Maternal and Neonatal Health in Select Districts of Iraq: Findings from a Recent Household Survey
Received: 21-Sep-2018 / Accepted Date: 17-Oct-2018 / Published Date: 24-Oct-2018 DOI: 10.4172/2376-127X.1000395
Keywords: Maternal health services; Postnatal care; Antenatal care services; Iraq; Newborn
Background
Women and children are disproportionately affected by conflict [1,2]. Instability due to conflict disrupts coverage of important Maternal, Newborn and Child Health (MNCH) services and undermines the health workforce capacity to respond to health needs [3,4]. A confluence of factors including infrastructural damage to health facilities, flight of the health workforce, interrupted access to essential information and social services, population displacement, and exposure to violence drive the increase in maternal, newborn and child deaths.
Iraq, at the time of survey is one of four countries classified as a system-wide level 3 emergency denoting the highest degree of severity of humanitarian conditions [5]. In 2014, a civil war broke out in Iraq between the Islamic State of Iraq and the Levant (ISIL) and Iraqi Armed Forces. Protracted conflict and resulting population displacement due to the armed conflict in Iraq have created considerable challenges for MNCH and have adversely affected health outcomes in this population.
Previous gains in reducing neonatal infant and child mortality rates have been slowed by years of war and the most recent conflict. Data published in UNICEF’s State of the World’s Children, 2012 reveals that 15% of newborn babies in Iraq have low birthweight, and neonatal mortality accounts for more than half the deaths of children under 5 years. In 2015, the maternal mortality ratio was estimated at 50 per 100,000 live births. Fertility rates are also high. From 1990 to 2010, the total fertility rate decreased from 6.1 to 4.7, but remained higher than other countries in the region. Access to reliable and updated data on MNCH indicators in Iraq remains limited, with the last Multiple Indicator Cluster Survey (MICS) having been conducted in 2011.
Here we present findings from a cross-sectional survey of 7182 households, which was conducted by the Central Statistics Organization under the Ministry of Planning in collaboration with the Ministry of Health and with technical support from UNICEF, in select districts in Iraq where the Iraq Every Newborn Action Plan will be implemented. The aim of the survey is to guide MNCH programmatic strategies and interventions in these districts. We present the results on key indicators concerning maternal and newborn health and highlight socioeconomic (SES) disparities.
Methods
Study design
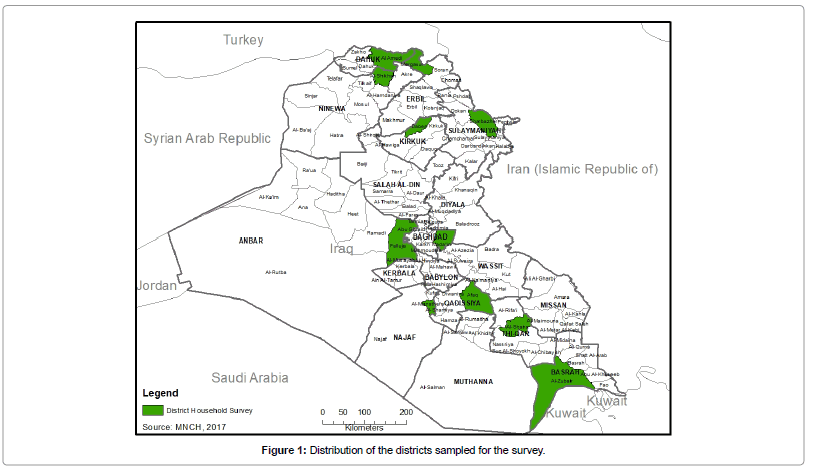
The present maternal, newborn and child health household survey used a household survey methodology. Data collection commenced in December 2016 and concluded in January 2017 in 12 selected districts where the Iraq Every Newborn Action Plan is to be implemented (Figure 1). The sample was designed to provide estimates on selected indicators about mothers and new born babies at the level of the district. A Two- Stage Cluster Sampling design was used for the sampling strategy. Within each stratum, 25 Blocks were selected as Primary Sampling Units (PSUs) systematically with probability proportional to size at first stage of sampling. Blocks covering at least 70-100 buildings/infrastructure sequentially numbered within the borders of mahalla/villages were considered as the PSU or the enumeration area. The “2009 Listing and Enumeration Frame” executed by the Central Statistical Organization was used as the sampling frame. After a household listing was carried out within the selected PSUs, a systematic sample of 24 households were drawn from each sample PSU as the secondary sampling units. Hence, a total of 600 households, selected from 25 clusters (24 households from each cluster), were planned as sample for each district. The final total sample size was 7200 households from 300 clusters. The sample was stratified by district, urban and rural areas, and is self-weighting within each district. However, for reporting the results both at district and aggregate level for the whole study area, sample weights are used.
