreliable as many deliveries occur at homes and conducted by untrained health professional especially in countries with poor healthcare accessibility [6]. These resulted in the gross underestimation of the prevalence of low birth weight. In addition, the LBW rates are unequal among different countries, depending upon many factors such as socioeconomic conditions, poor nutrition, education level, and health condition [7].
Low birth weight is a complex syndrome that includes preterm neonates (born before 37 weeks of gestation), small for gestational age neonates at term and the overlap between these two situations preterm and small for gestational age neonates, who typically have the worst outcomes.
These three groups have their own subgroups, with individual components linked to different causative factors and long-term effects, and distributions across populations that depend on the prevalence of the underlying causal factors [8]. Understanding and differentiating the various categories and their subgroups is an essential first step in preventing these conditions [9]. Socioeconomic conditions, poverty, education level, violence during pregnancy, and early marriages are also an essential contributing factor for low birth weight infants. Infectious agents have the potential to penetrate through the uterus and cause inflammations in uterus and placenta [10].
According to Report of National Health and Morbidity Survey (NHMS), by Jai et al. and UNICEF [10] as LBW is closely associated with foetal and neonatal mortality and morbidity, inhibited growth and cognitive development and development of chronic diseases later in life. Additionally, low birth weight is associated with longterm neurologic disability, impaired language development, impaired academic achievement, and increased risk of chronic diseases including cardiovascular disease and diabetes [6].
Problem Statement
Currently, the incidence rate of low birth weight at the national level and Kinta District seems to be plateau trend at around 11% for past few years (Table 1). Sutan, Mohtar, Mahat, & Tamil [11], in their study reported that the prevalence of LBW in the Malaysian population was 11.1% in 2011. The term low birth weight infants are 703 (63.6%) and 402 (36.7%) are preterm low birth infants at Kinta District in 2017.
| Year | Kinta District | Malaysia |
|---|---|---|
| 2014 | NA | 11.2% |
| 2015 | 11.6% | 11.53% |
| 2016 | 11.7% | 11.41% |
| 2017 | 11.8% | NA |
Table 1: Incidence of low birth weight infants.
The term low birth weight is predominant; this was coherent with other studies. The two aetiologies of low birth weight, preterm births and term low birth weight which were both causally associated with morbidity and mortality but through different pathways.
The recent endeavours to emphasize research on preterm births and term low birth weights birth are crucial for understanding the direct causes of mortality rather than low birth weight as a convenient surrogate.Malaysia adopted into its National Plan of Action for Nutrition of Malaysia III, 2016-2025 the target set in 2012, by the World Health Assembly Resolution 65.6 which was a comprehensive implementation plan on maternal, infant and young child nutrition. The policy brief covers the third target: a 30% reduction of low birth weight by 2025.
This plateau incidence pattern calls for further studies to be done to identify the root causes which of low birth weight in particular as low birth weight is still remain a significant health problem. Hence, Malaysia to be on par with the target set that is a <8.3% reduction of low birth weight by 2025, it definitely has to come up with good framework strategies, intervention and implementation.
Indeed; there was a room for research on term low birth weight and the associated factors. Certainly, there was an information gap to identify the predictors in the term birth weight separately as previous literature suggested the predictors for preterm and Small for Gestational Age (SGA) are different. So far; there are no studies on the risk factors associated with term low birth weight in Kinta District.
Significance of the Study
The study may provide and highlight the maternal risk factors associated with term low birth weight infants among the maternal who had antenatal care at government health clinics which can be used as a platform to prevent and control further incidences of low birth weight.
Research question
What are the determinants or maternal risk factors associated with term low birth weight infants in Kinta District?
Objectives
General objective
The objective of this study is to explore the socio-demographic and maternal risk factors especially the obstetric risk factors associated with LBW infants among maternal who had antenatal care at government health clinics in Ipoh. Perak, Malaysia.