Questionnaire
Three sets of questionnaire forms were used in the survey: 1) a household questionnaire, which was used to collect information on all de jure household members (usual residents), the household, and the dwelling, 2) a women's questionnaire administered in each household to all women who are married or ever married aged 15-49 years and 3) an under-5 questionnaire, administered to mothers or caregivers for all children under-5 years living in the household.
The questionnaires were based on the officially released MICS6 model questionnaire. They were translated into Arabic and Kurdish (both dialects) and back translation into English. The questionnaires were pre-tested in Karada, Baghdad and modifications were made for sequencing and appropriate wording to match the translation of the questionnaires.
Study teams
A total of 12 central supervisors were assigned per district. Three teams were allocated for each of the 12 districts (governorates) sampled. Each team consisted of 2 female physicians and one statistician. Female interviewers were assigned to ensure maximum participation of the respondents and were in charge of administering the women and children questionnaires, while the statistician established the contact with the household and identified all the household members. Moreover, the data collection process in each of these districts was supervised for quality and completeness by two senior doctors from the Directorate of Health (DOH) of the same governorate, two local supervisors and one statistical manager. All researchers and data collectors involved in the conduct of this study received a comprehensive training course in data collection.
Statistical analysis
All data analysis was completed using the statistical software SPSS version 17.0 and SAS 9.4 (SAS Institute; Cary, NC). We used frequencies for descriptive analysis, χ2 test for associations and logistic regression to identify significant predictors in multivariable analysis of antenatal care. Bivariate analysis using χ2 test was used to investigate the relationship between the independent variables and the categorical outcome variables, with detection of significant differences at p<0.10. Associations were estimated by odds ratios and their corresponding 95% CIs. For multivariable analysis, variables that had a P value less than 0.10 using the Chi-squared test were selected for inclusion in a multivariable model. Respondents were excluded if any data on the included predictors were missing.
Measures
Childhood mortality rates were calculated from information collected in the birth histories of the Women’s Questionnaires. All interviewed women were asked whether they had ever given birth, and if yes, they were asked to report the number of sons and daughters who live with them, the number who live elsewhere, and the number who have died. In addition, they were asked to provide a detailed birth history of live births of children in chronological order starting with the firstborn.
Antenatal care utilization was measured based on WHO recommendation of a minimum of four antenatal visits based on a review of the effectiveness of different models of antenatal care. ANC non-use was defined as zero ANC visits and adequacy of use was defined as at least four ANC visits.
Quality of ANC was defined based on WHO guidelines which require blood pressure measurement, urine testing and blood testing to be done during ANC visits. An additive index was created with responses concerning these three requirements, and was then dichotomized. Good quality care here indicates that the three elements were present during the ANC visit.
Essential Newborn Care (ENBC) includes the following, immediate drying, skin to skin contact of the newborn with the mother, clamping and cutting of the umbilical cord, early initiation of breastfeeding, and exclusive breastfeeding. In this study, early initiation of breastfeeding, commonly regarded as a tracer indicator for newborn care practices, is used along with skin to skin contact as proxy indicators for essential newborn care coverage.
Postnatal care for mothers and newborns was investigated by asking women age 15-49 with a birth in the two years preceding the survey whether they as well as their children received postnatal care within two days after birth.
Results
Sample characteristics
In total, 7182 households completed the survey accounting for 50,892 household members. Around 7274 women in child bearing age (15-49 years old) were listed in the households, of which 7222 women completed the survey-achieving a response rate of 99.3%. The response rates were slightly higher in rural (99.6%) compared to urban areas (99.1%).
Only 8.7% of households were headed by women and about 48.5% lived in urban areas. More than two-thirds (68%) of households had a family size of at least six members or more, reflecting the large family sizes in the study districts. The average household size is 6.6. Table 1 provides information on the background characteristics of female respondents 15-49 years of age (Table 1).
| % | Weighted N | |
|---|---|---|
| District (Governorate) | ||
| AL-Amadia (Duhuk) | 6.8 | 341 |
| Al-Shaikhan (Ninevah) | 8.3 | 419 |
| Sharbazir (Sulaimaniya) | 5.7 | 68 |
| Dibis (Kerkuk) | 7.1 | 211 |
| Meirkasoor (Erbil) | 6.8 | 154 |
| Al-Khalis (Diala) | 7.9 | 1043 |
| Amiryat alfaluja (Anbar) | 9.1 | 303 |
| Al-Madain (Baghdad) | 9.6 | 1317 |
| Al-Mishkhab (Najaf) | 9.8 | 387 |
| Afaq (Qadisiya) | 8.7 | 486 |
| Al-Shattra (Thi Qar) | 10.0 | 1050 |
| Al-Zubair (Basrah) | 10.3 | 1444 |
| Region | ||
| Kurdistan Region of Iraq districts | 7.8 | 563 |
| Other 9 districts of Iraq | 92.2 | 6659 |
| Area | ||
| Urban | 51.1 | 3688 |
| Rural | 48.9 | 3534 |
| Age in years | ||
| 15-19 | 6.5 | 469 |
| 20-24 | 14.8 | 1071 |
| 25-29 | 16.9 | 1223 |
| 30-34 | 17.7 | 1276 |
| 35-39 | 16.6 | 1200 |
| 40-44 | 15.2 | 1098 |
| 45-49 | 12.3 | 885 |
| Education | ||
| None | 20.8 | 1503 |
| Primary | 48.1 | 3473 |
| Intermediate/secondary | 23.7 | 1713 |
| Higher Education | 7.4 | 534 |
| Wealth index quintile | ||
| Poorest | 18.7 | 1351 |
| Second | 19.4 | 1404 |
| Middle | 20.3 | 1463 |
| Fourth | 20.7 | 1492 |
| Richest | 20.9 | 1513 |
| Total sample | 100.0 | 7222 |
*In this table and throughout the report, mother's education refers to educational attainment of mothers as well as caregivers of children under 5, if the mother is deceased or is living elsewhere.
Table 1: Frequency distribution of mothers aged 15-49 years of age by background characteristics.
Under-five, infant and neonatal mortality
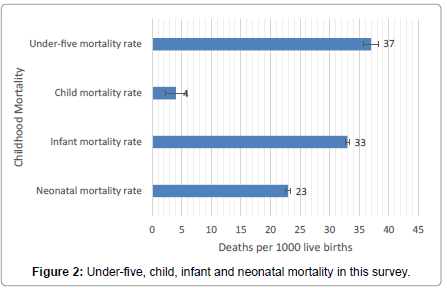
Neonatal, infant, child mortality and under-five mortality for the five years preceding the survey are presented in Figure 2. The overall under-five mortality rate in this sample was 37 per 1000 live births, while the neonatal mortality rate was 23 per 1000 live births, accounting for more than half of the under-five mortality rate (Figure 2).
The neonatal and overall under-five mortality rates were found to be lower in the Kurdistan Region of Iraq (16 and 24 deaths per 1000 live births respectively) compared to the nine Iraqi districts surveyed (23 and 28 deaths per 1000 live births respectively).
Prevalence of early child bearing
The survey aimed to identify the prevalence of adolescent childbearing. Table 2 shows the percentage of women age 15-24 years with early childbearing by their background characteristics. Overall, the proportion of teenage women (15-19 years of age) who had a live birth in Iraq was 54.5% and the proportion of those women who had a live birth before age 15 was 10.4. As for women age 20-24, 26.5% had a live birth before age 18 and 1.8% had a live birth before age 15. The higher prevalence of childbearing before the age of 15 among women aged 15-19 (10.4%) compared to women in the age group 20-24 (1.8%) may indicate that early childbearing is on the rise in Iraq aged 15-19 (10.4%) compared to women in the age group 20-24 (1.8%). may indicate that early childbearing is on the rise in Iraq (Table 2).