Specific objectives:
To determine the associations between socio-demographic factors and term low birth weight infants
➢ age
➢ ethnic group
➢ education level
➢ marital status
➢ occupation
➢ smoking status
To determine the association between maternal risk factors and term low birth weight infants
➢ height at booking
➢ weight at booking
➢ body mass index (BMI)
➢ weight gain during pregnancy
➢ parity
➢ period of gestation at booking
➢ history of low birth weight
➢ birth spacing/interval
➢ number of visits for antenatal care
➢ pre-existing Hypertension
➢ pre-existing Diabetic Mellitus
➢ Pregnancy Induced Hypertension
➢ Gestational Diabetic Mellitus
➢ Anaemia in pregnancy
➢ To determine the correlation of term infants birth weight and the maternal age
➢ To determine the odds of delivering term low birth weight infant among maternal anaemia compared to mother without anaemia
Hypothesis
There is a significant correlation between infant birth weight and maternal age. The odds of delivering term low birth weight.is significantly higher in mother with anaemia than mother without anaemia
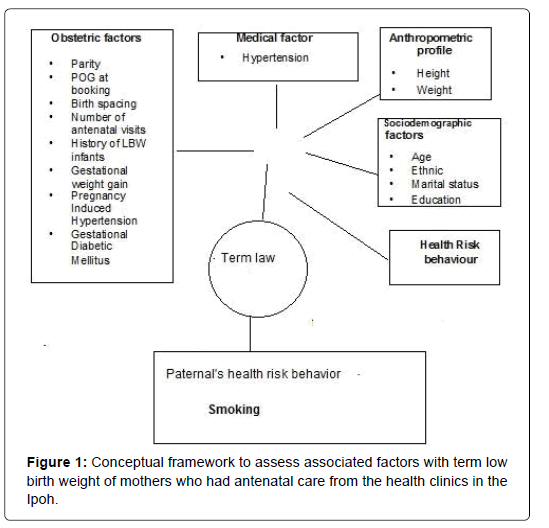
Conceptual framework
The conceptual framework for this study as illustrated (Figure 1). The framework shows the 2 main components will be focused, mothers social demographic, obstetric risk factors and followed the others such as medical, anthropometric measures, health risk behaviour like maternal smoking habit as well the paternal.
Materials and Methods
Overview
A matched case control study was conducted at government health clinics under the administration of Kinta District Health Office. All of the 9 health clinics located at Ipoh city, in Perak state, Malaysia. Ipoh is the third largest city in Malaysia.
The sample population was all deliveries from January to December 2017 from the operational areas of these 9 government health clinics. The information related to the study samples were retrospectively extracted from antenatal records kept at the Maternal and Child Health Unit of the government health clinics.
Study design
This was a case-control study carried out at government health clinics located at Ipoh area and its vicinities.
Study population: All live births delivered in one year period between 1 January 2017 and 31 December 2017, captured in statistics of the operational areas at 9 government health clinic.
Sample size: The sample size (case and control) determined by a free, web-based and open source; OPENEPI: A Webbased Epidemiologic and Statistical Calculator for Public Health. The sample size was ascertained based on the prevalence of 37.13% maternal who had anaemia delivered LBW and 62.87% maternal were non-anaemia in study at 2012 conducted by Karalasingam et al. In addition, the significance level set at 0.05 with power 80%, 95% Confidence Interval and ratio.
The sample size of cases and control derived were 45 and 89 respectively; the total samples are 134. The total samples for each clinic were 15 which are 5 cases and 10 controls. When there were not enough cases in one particular clinic, the number of cases taken from the next clinic increased to compensate.
Case definition: Woman who have delivered live birth, term infant with the period of gestation ≥ 37/52 period of gestation with birth weight <2500 g
Control definition: Woman who have delivered live birth, term infant with the period of gestation ≥ 37/52.
Criteria for matching: In this study, every control was matched for sex distribution with its corresponding case.
Inclusion criteria
➢ Malaysia citizen
➢ Women had obtained antenatal care until delivery at the government health clinics
➢ All types of childbirth
Exclusion criteria
➢ Multiple pregnancy
➢ iIncomplete data
Variables of the study
Dependent variable
➢ Birth weight of infant
➢ Independent variables
The independent variable studied in this research as shown in Table 2.