| Percentage of women age 15-19 years who: | Number of women age 15-19 years |
Percentage of women age 20-24 years who: | Number of women age 20-24 years |
||||
|---|---|---|---|---|---|---|---|
| Have had a live birth before age 18 | Have had a live birth before age 15 | Have had a live birth before age 18 | Have had a live birth before age 15 | ||||
| Region | Kurdistan districts | (56.5) | 0.0 | 14 | 12.7 | 2.8 | 42 |
| Other 9 districts of Iraq | 54.4 | 10.7 | 454 | 27.0 | 1.8 | 1029 | |
| Residence | Urban | 57.2 | 9.9 | 247 | 27.6 | 3.4 | 481 |
| Rural | 51.5 | 10.9 | 222 | 25.5 | 0.5 | 591 | |
| Education | None | 66.0 | 4.5 | 56 | 31.8 | 3.2 | 201 |
| Primary | 56.2 | 14.7 | 260 | 30.7 | 2.4 | 507 | |
| Intermediate/secondary | 47.9 | 5.4 | 149 | 21.1 | 0.2 | 300 | |
| Higher Education | (*) | (*) | 4 | 0.6 | 0.0 | 63 | |
| Wealth index quintile | Poorest | 70.1 | 28.6 | 67 | 29.4 | 2.4 | 187 |
| Second | 43.6 | 4.3 | 100 | 26.6 | 1.8 | 243 | |
| Middle | 57.3 | 7.1 | 106 | 25.1 | 0.9 | 224 | |
| Fourth | 52.2 | 7.5 | 82 | 29.3 | 1.8 | 198 | |
| Richest | 53.8 | 10.0 | 114 | 22.5 | 2.3 | 219 | |
| Total | 54.5 | 10.4 | 469 | 26.5 | 1.8 | 1071 | |
Note: *Figures that are based on less than 25 unweighted cases.
Table 2: Early childbearing among women age 15-19 and women age 20-24 years.
We found evidence for a significant relationship between adolescent childbearing and mother’s education (p value=0.064) and wealth quintile (p-value=0.017). The proportion of teenage women who had a live birth was highest among women with no education (66.0%) and those in the poorest quintile (70.1%) (Table 3).
| ANC Non-use | Quality of ANC | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | Adjusted OR (95% CI) | OR (95% CI) | Adjusted OR (95% CI) |
| Residence | ||||
| Urban | Reference | Reference | Reference | Reference |
| Rural | 1.63 (1.22-2.19) | 1.08 (0.76-1.54) | 0.64 (0.53-0.77) | 0.97 (0.77-1.22) |
| Age | ||||
| ≤ 19 years | 0.32 (0.15-0.65) | 0.34 (0.17-0.71) | 0.96 (0.67-1.40) | 0.91 (0.62-1.33) |
| 20-34 | 0.93 (0.64-1.37) | 0.96 (0.65-1.42) | 0.84 (0.64-1.11) | 0.82 (0.62-1.08) |
| 35-49 | Reference | Reference | Reference | Reference |
| Education | ||||
| None | 5.26 (2.14-12.99) | 4.31 (1.70-10.87) | 0.21 (0.12-0.37) | 0.29 (0.17-0.52) |
| Primary | 2.51 (1.02-6.17) | 2.36 (0.94-5.92) | 0.35 (0.20-0.61) | 0.43 (0.25-0.75) |
| Intermediate/Secondary | 1.28 (0.48-3.37) | 1.36 (0.51-3.62) | 0.48 (0.27-0.84) | 0.53 (0.30-0.94) |
| Higher Education | Reference | Reference | Reference | Reference |
| Wealth | ||||
| Poorest | 2.86 (1.81-4.50) | 1.80 (1.07-3.01) | 0.33 (0.24-0.46) | 0.44 (0.31-0.62) |
| Second | 1.47 (0.90-2.40) | 1.08 (0.62-1.86) | 0.43 (0.32-0.59) | 0.51 (0.36-0.72) |
| Middle | 1.30 (0.79-2.16) | 0.97 (0.55-1.69) | 0.64 (0.46-0.89) | 0.76 (0.53-1.09) |
| Fourth | 0.73 (0.41-1.29) | 0.58 (0.33-1.04) | 1.10 (0.77-1.58) | 1.23 (0.86-1.77) |
| Richest | Reference | Reference | Reference | Reference |
Table 3: Multivariable analysis. Predictors of ANC non-use and quality of ANC adjusting for residence, age, education and wealth.
Coverage of antenatal care, delivery and postnatal care for mothers and newborns
The survey also collected information on key areas in maternal and neonatal health. The information presented can be used to identify women who may be at risk due to non-use of health services and provide a basis for implementing appropriate interventions.
Antenatal Care (ANC)
Figure 3 shows the distribution of ANC non-use and adequacy of use-defined as at least four ANC visits-by selected respondents’ characteristics (Figure 3).
Overall, more than half of mothers received antenatal care at least four times (58.3%) and 8.7% did not make any ANC visits. Non-use of antenatal care varied across districts, with the highest rate of non-use in Fallujah district at 20% and the lowest rate at 3.8% in Meirkasoor (Erbil). Non-use was highest in rural areas compared to urban areas (crude OR=1.63, 95% CI=1.22-2.19), among women who had low educational attainment compared to women with higher education (crude OR=5.26, 95% CI=2.14-12.99), and women who belonged to the poorest wealth quintile compared to women in the richest wealth quintile (crude OR=2.86, 95% CI=1.81-4.50). Women in the age group 35-49 had higher rates of ANC non-use compared to women in the lowest age group (crude OR=3.13, 95% CI=1.54-6.67) (Table 3).
In logistic regression analysis, residence was no longer associated with ANC non-use (adjusted OR [aOR] 1.08, 95% CI, 0.76-1.54). However, educational attainment, wealth and mother’s age were associated with increased odds of ANC non-use (p-values<0.01). This indicates that the effect of urban/rural residence could possibly be explained by education and wealth since the significant association did not persist when adjusting for other variables (Table 3).
Additionally, quality of ANC was examined along with its association with selected sociodemographic variables. Table 3 shows that in rural areas, women were less likely to receive good quality ANC (crude OR=0.64, 95% CI=0.53-0.77) compared to their urban counterparts. However, the urban effect is likely explained by education and wealth since the significant association did not persist when adjusting for other variables. In multiple regression, there was a strong dose-response association between education and quality ANC. After adjusting for other variables, those with a higher education were 1.9, 2.3 and 3.4 times more likely to receive good quality ANC compared to those with secondary, primary or no education, respectively. Similarly, the poorest and second quintiles were less likely to receive good quality ANC compared to the richest quintile (Table 3).
Delivery by any skilled provider and essential newborn care (skin to skin contact and early initiation of breast feeding)
As for assistance during delivery, a high proportion (95.8%) of births occurring in the two years preceding the survey in the selected districts were assisted by skilled personnel. This estimate varied across districts, ranging between 89.7% in Kerkuk/Dibis and 100% in both Sulaimaniya/Sharbazir and Erbil/Meikasoor. Around 16.4% of live births took place at home, and home births were most prevalent in Alkhalis/Diala at 33.5%.
Overall, around 41% of mothers experienced Skin to Skin contact with their newborn immediately after birth. Table 4 demonstrates differentials in skin-to-skin contact by urban/rural residence, wealth and education level. Mothers delivering in urban areas were 1.27 times more likely to have experienced skin-to-skin contact compared to their rural counterparts (95% CI=1.04-1.55). Moreover, those belonging to the richest wealth quintile were 4 times more likely to have experienced skin-to-skin contact compared to the poorest wealth quintile, and 2.46, 2.4 and 1.56 times more likely to have experienced contact compared to the second, middle and fourth wealth quintiles. A somewhat similar pattern was observed for education (Table 4).
| Variable | Delivery assisted by any skilled attendant (%) | No. of women with Live Birth | OR (95% CI) | Early initiation of Breast feeding (%) | OR 95% CI) | Skin to Skin Contact (%) | No. of Women with Normal Delivery | OR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Residence | ||||||||
| Urban | 97.0 | 1186 | 1.84 (1.21-2.79) | 33.9 | 1.09 (0.92-1.30) | 43.7 | 787 | 1.27 (1.04-1.55) |
| Rural | 94.5 | 1143 | Reference | 31.9 | Reference | 37.9 | 844 | Reference |
| Education | ||||||||
| None | 93.5 | 598 | 0.13 (0.02-0.71) | 36.5 | 1.43 (0.97-2.10) | 34.6 | 451 | 0.47 (0.30-0.74) |
| Primary | 95.9 | 1036 | 0.21 (0.04-1.16) | 31.9 | 1.16 (0.80-1.68) | 42.9 | 735 | 0.67 (0.44-1.03) |
| Intermediate/Secondary | 97.0 | 541 | 0.29 (0.05-1.67) | 32.2 | 1.18 (0.80-1.74) | 40.9 | 350 | 0.62 (0.39-0.97) |
| Higher Education | 99.1 | 155 | Reference | 28.7 | Reference | 52.6 | 95 | Reference |
| Wealth | ||||||||
| Poorest | 91.0 | 448 | 0.05 (0.01-0.19) | 46.6 | 2.93 (2.20-3.90) | 26.3 | 354 | 0.25 (0.18-0.35) |
| Second | 95.3 | 482 | 0.09 (0.02-0.39) | 35.6 | 1.86 (1.39-2.47) | 36.8 | 342 | 0.41 (0.30-0.56) |
| Middle | 95.4 | 473 | 0.10 (0.02-0.39) | 35.8 | 1.87 (1.40-2.49) | 37.4 | 340 | 0.42 (0.30-0.57) |
| Fourth | 97.6 | 470 | 0.19 (0.04-0.81) | 24.0 | 1.06 (0.78-1.44) | 48.1 | 310 | 0.64 (0.46-0.89) |
| Richest | 99.5 | 457 | Reference | 23.0 | Reference | 58.9 | 285 | Reference |
Table 4: Bivariable analysis. Determinants of delivery assisted by skilled attendant, skin-to-skin contact and early initiation of breastfeeding.