| No. | The conceptual definition of variables | Operational definition | Scale of measurement |
|---|---|---|---|
| 1 | Age | Maternal age at time registration for antenatal care. | completed years (continuous interval/ ratio and categorical– nominal) |
| 2 | Ethnic | ethnic of maternal | Malay/Chinese/Indian/ others(categorical-nominal) |
| 3 | Education | the level formal education maternal obtained |
primary, secondary and tertiary level of education (categorical-nominal) |
| 4 | Occupation | maternal job | employment status Yes/ No (categorical-nominal) |
| 5 | Marital status | current marital status of the maternal |
Married and unmarried, (categorical-nominal) |
| 6 | Smoking status woman/ Spouse | Smoking Behaviour for woman and spouse |
present of the condition (yes) /Absent (no) (categorical-nominal) |
| 7 | Height at booking | maternal height measured | centimetre (cm) (ratio scale) |
| 8 | Weight at booking | maternal weight during registration for antenatal care | maternal weight during registration for antenatal care kilogramme (kg) (ratio scale) categorical –ordinal) |
| 9 | Body Mass Index | Maternal body weight corresponding to maternal height at registration | kilogramme (kg) / meter2 (categorical data-ordinal) |
| 10 | Weight gain during pregnancy | Weight gained from registration day until the last check-up prior to delivery | kilogramme (kg) (ratio scale) / categorical -ordinal) |
| 11 | Parity | The number of previous births, including stillbirths | numeric (discrete)/ categorical -ordinal) |
| 12 | Period of gestation (POG) at booking | Number of weeks from the normal last menstrual period until registration day for antenatal care | numeric (discrete) booking( ≤ 12 weeks POG) and late booking (>12 weeks POG) (categorical data-ordinal) |
| 13 | The number of antenatal visits | The number of clinic visits from the maternal record as an indication of their utilization of antenatal care service. | Numeric (discrete) / Categorical-ordinal) |
| 14 | Birth spacing | Duration form date of the birth previous child until the first day last menstrual period this pregnancy | completed year and month (continuous interval/ ratio) (categorical-ordinal) |
| 15 | History of LBW infants | The number of previous birth of LBW infant. | (Categorical - nominal) |
| 16 | Maternal’s medical condition (selected only) | Pre-existing (before pregnancy) medical condition Diabetes Mellitus and Hypertension |
present of the condition (yes)/ Absent (no) of each condition (categorical- nominal) |
| Current medical condition developed during pregnancy which includes Gestational Diabetes Mellitus Pregnancy Induced Hypertension |
present of the condition (yes)/ absent (no) of each condition (categorical- nominal |
||
| Anaemia in pregnancy Haemoglobin level during the antenatal check-up period | Based on the reading <11 gram/decilitre (gm/dL) the cut off point for anaemia (categorical-nominal) |
Table 2: Framework of defining variables used to determine the association between predictor and low birth weight infants in this study.
Ethical Considerations
Ethical approval and clearance obtained from the Research Ethical Committee of Royal College Medical Perak– University Kuala Lumpur and Medical Research Ethics Committee (MREC) via registration with National Medical Research Registry (NNMR). The study was conducted after approval obtained from Director of Perak Health Department and Kinta District Health Office.
Data collection and Analysis
Data collection sheet was developed based on variables and other relevant information to ascertain the possible risk factors of LBW. The content of the data collection sheet was examined by a content expert.
The segregated cards were grouped into cases and controls chosen by simple random sampling (Figure 2).
The data was checked thoroughly for consistency and completeness after collection and then cleaned, edited, and verified to exclude any error or inconsistency. Statistical analysis was performed using the Statistical Package for Social Science (SPSS) software for Windows (version 23).
Results
Description of the population
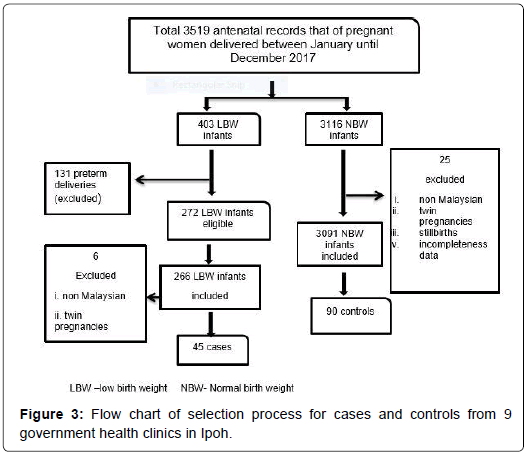
The numbers of the study population were 3519 pregnant women who were registered with the 9 government health clinics in Ipoh and had antenatal care until delivery between the months of January to December in 2017. Among these maternal, 3116 (88.5%) delivered normal birth weight (NBW) infants and 403 (11.5%) delivered low birth weight (LBW) infants. The number of low birth weight infants when further segregated into term low birth weight infants were 272 (67.5%) and preterm birth weight infants were 131 (32.5%) Figure 3.