Infant feeding practices were also examined. The proportion of newborns who were breastfed for the first time within one hour of birth was 33%. The top five fluids other than breast milk given to newborns in the first three days after birth were nothing (35.7%), sugar or glucose water (32.1%), tea/infusions/traditional herbal preparations (20.1%), infant formula milk (13.8%) and milk (11.0%).
In contrast to skin-to-skin contact, early initiation of breastfeeding did not demonstrate the same differentials by wealth or education. In fact, the reverse was true, wealth was negatively associated with breastfeeding and the poorest mothers were the most likely to initiate early breastfeeding compared to more affluent women. Education which is a proxy for wealth was similarly negatively associated with breastfeeding (Table 4).
Postnatal care for mothers and newborn
Proportion of women and children who received PNC varied by socioeconomic characteristics. In general, the proportion of women as well as children who received PNC after delivery was highest for urban compared to rural respondents, most educated vs least educated and among the rich and richest (Table 5).
| % of mothers receiving PNC | OR (95%CI) | % of new-borns receiving PNC | OR (95%CI) | ||
|---|---|---|---|---|---|
| Residence | Urban | 83.7 | 1.36 (1.11-1.68) | 83 | 1.47 (1.2-1.8) |
| Rural | 79 | Reference | 76.9 | Reference | |
| Education | None | 76.4 | Reference | 77.4 | Reference |
| Primary | 83.1 | 1.52 (1.19 - 1.95) | 81.3 | 1.27 (0.99-1.62) | |
| Secondary | 82.5 | 1.46 (1.1 - 1.95) | 77.9 | 1.03 0.78-1.36) | |
| Higher | 85.4 | 1.81 (1.11-2.93) | 89.2 | 2.41 (1.40-4.14) | |
| Wealth index | Poorest | 79.6 | Reference | 74.2 | Reference |
| second | 78.3 | 0.93 (0.67 - 1.27) | 75.1 | 1.049 (0.780-1.409) | |
| Middle | 81.1 | 1.10 (0.79 - 1.52) | 79.7 | 1.37 (1.00-1.858) | |
| Fourth | 84.1 | 1.36 (0.97 - 1.90) | 84.6 | 1.91 (1.38-2.65) | |
| Richest | 84 | 1.35 (0.96 - 1.89) | 86.4 | 2.21 (1.57-3.10) |
Table 5: Sociodemographic variables associated with PNC for mothers and for newborns.
Discussions
This household survey shed light on the status of important MNH indicators in select districts in Iraq where the implementation of the Iraq Every Newborn Action Plan is planned to take place. It highlighted important socioeconomic and geographic disparities that require tailoring planned interventions and strategies to target the most disadvantaged [6].
The first subsection provided information on levels of neonatal, infant and child mortality. Mortality rates among young children are the single most important indicator of child health in low- and middleincome countries [7]. The mortality rates revealed in these districts are much higher than the average child mortality rates in other Middle East and North African countries. Both the neonatal and under-five mortality rates calculated in this sample were higher than the most recent national morality estimates developed by the UN Inter-agency Group for Child Mortality Estimation which placed neonatal mortality in Iraq in 2015 at 18 deaths per 1000 livebirths and under-five mortality at 32 deaths per 1000 live births [8]. More than half of the under-five deaths in this sample were due to neonatal deaths, highlighting the need to direct special attention towards reducing neonatal mortality in Iraq. Further examination of the determinants of neonatal mortality in this context is needed to help policy makers and researchers develop efficient interventions and strategies to improve the survival of newborns.