Description of the maternal characteristics
The majority of maternal were Malays; 92 (68.1%) followed by Indian; 24 (17.8%), Chinese 17 (12.6%) and others 2 (1.5%). The samples or maternal were preponderance at the age between 18 to 40 years and almost all 133 (97.8%) were married. More than half of them; 71 (52.6%) were employed and 124 (91.9%) had education at secondary level and above. There was one smoker 1 (0.7%) among the pregnant women. Spouses of the maternal approximately half of them smoke; 68 (50.4%) (Table 3).
| Variables n (%) | n=135 |
|---|---|
| Ethnic | |
| Malay | 92 (68.1) |
| Chinese | 17 (12.6) |
| Indian | 24 (17.8) |
| Others | 2 (1.5) |
| Age (years) | |
| <18 | 2 (1.5) |
| 18-40 | 131 (97.0) |
| >40 | 2 (1.5) |
| Martial status | |
| Married | 132 (97.8) |
| Unmarried | 3 (2.2) |
| Employment | |
| Yes | 71 (52.6) |
| No | 64 (47.4) |
| Education | |
| Primary | 12 (8.1) |
| Secondary | 79 (59.3) |
| Tertiary | 44 (32.6) |
| Smoking status | |
| Maternal | |
| Yes | 1 (0.7) |
| No | 134 99.3 |
| Paternal | |
| Yes | 68 (50.4) |
| No | 64 (47.4) |
| Other (unmarried) | 3 (2.2) |
Table 3: Descriptive statistics of socio demographic.
The maternal parameter in continuous variables as illustrated below in Table 4. In this study there were no significant association of the continuous variables found between cases and controls.
| Variables | Case | 95% Cl | Control | 95% Cl | p-value |
|---|---|---|---|---|---|
| Maternal age at booking | 28.04 (5.64)* | 26.35, 29.74 | 29.00 (5.58)* | 28.03, 30.37 | 0.263 |
| Maternal height | 1.57 (0.59)* | 1.55, 1.58 | 1.58 (0.53)* | 1.56, 1.59 | 0.250 |
| Maternal Weight at booking | 55.90 (14) ** | 54.98, 62.50 | 60.95 (18.5)** | 58.26, 64.73 | 0.375 |
| BodyMass Index (BMI) at booking | 22.39 (7.4)** | 22.56, 25.40 | 23.95 (7.1)** | 23.47, 26.12 | 0.582 |
| Weight gain during pregnancy | 8.00 (7.1)** | 7.69,11.01 | 9.00 (5.2)** | 8.67, 10.59 | 0.449 |
CI: Confidence IntervalL p value: < 0.05 as significant
Table 4: Distribution for continuous variables of maternal in both groups.
Description of the infants
The infants constituted of 72 (53.3%) males and 63 (46.7%) females. The weight of infants with low birth weight (cases) ranged from 1570 g until 2450 g and median of 2300 g with IQR: 300 g. Moreover, the weights of normal birth weight infants (controls) ranged from 2500 g until 4000 g and median of 3000 g with IQR: 400 g.
The measure of association between social demographic variables of cases and controls.
The socio demographic and risk behaviour of both groups were compared as illustrated below in Table 5.
| Variables | Case | 95% Cl | Control | 95% Cl | p-value |
|---|---|---|---|---|---|
| Birth weight | 2300 (300) | 2180, 2299 | 3000 (400) | 2942, 3081 | 0.0001 *** |
Table 5: Distribution of infants’ birth weights in both groups.
Description of maternal obstetric risk factors
Generally, 82 (61%) were multiparas among the maternal. The numbers of maternal who did early booking were 93 (68.8%). They were 27 (20%) of them had less than 2 years birth spacing meanwhile; 46 (34%) had recommended spacing that is 2 to 5 years. Those maternal had a previous history of low birth infants in term pregnancy were 14 (10.3%) The number of maternal who had pre-existing hypertension was merely 2 (1.5%) and pre-existing Diabetic Mellitus were 3 (2.2%) of them. There were 20 (14.8%) maternal had Gestational Diabetic Mellitus and 3 (2.2%) had Pregnancy Induced Hypertension. Anaemia in pregnancy condition had become the most common medical problem among them; 59 (43.7%) (Table 6).
| Variables | Cases (n) % n=45 | Controls (n )% n=90 | p value | |||
|---|---|---|---|---|---|---|
| Ethnic | ||||||
| Malay | 31 | (68.9) | 61 | (67.8) | - | |
| Chinese | 4 | (8.9) | 13 | (14.4) | - | |
| Indian | 9 | (20) | 15 | (16.7) | - | |
| Others | 1 | (2.2) | 1 | (1.1) | - | |
| Age (years) 1.000 | ||||||
| <18 | 0 | 0 | 2 | (2.2) | - | |
| 18 -40 | 44 | (97.8) | 87 | (96.7) | - | |
| >40 | 1 | (2.2) | 1 | (1.1) | - | |
| Marital status 1.000 | ||||||
| Married | 44 | (97.8) | 88 | (97.8) | - | |
| Unmarried | 1 | (2.2) | 2 | (2.2) | - | |
| Employment 0.903 | ||||||
| Yes | 24 | (53.3) | 47 | (52.2) | - | |
| No | 21 | (46.7) | 43 | (47.8) | - | |
| Education 0.026 *** | ||||||
| Primary | 8 | (17.7) | 4 | (4.4) | - | |
| Secondary | 21 | (46.6) | 58 | (64.4) | - | |
| Tertiary | 17 | (37.7) | 28 | (31.2) | - | |
| Smoking status | ||||||
| Maternal | ||||||
| Yes | 0 | (0) | 1 | (1.1) | - | |
| No | 45 | (100) | 89 | (98.9) | - | |
| Spouse 1.000 | ||||||
| Yes | 23 | (51.1) | 45 | (50) | - | |
| No | 21 | (46.7) | 43 | (47.8) | - | |
| (unmarried) | 1 | (2.2) | 2 | (2.2) | - | |
Table 6: Association socio demographic and risk behaviour variables of cases with controls.
The measure of association of maternal obstetric risk factors with cases and controls
The variables such as parity, birth spacing, and history of term low birth weight, the period of gestation at booking and medical conditions were tested for statistical association with LBW using the Pearson Chi- Square Test and Fisher Exact Test. There were no significant difference maternal obstetric risk factors in between cases and controls except for a history of term low birth weights with p<0.05 (Table 7).
| Variables | Cases n (%) n=45 | Controls n (%) n=90 | p-value |
|---|---|---|---|
| Parity 0.456 | |||
| Primipara | 20 (44.5) | 34 (37.8) | - |
| Multipara | 25 (55.5) | 56 (62.2) | - |
| Birth spacing (years) | 0.717 | ||
| First birth | 20 (44.5) | 34 (37.8) | - |
| <2 | 9 (20) | 18 (20) | - |
| ≥ 2 | 16 (35.5) | 38 (42.2) | - |
| History of LBW in previous term deliveries | 0.040*** | ||
| First birth *(exempted) | 20 (44.5) | 34 (37.8) | - |
| Term LBW | 10 (22.2) | 5 (5.5) | - |
| Preterm LBW | 1 (2.2) | 4 (4.4) | - |
| No history of LBW | 14 (31.1) | 47 (52.2) | - |
| Period of Gestation (POG) at booking | 0.430 | ||
| ≤ 12 weeks POG | 33 (73.3) | 60 (67.7) | - |
| >12 weeks POG | 12 (26.7) | 30 (33.3) | - |
| Medical complications 1.000 | |||
| Pre-existing Hypertension | |||
| Yes | 1(2.2) | 1 (1.1) | - |
| No | 44 (97.8) | 89 (98.9) | - |
| Diabetic Mellitus 1.000 | |||
| Yes | 1(2.2) | 2 (2.2) | - |
| No | 44 (97.8) | 88 (97.8) | - |
| Pregnancy Induced Hypertension | 0.258 | ||
| Yes | 2 (4.4) | 1 (1.1) | - |
| No | 43 (95.6) | 88 (98.9) | - |
| Gestational Diabetic Mellitus | 0.870 | ||
| Yes | 10 (22.1) | 10 (11.1) | - |
| No | 35 (77.9) | 80 (88.9) | - |
| Anaemia in pregnancy | 0.393 | ||
| Yes | 23 (51.1) | 39 (43.3) | - |
| No | 22 (48.9) | 51 (56.7) | - |
Table 7: Distribution and association of the maternal obstetric risk factor with cases and controls.
The magnitude of the association selected variables
The two variables which significantly associated with LBW were the education level and history of term low birth weight tested in Binomial Regression Model (Table 7). The binomial logistic regression was for the primary education level and secondary level as reference with low birth weight. The result were logistic regression model was statistically significant; X2(1)=6.141, p=0.013. The model explained 6.2% or the variance of low birth weight and correctly classified 68.1% of cases (Table 8).
| Variables | OR | 95% CI | p-value | Logistic regression Model | R2 | |
|---|---|---|---|---|---|---|
| X2 | p-value | |||||
| Primary education | 4.649 | 1.318, 16.398 |
0.017 | 6.141 | 0.013 | 0.062 |
| History of LBW | 2.912 | 1.106, 7.664 |
0.030 | 4.692 | 0.030 | 0.047 |
Table 8: Measure of association the significant predictors with case and controls.