Child mortality in the Kurdistan region was considerably less than that in other districts in Iraq in this sample. This is consistent with findings from the most recent MICS in which under-five mortality was estimated at 32 deaths per 1000 live births for the Kurdistan region and 38 for Iraqi districts [9]. However, while mortality rates were also lower for the Kurdistan region in the last MICS, the gap between the two regions has increased considerably in this survey as evidenced by the childhood mortality estimates presented earlier. This finding can be situated against a broader contextual backdrop. The health system of the Kurdistan autonomous region has been strained by a protracted humanitarian situation as well as several political and economic challenges, but it has concomitantly benefited from large health initiatives and reforms as well as a substantial infusion of humanitarian aid [10]. It is possible that such initiatives and reforms have contributed to the decline in childhood mortality.
We also found evidence of high rates of adolescent childbearing in the sampled districts. More than half of women aged 15-19 years of age had a live birth at the time of the survey and one tenth of these women had a live birth before age 15. Rates of early childbearing were most pronounced for lower income women and those with the least educational attainment. Early childbearing impacts morbidity, mortality and educational attainment and is accompanied by lifelong economic and social disadvantages for women [11,12]. Childbearing before the age of 16 is particularly problematic as it is accompanied by high rates of adverse clinical outcomes [13]. As such, this phenomenon demands that appropriate strategies and interventions be tailored to the most at-risk groups, especially in light of trends of increasing rates of early childbearing among younger generations of Iraqi women.
Findings pointed to a marked expansion in coverage of ANC in many of the surveyed districts. ANC care visits are an indicator of the extent to which women visit health care facilities to enable them to obtain proper care and understand the need for having skilled personnel at birth. Results show that non-use of ANC was overall low at 10% but reached a high of 20% in Fallujah, which is one of the cities most affected by armed conflict and Afaq district (19.3%). Despite the gains in expanding ANC coverage, large disparities exist in the utilization of ANC by women’s wealth, educational attainment and age. Similar disparities occur in the quality of ANC, which may be responsible for the abovementioned disparities in ANC utilization. Delivery care was promising with a high proportion (95.8%) of births assisted by skilled personnel. Home births however were not uncommon. The survey revealed that around 16.4% of live births took place at home and in some districts such as Alkhalis/Diala and Al-Mada’in/Baghdad, home births reached 33.5% and 30%. This is not surprising as both cities were heavily affected by violence and armed conflict, thereby potentially interrupting service coverage.
The survey also provided an update on the status of newborn care in Iraq. In fact, it was the first time in Iraq that a household survey was used to gauge respondents’ recollection of events around early postnatal care in addition to essential newborn care such as Skin to Skin contact with their newborn. In this sample, 44% of women experienced skin-to-skin contact and only 33% initiated early breastfeeding. Early initiation of breastfeeding is considered as the foremost indicator for essential newborn care coverage and the finding that only 1 in three women initiated breastfeeding within one hour of birth is cause for concern. Additionally, there was a negative association between early initiation of breastfeeding and SES variables, namely wealth and education. This relationship can be explained by the widespread use of infant formula by women belonging to higher SES, which due to the cost of infant formula makes it less accessible to poorer women and more within the reach of affluent women. Increased attention must be directed at addressing the problem of early initiation of breastfeeding given the strong association between early initiation of breastfeeding and neonatal mortality and particularly against a backdrop of high rates of neonatal mortality in Iraq [14].
In addition, the survey highlighted high rates of PNC coverage for mothers and newborns, at 81.4% and 80% respectively. Both time of birth and immediately after are a critical window of opportunity to deliver lifesaving interventions for both the mother and newborn. Global evidence for better maternal and newborn outcome have recently increased emphasis on the importance of post-natal care, recommending that all women and newborns receive a health check within two days of delivery. While PNC rates were high for newborns and mothers, there remain to be differentials in PNC coverage that disadvantage the poor, rural and uneducated.
This study has some limitations. First, some of the indicators presented relied on self-report without medical verification. For infant and child deaths for example, it is possible that there is under-reporting as is characteristic of retrospective self-reports. The period of recall, which is five years, may bear on the precision of the reporting. However, several studies have confirmed that women have good and precise recall of maternal events such as this [15-17]. In the measurement of quality of ANC, we relied on indicators that reflected service provision but that failed to capture the experiences of women with the health system. Patient experiences may be further driving the differentials in ANC use in this study sample.
Furthermore, cause of death was not recorded and thus patterns and trends in causes of childhood mortality were unexamined. These would have otherwise served to inform priority needs and necessary programmatic interventions.
Finally, another limitation of the study is that it is based on crosssectional data, precluding causal inference.