Maternal with primary education level was significantly associated with delivering of low birth weight infants than maternal with higher education levels; OR; 4.649, (95% CI; 1.318, 16.398), p<0.05. Maternal with primary level of education had 4.65 times higher odd to have low birth infants than the maternal whom had secondary and above level of education.
Maternal who had the previous history of LBW infants was significantly associated with delivering of low birth weight infants than the maternal who did not have the previous history of LBW infants. The logistic regression model was statistically significant; X2(1)=4.692, p=0.030. The model explained 4.7% or the variance of low birth weight infants and correctly classified 66.7% of cases.
The maternal with the previous history of low birth weight infants were associated with low birth weight infants also statistically significance; (OR; 2.912, 95% CI; [1.106, 7.664], p < 0.05). The maternal with the previous history of low birth weight had 2.91 times higher odd to have low birth weight than maternal who do not have history low birth weight infants. (Table 8) The multivariate logistic regression analyses for these two predictors were statistically insignificant with p>0.05.
The first hypothesis of this study: Maternal age have correlations with the probability to deliver infants with low birth weight (LBW) was tested by Nonparametric Correlations test or Spearman's correlation test. It showed that the Spearman’s rank correlation coefficient (Spearman’s rho) is 0.59 and p a value was 0.49. It means that the correlation was not statistically significant. Therefore, the hypothesis was rejected.
The second hypothesis was maternal with anaemia are more likely to have low birth weight (LBW) compared to non-anaemic maternal. This hypothesis was tested Pearson’s chi-square (X2). Asymptotic Significance (2-sided) had elicited p-value >0.05 in other words, it was not statistically significant. Therefore, the hypothesis was rejected.
Discussion
Incidences of Low Birth Weight
The incidence rate of low birth weight infants at all the 9 government health clinics in 2017 were 12.5%; enabled to be calculated by the collection process of all the antenatal records for selection of cases and controls. The Kinta District’s incidence rate at same year was around 11.8% based on the Kinta District Health Census, 2017 and at national level was 11.4% in as reported in NHMS 2016. The present study’s finding, on incidence rate of low birth weight is almost similar to the district and national level.
Distribution of term low birth weight
The trend distribution of term low birth weight was higher compared to preterm low birth weight at these 9 government health clinics 272 (67.5%) similar to Kinta District which had 703 (63.6%) term birth weight more than preterm low birth weight.
The same trend of term low birth weight more than preterm low birth weight was reported in another study by Lee et al. had highlighted that of the 18 million low-birth weight babies, worldwide; 59% were term-SGA. In another word it refers to term low birth weight infants and 41% were preterm.
There was another study revealed consistent trend of distribution too, that were two-thirds of SGA infants were born in Asia. LBW was largely attributed to intrauterine growth retardation in the developing countries from Asia, as compared to prematurity in developed and African countries.
Main findings
Univariates analysis showed a history of low birth weight (LBW) infant and primary education level of maternal were shown to be the most associated predictor for LBW; in this study. There is an association between the history of low birth weight infant and cases which are 2.91 times more likely to be exposed LBW as compared to controls’ in this study. There were many local studies which reported previous delivery of low birth weight infants as an important predictor. Similar result found in studies Boo et al, [12] study found that history of low birth weight infants was AOR:23 p=0.001, and Sutan et al., [13] elicited history low birth weight infants had AOR:37 p=0.045.
The previous history of low birth weight was associated with recurrent LBW in subsequent pregnancies was found in many numbers of studies carried in other countries. The studies which had consistent finding with this study were many; for example; Barua, Hazarika, & Dutta, 2014 [14] had reported a history of low birth weight are AOR; 5, p= 0.04 and Muchemi, Echoka & Makokh [15], found that history of low birth weight; AOR; 5.07, p=0.006.
A cohort design study by Sclowitz, et.al, [16] to identify prognostic factors associated with recurrence of low birth weight (LBW) in successive gestations at Pelotas, Brazil had recommended based on their finding to prevent recurrence of LBW are appropriate antenatal care and adequate maternal weight gain in pregnancy for high risk maternal. The history of previous delivery of low birth weight infant had been identified as one of the specific risk factor to provide pre pregnancy care as initiated by Malaysia‘s Ministry of Health in 3rd edition of Perinatal Care Manual published in 2013 [17]. The risk factor was recognised as need to acquire adequate pre pregnancy care.
Those maternal with previous history of delivering low birth weight infants will be usually tagged under green colour code: during antenatal care in the subsequent pregnancies; this as stipulated in the Perinatal Care Manual 3rd edition published in 2013. The green code denotes the care of the maternal will be under the Medical officer and nursing staff.
Generally, for maternal the pre pregnancy care in our country includes initial Pre pregnancy counselling is especially important for women who already have had a low birth weight delivery because the risk of repeating a poor outcome is high. Health care professionals should pay special attention to risk factor identification and reduction in these women [15]. However in our country managing the history of low birth in previous deliveries has no specific Standards Operating Procedure alike some risk factors such as recurrent abortions, history of unexplained perinatal death, history of congenital anomalies and also others too. Abusalah had recommended on developing follow up protocol and monitor progress in high risk pregnant women “Our preventive management policy is to identify these women from ANC, close follow up, educate and to avoid risks of LBW”.
Abusalah, IOM Washington D.C. & Sclowitz, [16-19] had recommended the needs to be strengthened and enforced in effort to reduce incidence of LBW infants through advocating the importance of pre-pregnancy screening, early antenatal booking and proper identification of high-risk maternal.
The maternal with primary education level had odds of 4.65 higher to the risk of having low birth infants compared to maternal who had the education level of secondary level and above. The meta analyses carried out by Silvestrin et al., [20] resulted in maternal with higher education having the protective factor. The other studies which conducted by Abdal Qader [21] and Sharma et al., [11] showed educational level as a significant predictor. Education is critical to social and economic development and has a profound impact on population health. Lack of education, for example, can lead to reduced ability to find, understand and use health information. Thus, education is an important determinant of health status.
Well educated individuals experience better health than the poorly educated, as indicated by high levels of self-reported health and physical functioning and low levels of morbidity, mortality, and disability. In contrast, low educational attainment is associated with “high rates of infectious disease, many chronic non infectious diseases, self-reported poor health, shorter survival when sick, and shorter life expectancy” [22].
Furthermore, this study also provided the opportunity to test two hypotheses. The first hypothesis was maternal age have correlations with the probability to deliver infants with low birth weight. This study found there are no correlation maternal age and the probability to deliver low birth weight infants. Adamson, Harold [23], found that no significant association between age of maternal with LBW as similar with this study.
The maternal from this study were largely from 18 to 35 years; there was an insufficient number to conclude if age below 18 years or 35 and above years as variables to leading to low birth weight infants. It is unlike the large population study carried out by Karalasingam et al., [24] for two years from 2011 until 2012, locally highlighted maternal for age 10 to 19 years of 260,959 maternal were significant. In another study by Yadav & Lee [25] found that maternal with aged 35 and above had a significant association with low birth weight infants.
The second hypothesis was maternal with anaemia are more likely to have low birth weight (LBW) compared to non-anaemic maternal; however, this was not significant in this study. Srinivas & Srinivasan [26], found that no significant association between maternal anaemia & low birth weight.
Conclusion and Recommendation
This study highlighted that the history of low birth weight and primary level of education being the strong determinants. This definitely open avenue for areas to explore such as; what are actually the causes which increase the risk to incur in a subsequent pregnancy, how to prevent and control that definite cause and what are strategies or best approaches.
The identification of factors involved in the repetition of LBW is an attempt to understand the causal links that increase the chance of some women to be more susceptible to give birth to a LBW child. A longitudinal study should be done from the period prior to conception through pregnancy to after deliver.' to allow for a close follow-up of the subjects and evaluate the factors contributing to low birth weight in a cause-effect model for development of specific interventions.
Awareness of the importance of education might help drive investment in education and improvements in education and educational policy. The education level of the maternal plays an important role in determining her own health and also the children, therefore multi-level interplay needed to ensure every woman empowered with the minimum secondary level should be mandated with evidence of further researches.
There is the need for a national study of sufficient sample size to be carried out in Malaysia as steps taken to address the risk factors associated with LBW infants near future, based on improved study design to confirm the findings in this study and explore further. No single approach will solve the low birth weight problem. Instead, several types of programs should be undertaken simultaneously. These range from specific medical procedures to broad-scale public health and educational efforts.
Summary
LBW would induce complications during infancy period and life course, prevention and control of its determinant factors should be considered in primary health care settings in order to improve maternal and child health.
References
- Badshah S, Mason L, McKelvie K, Payne R, Lisboa PJG (2008) Risk factors for low birthweight in the public-hospitals at Peshawar, NWFP-Pakistan. BMC Public Health 8:1-10.