Conclusion
The MNCH survey data provides an in-depth and updated picture of the MNH situation in selected districts of Iraq. However, more thorough analysis of drivers of child and neonatal mortality is needed to elucidate drivers of the high under-five and neonatal deaths in Iraq. Further investigation of ANC practices is also needed to understand reasons behind the noted disparities in ANC utilization. Examining the experiences of Iraqi women with the health system is a crucial first step in diagnosing the problem.
Overall, the survey findings underscore the need for tailored strategies and interventions that focus on rural, uneducated and poor women who constitute the most vulnerable segments of the Iraqi population. Considering the disparities in ANC, the study findings would help design targeted strategies to narrow the equity gap for ANC coverage in Iraq.
Acknowledgments
Authors are grateful to the members of the National Technical Steering Committee for approving and overseeing the implementation of the study, Debra Jackson for reviewing as internal peer, Robert Cisoko for the map and to UNICEF Iraq for providing the technical and financial support.
References
- Bhutta ZA, Black RE (2013) Global maternal, newborn and child health-so near and yet so far. N Engl J Med 369: 2226-2235.
- Southall D (2011) Armed conflict women and girls who are pregnant, infants and children, a neglected public health challenge. What can health professionals do? Early Hum Dev 87: 735-742.
- Giacaman R, Wick L, Abdul-Rahim H, Wick L (2005) The politics of childbirth in the context of conflict: Policies or de facto practices? Health Policy 72: 129-139.
- Teela KC, Mullany LC, Lee CI, Poh E, Paw P, et al. (2009) Community-based delivery of maternal care in conflict-affected areas of eastern Burma: Perspectives from lay maternal health workers. Soc Sci Med 68: 1332-1340.
- Inter-Agency Standing Committee (2012) Humanitarian system-wide emergency activation: Definition and procedures-IASC transformative agenda reference document.
- Hilfi TK, Lafta R, Burnham G (2013) Health services in Iraq. Lancet 381: 939-948.
- Liu L, Hill K, Oza S, Hogan D, Chu Y, et al. (2016) Levels and causes of mortality under age five years. In:Â Black RE, Laxminarayan R, Temmerman M, Walker N (Eds), Disease control priorities, 3rd edition. Reproductive, maternal, newborn and child health, 2: 71-83.
- United Nations Children's Fund (2015) Levels and trends in child mortality. Estimates developed by the UN inter-agency group for child mortality estimation. New York, USA: UNICEF.
- The Central Statistics Organization, Kurdistan Regional Statistics Office (2012) Iraq multiple indicator cluster survey 2011, Final Report. Baghdad, Iraq.
- Shukor AR, Klazinga NS, Kringos DS (2017) Primary care in an unstable security, humanitarian, economic and political context: The Kurdistan region of Iraq. BMC Health Serv Res 17: 592.
- Stevens JH (1980) The consequences of early childbearing. Young Child 35: 47-55.
- Decker MR, Kalamar A, Tunçalp O, Hindin MJ (2017) Early adolescent childbearing in low and middle-income countries: Associations with income inequity, human development and gender equality. Health Policy Plan 32: 277-282.
- Phipps MG, Sowers M (2002) Defining early adolescent childbearing. Am J Public Health Res 92: 125-128.
- Khan J, Vesel L, Bahl R, Martines JC (2015) Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: Effects on neonatal mortality and morbidity: A systematic review and meta-analysis. Matern Child Health J 19: 468-479
- Olson JE, Shu XO, Ross JA, Pendergrass T, Robison LL (1997) Medical record validation of maternally reported birth characteristics and pregnancy-related events: A report from the children's cancer group. Am J Epidemiol 145: 58-67.
- Tilley BC, Barnes AB, Bergstralh E, Labarthe D, Noller KL, et al. (1985) A comparison of pregnancy history recall and medical records. Implications for retrospective studies. Am J Epidemiol 121: 269-281.
- Tomeo CA, Rich-Edwards JW, Michels KB, Berkey CS, Hunter DJ, et al. (1999) Reproducibility and validity of maternal recall of pregnancy-related events. Epidemiology 10: 774-777.
Citation: Moazzem Hossain SM, Ibrahim S, Al-Harun A, Muhammad S, Oudah K, et al. (2018) Maternal and Neonatal Health in Select Districts of Iraq: Findings from a Recent Household Survey. J Preg Child Health 5: 395. DOI: 10.4172/2376-127X.1000395
Copyright: © 2018 Moazzem Hossain SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3708
- [From(publication date): 0-2018 - Dec 18, 2024]
- Breakdown by view type
- HTML page views: 3044
- PDF downloads: 664