- World Health Organization (2004) International statistical classification of diseases and related health problems, tenth revision, 2nd ed. World Health Organization.
- Patel P, Bavarva N, Patel M, Rana J, Mehta S, et al. (2015). Sociodemographic and Obstetrical Factors Associated with Low Birth Weight: Community Based Retrospective Study in an Urban Slum of Western India. App Medical Res 1:94.
- Vahdaninia M, Tavafian SS, Montazeri A. (2008). Correlates of low birth weight in term pregnancies: A retrospective study from Iran. BMC Preg Child 8:1–5.
- Cutland CL, Lackritz EM, Mallett-moore T, Bardajà A, Chandrasekaran R, et al. (2017). Low birth weight: Case definition & guidelines for data collection, analysis , and presentation of maternal immunization safety data. Vaccine 35:6492-6500.
- Khan MW, Arbab M, Murad M, Khan MB, Abdullah S (2014) Study of factors affecting and causing low birth weight. J Scientific Res 6:387-394.
- Risnes KR, Vatten LJ, Baker JL, Jameson K, Sovio U, et al. (2011). Birthweight and mortality in adulthood: A systematic review and meta-analysis. Int J Epidemiol 40:647–661.
- Kramer MS, Papageorghiou A, Culhane J, Bhutta Z, Goldenberg RL, et al. (2012). Challenges in defining and classifying the preterm birth syndrome. Am J Obst Gynecol 206:108-112.
- United Nations Children’s Fund and World Health Organization (2004) Low Birthweight: Country, regional and global estimates. Unicef.
- Sharma SR, Giri S, Timalsina U, Bhandari SS, Basyal B, et al. (2015). Low Birth Weight at Term and Its Determinants in a Tertiary Hospital of Nepal: A Case-Control Study. PLoS ONE 10:e0123962.
- Boo NY, Lim SM, Koh KT, Lau KF, Ravindran J (2008) Risk Factors Associated with Low Birth Weight Infants in the Malaysian Population. Med J Malaysia 63:306-310.
- Sutan R, Mohtar M, Mahat AN, Tamil AM (2014) Determinant of Low Birth Weight Infants: A Matched Case Control Study. Open Prev Med 4: 91-99.
- Barua A, Hazarika J, Dutta S (2014) Correlates of Low Birth Weight. Global Pediatric Health 1: 2333794.
- Muchemi OM, Echoka E, Makokha A. (2015). Factors associated with low birth weight among neonates born at Olkalou district hospital, central region, Kenya. Pan African Med J 20:1–11.
- Sclowitz KI, Santos T, Domingues IS, Matijasevich A (2013) Prognostic factors for low birthweight repetition in successive pregnancies: a cohort study.
- Division of Health Promotion and Diseases Prevention, Institute of Medicine Washington [DC] (1985). Preventing Low Birthweight. US.
- Silvestrin S, Silva CH, Hirakata VN, Goldani AA, Silveira PP, et al. (2013). Maternal education level and low birth weight: a meta-analysis. J Pediatr 89:339-340.
- Abdal Qader MA, Shah SA, Isa ZM, Ghazi HF, Badilla I, et al. (2014). Factors Related to Low Birth Weight Babies in Baghdad City, Iraq. Malaysian J Public Health Med 14:45-49.
- Feldman Jacob J, Diane M Makuc, Joel C Kleinman, Joan Cornoni-Huntley (1989) National Trends in Educational Differentials in Mortality. American J Epidemiol 129:919-33.
- Adamson B, Mohammed H (2007) Low birth weight in relation to maternal age and multiple pregnancies. Muhimbili National Hosp 14:55-58.
- Karalasingam SD, Jeganathan R, Muniswaran G (2012) Prevalence of Low Birth Weight babies among thepopulation from Malaysian tertiary hospitals : A cross sectional study. National Obstetrics Registry, Malaysia.
- Yadav H, Lee N (2013) Maternal factors in predicting low birth weight babies. Medical J Malaysia 68:44-47.
- Srinivas P, Srinivasan P. (2015). The Relationship between Maternal Anemia and Birth Weight in New Born. IOSR Dental Med Sci 14:2279-2861.
Citation: Ratnam S (2020) Maternal Risk Factors Associated with Term Low Birth Weight Infants at Government Health Clinics in Ipoh, Perak-A Case-Control Study. J Comm Pub Health Nursing 6: 247. DOI: 10.4172/2471-9846.1000247
Copyright: © 2020 Ratnam S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2750
- [From(publication date): 0-2020 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 1862
- PDF downloads: 888